The Use of AI to Reduce Cardiogenic Shock in Post-Op Cardiac Surgery Patients
Written Summary
The assignment aimed to evaluate the effectiveness of bringing in artificial intelligence (AI) in decreasing the incidence of cardiogenic shock in patients who have been operated on for cardiac ailments. Cardiogenic shock is a combinative form of shock, and this makes its prognosis poor and is an important cause of mortality among these patients. Since it has been observed that AI can come up with prospective treatments for a number of forms of cardiovascular diseases, it became a question of whether it can also intervene to halt a case of cardiogenic shock among patients undergoing heart operations.
Search Strategy
The sources that were employed in the search for articles with data on the use of AI in identifying cardiogenic shock in postoperative cardiac surgery patients consisted of two databases: PubMed and CINAHL. Thus, the search approach was used in order to obtain articles that discuss the application of AI or machine learning in the prediction of certain outcomes, for example, cardiogenic shock in patients who endured cardiac surgery (Leivaditis et al., 2025). The adopted keywords for the study were artificial intelligence, cardiogenic shock, postoperative cardiac surgery, machine learning, and heart surgery complications. These terms were combined with the Boolean operators such as ‘AND’ and ‘OR’ to increase the extent of searching since there are many other related areas of study concerning the subject.
Further refinement was done to include articles published in the last five years only, clinical trials and randomized control trials, cohort and quantitative type of studies. Moreover, studies done as systematic reviews, meta-analyses, or non-scientific articles were not considered. The articles identified from these databases totaled 260 articles at first. After applying the filters to the articles and going through the abstracts, the articles that were selected for further evaluation were 26. Four articles were included primarily because they met the criteria of focusing on the aspects related to the PICO(T) question and were scientifically sound.
Description of the Studies and Search Results
These studies were chosen according to their design, relation to the clinical question, and methodological quality of the studies. Of the total 26 articles that underwent a qualitative assessment and summary, some study types addressed were randomized controlled trials, cohort studies, and even observational studies. Still, some of the publications were eliminated as they were not related to cardiac surgery patients and discussed other patient populations or presented theoretical aspects regarding AI implementation without reporting clinical results. These studies were also, many times, broad, not targeted toward identifying outcomes that are relevant to the prediction of cardiogenic shock or other post-surgery complications.
Four articles were reviewed for this assignment as these studies precisely assess the use of AI in advanced cardiac surgery scenarios, including the prediction of cardiogenic shock or better outcomes for risk factors patients. These comprised both cohort studies and RCTs, inclusive of machine learning and algorithms in conjunction with predictive modeling.
Overview of Studies
The first article looked at the development of a machine learning method based on statistical learning models for the prediction of major adverse cardiovascular events in patients with percutaneous coronary intervention (PCI). Despite the fact that this study used STEMI patients instead of postoperative cardiac surgery patients, its approach to the use of AI methods to predict adverse cardiovascular events can be used. It highlighted that the models created by AI could accurately predict the likelihood of extensive cardiovascular complications that can be used mainly in post-surgical cases requiring consistent monitoring for early identification, which is necessary in cases where cardiogenic shock may occur (Chen et al., 2025).
The analysis of the literature reveals AI’s utility in the population, especially in the identification of cardiovascular complications and their risk assessment. The study demonstrated that AI was capable of identifying the risk of cardiovascular events for patients with PCI, and the same study model could be used to address patients with cardiogenic shock after cardiac surgery. Although it does not explicitly relate to cardiogenic shock, the study generalizes the use of AI in cardiology (Chen et al., 2025).
In the work of Bohm et al. (2022), a retrospective cohort study was designed to derive machine learning models for cardiogenic shock (CS) in acute coronary syndrome (ACS). They used information derived from data from more than 40,000 patients undergoing cardiac catheterization after excluding those with CS at the time of admission. The last group included 3,232 patients who did not get complications and 176 patients who developed CS. Among the clinical measurements, age, heart rate, mean arterial pressure, respiratory rate, oxygen flow, peripheral oxygen saturation, blood glucose, type of pain, heart rhythm, and ectopy rate were input variables. Seven machine techniques were used in this study, with Logistic Regression Classifier and Gaussian Process Classifier using RBF (Radial Base Function) as the most effective methods.
