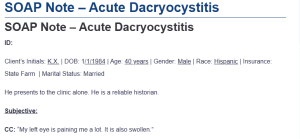
SOAP Note – Acute Dacryocystitis
ID:
Client’s Initials: K.X. | DOB: 1/1/1984 | Age: 40 years | Gender: Male | Race: Hispanic | Insurance: State Farm | Marital Status: Married
He presents to the clinic alone. He is a reliable historian.
Subjective:
CC: “My left eye is paining me a lot. It is also swollen.”
HPI:
A 40-year-old Hispanic male presented to the clinic with complaints of swelling and pain in the left eye. The symptoms began three days ago, are located in the inner corner of his left eye, and have been continuous since onset. He describes the pain as a throbbing pain that is aggravated by touch and is relieved slightly with over-the-counter pain medications. The pain has been constant for the past three days. The pain is accompanied by an increased tearing, a noticeable swelling, and a purulent discharge. The patient rates the pain as a 6/10 in severity.
Past Medical History:
- Medical problem list
- The patient has a negative history of physical and psychiatric illnesses. He has also never been involved in any accidents or had any head injuries.
- Surgeries: The patient has never had any eye or other surgeries before.
- Preventive Care:
- The patient had a dental checkup in March.
Allergies: No known food or drug allergies.
Medications:
- The patient is on an unknown over-the-counter analgesic medication.
Immunizations:
- The patient is current with all his vaccines. He recently received a booster shot of the Pfizer COVID-19 vaccine. He is scheduled to receive the influenza vaccine next week.
Social History:
- Chemical history: The patient has no history of taking alcohol. He, however, smokes occasionally.
- Sexual history: The patient is sexually active.
Other: The patient lives with his wife and two children. He works in a local company as a forklifter. He swims for fun, is physically active, and regularly goes jogging in the park. He sleeps 6-7 hours a day.
Safety:
- The patient owns a gun and keeps it in a locked cabinet. He wears a safety belt while driving and a helmet when performing outdoor activities.
Family History: No member of the patient’s family has been diagnosed with any chronic illness.
ROS:
- Constitutional: The patient reports experiencing fever and occasional chills. Denies any significant changes in his weight.
- Eyes: The patient reports blurred vision in his left eye. The visual functions in the right eye is intact. The left eye has been tearing significantly since the onset of the symptoms and is swollen. Denies any recent eye trauma, eye applications, or punctal plugs.
- Ears/Nose/Mouth/Throat: Denies hearing loss, tinnitus, or ear discharge. Denies nasal discharge, nasal congestion, or unusual sneezing. He also denies pain during swallowing, sore throat, or gum swelling.
- Cardiovascular: Denies chest pains, palpitations, irregular heart rate or rhythms, edema, or swelling in the extremities.
- Pulmonary: The patient denies wheezing, unusual coughs, or shortness of breath.
- Integumentary: Denies any skin color changes, scars, lesions, rashes, or any unusual pigmentation. He also denies excessive skin drying.
- Endocrine: Denies heat or cold intolerance or diabetes.
Objective
Vital signs: Blood Pressure: 121/81 mmHg [Normal: 90-120/60-80 mmHg]; Heart Rate: 81 beats per minute [Normal: 60-100 beats per minute]; Respiratory Rate: 17 breaths per minute [Normal: 12-20 breaths per minute]; Temperature: 99.2°F [Normal: 97.8-99.0°F]; Oxygen Saturation: 98% on room air [Normal: 95-100%]
Labs, radiology, or other pertinent studies:
Complete Blood Count for the Patient: This test was conducted to check for an underlying inflammatory process consistent with infectious illnesses. High WBC counts may signify the presence of an infection and thereby give insight into the likely diagnosis for the patient.
| Hematology | Result | Normal range |
| Red cell count | 5.4 x 1012/L | 4.5–5.7 |
| White cell count | 12.5 x 109/L | 4.0–10.0 |
| Hemoglobin | 159 g/L | 133–167 |
| Hematocrit | 0.51 | 0.35–0.53 |
| MCV | 83 fL | 77–98 |
| MCH | 29 pg | 26–33 |
| MCHC | 361 g/L | 330–370 |
| RDW | 11.5% | 10.3–15.3 |
Physical Exam
General Survey: The patient responds well to the interview questions and is cooperative. No signs of weight loss, fever, or chills.
- Head: The head is atraumatic and normocephalic. No sign of head scars, swelling, masses, abnormal hair thickening, or hair loss. The hair is well distributed on his scalp.
- Eyes: The eyes are symmetrical. The left eye is noticeably swollen and teary. There is a visible swelling in the medial canthus area. The medial canthus also appeared erythematous and tender. There is also a notable increase in the size of the tear meniscus. No sign of eye cataracts, corneal dystrophy, astigmatism, or retinal damage. Palpation of the medial canthus revealed that it was full. A purulent and tear reflux was also noted on massaging the lacrimal sac. The visual acuity was intact for the right eye. The visual acuity was, however, 10/20 for the left eye. The peripheral vision was intact bilaterally. No signs of diplopia.
- ENT: The ears are symmetrical. No signs of ear discharge, hearing loss, or use of hearing aids. The nose is symmetrical. No signs of erythema on the bridge of the nose. Also, no signs of nasal discharge, obstruction, or notable sneezing. The throat is clear. No signs of gum swelling or uvula deviation.
- Neck: The neck is symmetrical. The trachea is midline on the neck. No sign of swelling, lesions, skin color inconsistencies, or scars on the neck.
- CVS: The heart rate is rhythmic and regular. No pericardial friction sounds, gallops, or murmurs were heard on auscultation. The S1 and S2 sounds were, however, heard. Peripheral pulses were felt bilaterally. No sign of edema or cyanosis on the peripheries.
- Chest/Thorax: The chest is symmetrical. No sign of any chest wall deformities. No wheezing, rhonchi, or respiratory crackle sounds on auscultation. The apical pulse was felt on palpation.
- Integumentary: The skin was intact, dry, and warm to the touch. No signs of skin color inconsistencies, rashes, or lesions.
- Neurological: The patient is alert and oriented to the event and time. He also responds to the interview questions asked appropriately. His speech is logical and goal-directed, his judgment and thought processes are logical, and his memory is intact. Cranial nerves II- VII are intact.
Assessment
The case is of a 40-year-old male with a noticeable swelling in the left eye. He presents with complaints of pain. The medical canthus appeared tender, erythematous, and edematous. Purulent and tear reflux was noted on slight massage of the lacrimal sac. The patient also had a low-grade fever. These manifestations are suggestive of an eye infection.
Differential Diagnosis
- Acute dacrocystistis: Dacrocystistis is an inflammatory condition affecting the lacrimal sac. It is typically caused by an obstruction of the nasolacrimal duct, which results in the stagnation of tears in the lacrimal sac. It manifests clinically, upon lacrimal sac inflammation, as a swelling in the inferomedial canthus (Engelsberg & Sadlon, 2022). Dacryocystitis has a multifactoral etiology, with infectious agents, such as bacteria, eye application, and some ocular medications being implicated in its development. Dacrocystitis can be classified as either acute or chronic. Acute dacryocystitis is commonly attributed to infectious agents such as Staphylococcus and streptococcus variants, Haemophilus, and Pseudomonas (Chi et al., 2024). Patients with acute dacryocystitis will often present with complaints of pain and swelling in one or both eyes with an inset of a few hours or days. Assessment findings will reveal erythematous, edematous, and tender medial canthus. A purulent reflux on a slight massage of the medial canthus is often confirmatory of acute dacrocystis (Chi et al., 2024). The patient in the case presented had complaints of swelling and pain in the left eye. The complaints began three days before the clinic presentation. Assessment findings revealed an edematous, erythematous, and tender swelling in the medial canthus and a low-grade fever. This warranted the inclusion of this differential.
- Acute bacterial conjunctivitis: Bacterial conjunctivitis is an ophthalmological disorder characterized by eye redness. The redness can be accompanied by itching, pain, and discharge. The disorder results from eye contact with a fomite, respiratory droplets, and person-to-person transmission (Johnson et al., 2022). Staphylococcus variants and Hamephilus are the most commonly implicated pathogens in the development of bacterial conjunctivitis. Patients with acute bacterial conjunctivitis will often present with complaints of tearing, eye redness, eye itchiness or pain, and discharge from one or both eyes with an onset of less than three weeks (Johnson et al., 2022). Assessment findings often reveal vision loss, previous episodes, the presence of trauma, and the use of contact lenses. Fever is also apparent in the disease. A physical exam may be positive for a purulent discharge, conjunctival erythema, and reduced visual acuity (Chan et al., 2021). The presence of eye discharge, fever, and complaints of pain in the left eye in the case presented warranted the inclusion of this differential. However, a clear conjunctiva on an eye exam makes this diagnosis less probable.