These studies emphasize the application of the machine learning model in the early detection of CS among patients with ACS using clinical parameters. Due to the results obtained, it can be stated that early identification of such patients can help increase the number of positive results of the treatments. However, new developments of these models require additional improvement and independent testing to improve their accuracy and best fit for clinical use.
The third article was directly related to the ability to predict post-cardiotomy cardiogenic shock among high-risk cardiac surgical patients. This cohort study aimed at determining the multivariable predictors of cardiogenic shock post-surgery with the help of ML algorithms. The study further showed that the AI models could identify which patient is at higher risk, thus facilitating early intervention. It is pertinent to the formulated PICO(T) question as the study directly looks at the impact of AI in avoiding or lessening the chances of developing cardiogenic shock in postoperative cardiac surgery patients (Soltesz et al., 2024). This study was most applicable to the PICO(T) question because it demonstrated how AI can forecast cardiogenic shock in patients undergoing high-risk cardiac surgery, giving accurate prognosis to the proposition that, in postoperative care, AI can lower mortality and strengthen patient results (Soltesz et al., 2024).
The fourth article by Jajcay et al. (2023) employed a retrospective cohort analysis with the prepared machine learning model to identify factors associated with CS in patients with ACS. About their methods, they utilized the MIMIC III database to establish a data processing pipeline with an emphasis on imputing the missing data. After data preprocessing, the best result was obtained with the gradient-boosted tree-based classification method, which gave the cross-validated mean AUC of 0.805. The goal of this work was to improve the prediction of CS using clinic features that can be accessed within electronic health records. This research is closely related to the formulated PICO(T) question as it examines the application of machine learning algorithms for the prediction of CS in patients diagnosed with ACS (population of interest). As for the study data, the use of MIMIC III for data processing is relevant to the clinical issue of identifying cardiogenic shock in high-risk patients and recognizing the necessity of early management by creating more feasible risk stratification approaches in clinical practice.
Evidence Review Table (ERT)
| Evaluation criteria | Evaluation | |
| Citation & hyperlink | Bohm, A., Jajcay, N., Jankova, J., Petrikova, K., & Bezak, B. (2022). Artificial intelligence model for prediction of cardiogenic shock in patients with acute coronary syndrome. European Heart Journal Acute Cardiovascular Care, 11(Supplement_1). https://doi.org/10.1093/ehjacc/zuac041.077 | |
| Study citation and hyperlink | Purpose/Hypothesis | Purpose: To develop a machine learning-based model for predicting the onset of cardiogenic shock (CS) in patients with acute coronary syndrome (ACS).
Hypothesis: Machine learning algorithms can effectively predict the development of CS in ACS patients using easily obtainable clinical variables. |
| Type of Evidence & Detailed Design | Study Design: Retrospective cohort study employing machine learning techniques to analyze clinical data.
Detailed Design: Data from over 40,000 patients in critical care units of the Beth Israel Deaconess Medical Center were analyzed. Patients with ACS undergoing cardiac catheterization were selected and divided into two groups based on the development of CS. Patients with CS at admission were excluded. The study population consisted of 3,056 patients who did not develop CS and 176 who did. Clinical variables such as age, heart rate, mean arterial pressure, respiratory rate, oxygen flow, peripheral oxygen saturation, blood glucose, pain type, heart rhythm, and ectopy frequency were selected as input features (Bohm et al., 2022). |
|
| Study Population Characteristics | Population: Patients with ACS undergoing cardiac catheterization.
Sample Size: 3,232 patients (3,056 without CS and 176 with CS). Inclusion Criteria: Patients diagnosed with ACS undergoing cardiac catheterization. Exclusion Criteria: Patients with CS at admission, cardiac arrest prior to admission, delayed percutaneous coronary intervention, conservative/pharmacological treatment strategy, unknown presentation, or symptom onset >24 hours before admission. |
|
| Intervention Procedures | Intervention: Application of machine learning algorithms to predict CS in ACS patients.
Delivery: Data analysis was performed retrospectively using the Beth Israel Deaconess Medical Center database. Duration: Data from patients admitted between 2001 and 2012 were analyzed. |
|
| Comparison Procedures | Comparison Group: Patients who did not develop CS during hospitalization.
Analysis: Comparison of clinical variables between patients who developed CS and those who did not, utilizing machine learning models |
|
| Primary Outcome/Measures (including tools and units) | Primary Outcome: Development of CS during hospitalization.
Outcome Measurement Tools: Clinical records from the Beth Israel Deaconess Medical Center database; outcomes measured as the occurrence of CS during hospitalization. |
|
| Key Findings | Results: Both Logistic Regression and Gaussian Process Classifier with RBF kernel demonstrated good discrimination in predicting CS, with AUCs of 0.76 ± 0.04 and 0.77 ± 0.03, respectively.
Statistical Significance: The models showed significant predictive performance, though specific p-values were not provided. Clinical Significance: Early identification of patients at risk for CS allows for timely interventions, potentially improving patient outcomes. |
|
| Limitations | Study Limitations: Retrospective design may introduce biases; reliance on a single-center dataset may limit generalizability.
Generalizability: Findings may not be applicable to populations outside the Beth Israel Deaconess Medical Center or patients with different demographics (Kim et al., 2024). |
|
| Level of Evidence & Rationale | Level 3. The study provides valuable insights into predictive modeling for CS in ACS patients, though the observational design limits causal inference. | |
| Evaluation criteria | Evaluation | |
| Citation & hyperlink | Chen, M., Sun, C., Yang, L., Zhang, T., Zhang, J., & Chen, C. (2025). Application of machine learning algorithms in predicting major adverse cardiovascular events after percutaneous coronary intervention in patients with new-onset ST-segment elevation myocardial infarction. Reviews in Cardiovascular Medicine, 26(2). https://doi.org/10.31083/rcm25758 | |
| Study citation and hyperlink | Purpose/Hypothesis | Purpose: To develop and validate predictive models for major adverse cardiovascular events (MACE) following percutaneous coronary intervention (PCI) in patients with new-onset ST-segment elevation myocardial infarction (STEMI) using machine learning algorithms.
Hypothesis: Machine learning models can accurately predict MACE risk in STEMI patients post-PCI, aiding in personalized risk assessment and improving clinical decision-making. |
| Type of Evidence & Detailed Design | Study Design: Quantitative, retrospective cohort study utilizing machine learning algorithms to predict MACE risk.
Detailed Design: Data from 250 STEMI patients who underwent PCI were retrospectively analyzed. To address the issue of having several essential features, the Boruta algorithm was adopted; four machine learning models were also applied in the prediction of the MACE risk among the patients: K-nearest neighbors (KNN), support vector machine (SVM), complement Naive Bayes (CNB); logistic regression. For the purpose of evaluating the models, the area under the curve (AUC), sensitivity, and specificity were employed. Thus, using SHAP analysis, the potential predictors were excluded, and to enhance risk differentiation, a nomogram was developed (Chen, Cheng et al., 2025). |
|
| Study Population Characteristics | Population: New STEMI patients who will undergo PCI.
Sample Size: 250 patients. Inclusion criteria: Patients presenting with new STEMI and who received PCI. Exclusion Criteria: Patients with incomplete clinical data or contraindications to PCI. |
|
| Intervention Procedures | Intervention: Considering the application of a machine learning technique to predict MACE risk after PCI.
Delivery: Retrospective analysis of clinical and laboratory data from patient records. Duration: The data was obtained from patients who were treated between the years 2015 and 2020. |
|
| Comparison Procedures | The study focused on evaluating the performance of machine learning models without a comparative group. | |
| Primary Outcome/Measures (including tools and units) | Primary Outcome: Incidence of major adverse cardiovascular events (MACE) post-PCI.
Outcome Measurement Tools: Clinical records and laboratory results; outcomes measured as the occurrence of MACE events (e.g., reinfarction, stroke, death) (Kumar et al., 2022). |
|
| Key Findings | The logistic regression model demonstrated the best performance with an AUC of 0.814 in training and 0.776 in validation datasets. Key predictors of MACE included Killip classification, Gensini score, blood urea nitrogen (BUN), heart rate (HR), creatinine (CR), glutamine transferase (GLT), and platelet count (PCT).
Statistical Significance: P-values for key predictors were less than 0.05, indicating statistical significance. Clinical Significance: The nomogram developed provides a practical tool for clinicians to assess individual MACE risk, supporting personalized patient management. |
|
| Limitations | Study Limitations: Single-center design, retrospective nature, and potential selection bias.
Generalizability: Findings may not be generalizable to populations outside the study setting. Data Limitations: Reliance on retrospective data may limit the ability to establish causal relationships. |
|
| Level of Evidence & Rationale | Level of Evidence: Level 3 (Cohort Study). The study’s retrospective design and use of cohort data provide valuable insights into predictive modeling but lack randomization, limiting the strength of causal inferences. | |
| Evaluation criteria | Evaluation | |
| Citation & hyperlink | Jajcay, N., Bezak, B., Segev, A., Matetzky, S., Jankova, J., Spartalis, M., Tahlawi, M. E., Guerra, F., Friebel, J., Thevathasan, T., Berta, I., Pölzl, L., Nägele, F., Pogran, E., Cader, F. A., Jarakovic, M., Gollmann-Tepeköylü, C., Kollarova, M., Petrikova, K., . . . Böhm, A. (2023). Data processing pipeline for cardiogenic shock prediction using machine learning. Frontiers in Cardiovascular Medicine, 10. https://doi.org/10.3389/fcvm.2023.1132680 | |
| Study citation and hyperlink | Purpose/Hypothesis | Purpose: This study aims at establishing a data pipeline consisting of machine learning algorithms for the early diagnosis of CS in patients with ACS and using the MIMIC III database.
The study hypothesizes that the design and completion of a rigorous data processing scheme coupled with appropriate imputation strategy and machine learning models can enable the prediction of CS in ACS patients to help intervene and enhance patient outcomes. |
| Type of Evidence & Detailed Design | Study Methods: The study involved a data-driven retrospective cohort with observation carried out with the help of patient data employed in machine learning analysis.
Data Sources: The study employed the MIMIC III database specific to the case of patients with ACS. Among the multivariate imputation techniques that were assessed and compared were k-nearest neighbor imputation, imputations based on singular value decomposition, and multiple imputations by chained equations (AUC) (Lou et al., 2024). |
|
| Study Population Characteristics | Population: Acute coronary syndrome under treatment in Intensive Cardiac Care Units.
Inclusion Criteria: All patients who have been diagnosed with acute coronary syndrome have information in the MIMIC III database. |
|
| Intervention Procedures | Intervention: Predicting CS in patients with ACS through the use of modern techniques in working with machine learning algorithms.
Delivery: Data analysis was done according to a retrospective view of the MIMIC III clinical database. Duration: Data from the patients admitted from the years 2001 to 2012 were considered for this study (Jajcay et al., 2023). |
|
| Comparison Procedures | Not applicable; the study focused on developing and validating a predictive model without direct comparisons. | |
| Primary Outcome/Measures (including tools and units) | Primary Outcome: Development of cardiogenic shock during hospitalization.
Outcomes measurements: Using notes from MIMIC III, the frequency of CS during hospital stay will be considered as the outcome. |
|
| Key Findings | Achievement: For CS prediction, using the pipeline based on successful imputation and machine learning modeling, the cross-validation mean of AUC was 0.805 without using hyperparameter optimization.
Based on the statistical analysis, it could be seen that the AUC gives a good discriminative power; however, calculated p-values are missing. Clinical relevance: The current pipeline using the proposed approach provides a method of identifying high-risk CS-ACS patients and can help in early diagnosis. |
|
| Limitations | Limitations of the study include the use of a retrospective study design, which can predispose the study to bias; the use of a single database may also limit the generalizability of the findings of the study.
Generalizability: The results may not reflect the broader population other than patients in the MIMIC III database or patients of different ages, genders, and races. They again come with several limitations, such as missing or inaccurate data in the database that may impact the model. |
|
| Level of Evidence & Rationale | Level 3. The study provides valuable insights into predictive modeling; the observational design limits causal inference. | |
| Evaluation criteria | Evaluation | |
| Citation & hyperlink | Soltesz, E. G., Parks, R. J., Jortberg, E. M., & Blackstone, E. H. (2024). Machine learning-derived multivariable predictors of postcardiotomy cardiogenic shock in high-risk cardiac surgery patients. JTCVS Open, 22, 272–285. https://doi.org/10.1016/j.xjon.2024.10.002 | |
| Study citation and hyperlink | Purpose/Hypothesis | Purpose: The study aimed at determining the validity of the machine learning-developed multivariable model for PCS in high-risk cardiac surgery patients.
Hypothesis: It is feasible to find combinations of preoperative, intraoperative, and postoperative variables likely to result in PCS among the highest-risk cardiac surgery patients. |
| Type of Evidence & Detailed Design | Study Design: This was a cross-sectional retrospective study in which the EHR data was used with a machine learning approach.
Detailed Design: In this study, original data from the EHR of patients who underwent cardiac surgery from 2010 to 2019 were retracted from a single center. In all, 150 patients developed PCS among a total of 1,500 patients. |
|
| Study Population Characteristics | Population: It included all adult patients (age ≥18 years) who had cardiac surgery at a tertiary medical center.
Sample Size: 1500 patients in three groups, and out of them, 10% of the patients developed PCS post-surgery. Inclusion Criteria: The patient’s age should be above 18 years, and the procedure should be either elective or emergency cardiac surgery. Exclusion Criteria: Patients who had an emergency surgical procedure, patients with a lack of essential data, and contraindications to cardiopulmonary bypass (Soltesz et al., 2024). |
|
| Intervention Procedures | Intervention: CABG, valve surgery, repair/replacement, and other routine cardiac surgical operations.
Delivery: Operations or interventions are carried out by qualified cardiac surgeons as per the procedures and policies of the institution. Duration: Patients’ data accrued from surgeries they underwent between the years 2010 and 2019. |
|
| Comparison Procedures | Comparison Group: Patients who did not develop PCS were used as this group.
Analysis: Perform a comparative study between PCS and non-PCS groups and apply univariate or multivariate machine learning algorithms. |
|
| Primary Outcome/Measures (including tools and units) | Primary Outcome: Development of post-cardiotomy cardiogenic shock within 30 days post-surgery.
Outcome Measurement Tools: Classification of PCs depends on certain clinical features such as hypotension that does not respond to an intravenous fluid challenge, the need for inotropic support, and end-organ dysfunction. |
|
| Key Findings | Results: Numerous and varied factors were deemed necessary for PCS outcomes by the machine learning models, such as preoperative renal dysfunction, intraoperative transfusions, and postoperative low cardiac output syndrome.
Statistical Significance: For the random forest, the AUC-ROC of 0.85 with a sensitivity of 80% and a specificity of 75% was observed for the prediction of PCS. Clinical Significance: The identification of high-risk PC patients enables practicing clinicians to follow up and manage such patients carefully in order to possibly reduce the prevalence and severity of PCS (Fan et al., 2021). |
|
| Limitations | Conducted on a limited number of patients from a single hospital, which restricts generalization of the results. The retrospective characteristic of the analysis is based on the quality of EHR data.
Generalizability: The results of this study would not reflect broader populations in other healthcare facilities or for patients receiving other forms of operations. |
|
| Level of Evidence & Rationale | Level 3 (Cohort Study). While the study provides valuable insights into PCS prediction, the observational design limits causal inference. | |
References
Bohm, A., Jajcay, N., Jankova, J., Petrikova, K., & Bezak, B. (2022). Artificial intelligence model for prediction of cardiogenic shock in patients with acute coronary syndrome. European Heart Journal Acute Cardiovascular Care, 11(Supplement_1). https://doi.org/10.1093/ehjacc/zuac041.077
Chen, M., Sun, C., Yang, L., Zhang, T., Zhang, J., & Chen, C. (2025). Application of machine learning algorithms in predicting major adverse cardiovascular events after percutaneous coronary intervention in patients with new-onset ST-segment elevation myocardial infarction. Reviews in Cardiovascular Medicine, 26(2). https://doi.org/10.31083/rcm25758
Fan, Y., Dong, J., Wu, Y., Shen, M., Zhu, S., He, X., Jiang, S., Shao, J., & Song, C. (2021). Development of machine learning models for mortality risk prediction after cardiac surgery. Cardiovascular Diagnosis and Therapy, 0(0). https://doi.org/10.21037/cdt-21-648
Jajcay, N., Bezak, B., Segev, A., Matetzky, S., Jankova, J., Spartalis, M., Tahlawi, M. E., Guerra, F., Friebel, J., Thevathasan, T., Berta, I., Pölzl, L., Nägele, F., Pogran, E., Cader, F. A., Jarakovic, M., Gollmann-Tepeköylü, C., Kollarova, M., Petrikova, K., . . . Böhm, A. (2023). Data processing pipeline for cardiogenic shock prediction using machine learning. Frontiers in Cardiovascular Medicine, 10. https://doi.org/10.3389/fcvm.2023.1132680
Kim, Y. R., Chung, S. W., Kim, M., Choi, W., Choi, J., Lee, D., Lee, H. C., & Shim, J. H. (2024). Limited generalizability of retrospective single-center cohort study in comparison to multicenter cohort study on prognosis of hepatocellular carcinoma. Journal of Hepatocellular Carcinoma, Volume 11, 1235–1249. https://doi.org/10.2147/jhc.s456093
Kumar, R., Shah, J. A., Solangi, B. A., Ammar, A., Kumar, M., Khan, N., Sial, J. A., Saghir, T., Qamar, N., & Karim, M. (2022). The burden of short-term major adverse cardiac events and its determinants after emergency percutaneous coronary revascularization: A prospective follow-up study. Journal of the Saudi Heart Association, 34(2), 100–109. https://doi.org/10.37616/2212-5043.1302
Leivaditis, V., Beltsios, E., Papatriantafyllou, A., Grapatsas, K., Mulita, F., Kontodimopoulos, N., Baikoussis, N. G., Tchabashvili, L., Tasios, K., Maroulis, I., Dahm, M., & Koletsis, E. (2025). Artificial intelligence in cardiac surgery: Transforming outcomes and shaping the future. Clinics and Practice, 15(1), 17. https://doi.org/10.3390/clinpract15010017
Lou, J., Xiang, Z., Zhu, X., Fan, Y., Song, J., Cui, S., Li, J., Jin, G., & Huang, N. (2024). A retrospective study utilized the MIMIC-IV database to explore the potential association between the triglyceride-glucose index and mortality in critically ill patients with sepsis. Scientific Reports, 14(1). https://doi.org/10.1038/s41598-024-75050-8
Soltesz, E. G., Parks, R. J., Jortberg, E. M., & Blackstone, E. H. (2024). Machine learning-derived multivariable predictors of postcardiotomy cardiogenic shock in high-risk cardiac surgery patients. JTCVS Open, 22, 272–285. https://doi.org/10.1016/j.xjon.2024.10.002
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
The Use of AI to Reduce Cardiogenic Shock in Post-Op Cardiac Surgery Patients
Systematically retrieving and critically appraising research evidence relevant to the clinical question.
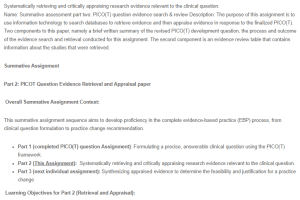
Name: Summative assessment part two: PICO(T) question evidence search & review Description: The purpose of this assignment is to use information technology to search databases to retrieve evidence and then appraise evidence in response to the finalized PICO(T). Two components to this paper, namely a brief written summary of the revised PICO(T) development question, the process and outcome of the evidence search and retrieval conducted for this assignment. The second component is an evidence review table that contains information about the studies that were retrieved.
The Use of AI to Reduce Cardiogenic Shock in Post-Op Cardiac Surgery Patients
Summative Assignment
Part 2: PICOT Question Evidence Retrieval and Appraisal paper
Overall Summative Assignment Context:
This summative assignment sequence aims to develop proficiency in the complete evidence-based practice (EBP) process, from clinical question formulation to practice change recommendation.
- Part 1 (completed PICO(T) question Assignment): Formulating a precise, answerable clinical question using the PICO(T) framework.
- Part 2 (This Assignment): Systematically retrieving and critically appraising research evidence relevant to the clinical question.
- Part 3 (next individual assignment): Synthesizing appraised evidence to determine the feasibility and justification for a practice change.
Learning Objectives for Part 2 (Retrieval and Appraisal):
Upon successful completion of this assignment, students will be able to:
- Execute a Systematic Search Strategy:
- Employ appropriate databases and search terms to conduct a comprehensive and reproducible search for relevant research evidence.
- Demonstrate proficiency in utilizing information technology to access and manage research literature.
- Critically Appraise Research Evidence:
- Apply established appraisal tools and criteria to evaluate the validity, reliability, and applicability of research studies.
- Differentiate between various research designs and their respective strengths and limitations.
- Assess the quality and level of evidence presented in research studies.
- Synthesize and Present Appraised Findings:
- Summarize the search strategy and selection process in a clear and concise manner.
- Organize and present appraised evidence in a structured format, such as an Evidence Review Table (ERT).
- Articulate the key findings and limitations of the appraised research.
- Integrate with the EBP Process:
- Connect the appraisal process to the previously developed PICO(T) question.
- Prepare the appraised evidence for subsequent synthesis and application in Part 3 of the summative assignment.
- Understand how this stage of the EBP process facilitates the decision making process for clinical changes.
Evidence Retrieval and Appraisal
Building upon the foundational PICO(T) question, this phase precedes the final synthesis of evidence and the development of evidence-based practice recommendations. This assignment facilitates the transition from clinical question formulation to the evaluation of supporting research.
Steps:
- Retrieve Evidence:
- Use databases (PubMed, CINAHL, etc.) to search for studies relevant to your finalized PICOT question. (Ensure you’ve incorporated prior feedback. Contact your instructor if needed.)
- Use keywords from your PICOT question and filters (date, study type) to refine your search.
- Document your search including:
-
-
- Databases used.
-
-
-
- Keywords.
-
-
-
- Filters.
-
-
-
- Mesh terms.
-
-
-
- Number of results at each step.
-
-
- Select the four most relevant studies, prioritizing by strong study designs and findings pertinent to your question. Use the Appraisal Tool for Evaluating a Single Research Study provided. Attach the completed Appraisal Tool for each of the studies that are included in the assignment evidence review table
- Appraise Evidence:
Use the provided Study Appraisal Tool to evaluate each of the four selected studies.
-
- Answer all questions in the tool related to each study.
-
- Consider study design, sample size, methodology, bias, and clinical significance.
-
- Determine the level of evidence for each study (e.g., using the Oxford Centre for Evidence-Based Medicine hierarchy, or the Johns Hopkins research evidence appraisal tool rating level and quality of scientific research evidence).
-
- Enter your findings into the Evidence Review Table (ERT) template
- Written Summary (Max 3 pages):
Include your finalized PICOT question paper as the introduction – this will not be included in the page limit. Please use track changes to show the revisions that were made to the document. The following section of the assignment counts in the 3 page limit:
- Describe your search strategy (keywords, filters, mesh terms, databases, etc.).
- Summarize your search results (number of studies found).
- Provide a succinct but thorough overview of the types of studies identified, why some were excluded. Finally describe the studies that were included, their primary findings, and relevance to the clinical problem that you are addressing.
- Evidence Review Table (ERT):
-
- Complete the provided ERT template for the four appraised studies selected using a maximum of one page for each study.
- Accurately and succinctly enter the required information for each study into the table.
- Include hyperlinks to the full text of each study.
- Submit the revised PICO(T) with changes shown by using track changes, the 3 page max written summary and ERT as a single word document to the designated electronic submission portal for this assignment after submitting it for originality review. Because the document contains your original PICO(T) paper you can expect the report to show a very high percentage. Please check the report to make sure that you have not accidentally plagiarized other sources in the written summary and ERT.