- Preseptal Cellulitis:Preseptal cellulitis is a skin and soft tissue infection that primarily affects the tissues around the eye, specifically from the anterior to the orbital septum. It is caused primarily by sinusitis or trauma and predominantly affects children. The disease is attributed to infection spread from primary rhinosinusitis or infection from a traumatic injury to the eye. Patients with preseptal cellulitis will often manifest with periorbital erythema, eyelid swelling, periorbital edema, and visual loss. Assessment findings will sometimes reveal a history of trauma or sinusitis, decreased vision, and tearing. Fever is an uncommon finding in preseptal sinusitis (Vanga et al., 2023). The patient in the case presented had complaints of eye swelling and pain. Assessment findings were positive of decreased visual acuity on the left eye and tearing. This warranted the inclusion of this differential. Notwithstanding, the negative history of trauma and sinusitis, coupled with the presence of fever, makes this diagnosis less probable.
- Chalazion: Chalazion is an inflammatory condition of the eyelids. They manifest as slowly enlarging and non-tender lesions on the eyelid. Chalazia are typically benign but may develop chronic complications with resultant lid disfiguration. A chalazion can be caused by an inflammatory process and subsequent obstruction of the sebaceous gland. The chalazion may be painful and infected. Patients with a chalazion often present with complaints of eye swelling and pain. Physical examination may be positive for a non-tender, palpable, non-erythematous nodule in the eyelid. Visual loss is also apparent in the disease (Das & Dave, 2020). The patient in the case presented had eye pain and swelling, confirmed by a physical examination. This warranted the inclusion of this differential. However, the swelling in the patient’s case presented was tender and erythematous. This makes this diagnosis less probable.
Diagnosis: The presumptive diagnosis in the case presented is acute dacryocystitis. The manifestations of eye swelling and pain, along with the exam findings of fever, erythematous, edematous, and tender medial canthus, point toward this diagnosis. A purulent reflux on slight massage of the lacrimal sac gives a high suspicion of acute dacryocystitis. The absence of trauma and sinusitis or any other offending agent to the eye in the patient’s history, along with a clear conjunctiva, ruled out possible bacterial conjunctivitis. Fever and a negative history of trauma or sinusitis are also inconsistent, with preseptal cellulitis ruling out the diagnosis.
Plan:
Diagnostics
- Culture and gram staining will be ordered to identify the involved pathogen. The presence of fever in the patient’s case pointed toward the involvement of a bacterial pathogen. Culture and gram staining will help identify the likely bacteria and subsequently inform therapy. Culture and ram staining can be attained by obtaining the mucopurulent discharge expressed from the lacrimal sac (Engelsberg & Sadlon, 2022).
- A CT scan will be necessitated if orbital cellulitis is suspected. CT scans allow the visualization of an inflammatory process in the extraocular muscles (Zhang et al., 2019).
- In case of anatomical concerns, a dacryocystogram can be performed. A dacryocystogram can help ascertain the presence of blockage in the tear canals and subsequently inform therapy (Engelsberg & Sadlon, 2022).
Treatment
- The patient will be started on Crigler massage and warm compresses as a conservative measure against the disease. Crigler massage lowers the hydrostatic pressure from tear accumulation in the lacrimal sac. Conservative measures are the first line in managing acute dacryocystitis (Engelsberg & Sadlon, 2022).
- Oral antibiotics are considered when bacterial involvement is confirmed by culture. Cefalexin is considered the first line in the empiric therapy of acute dacryocystitis. The patient, in this case, will be started on cefalexin 500 mg administered every 12 hours for seven days. Antibiotic therapy maintains effectiveness in clearing the infection (Engelsberg & Sadlon, 2022).
- Topical antibiotics will be applied in case of acute flare-ups. Ocular gentamycin administered at one to two drops every four hours can help address flare-ups (Engelsberg & Sadlon, 2022).
Education
- The patient will be educated on the disease process. He will be informed that dacryocystitis is a disease that, if left untreated, can extend from the lacrimal sac to the surrounding orbital tissues. It is thus important to treat the disease (Engelsberg & Sadlon, 2022).
- The patient will also be educated on the significance of adhering to the prescribed therapy to ensure pain relief and clearing of the infection. In this respect, he will be advised against skipping doses. He will also be advised to report any side effects of the medication used. Cefalexin can sometimes cause GI disturbances. The patient should report to the clinic if he develops a rash, as this may be suggestive of a hypersensitivity reaction (Engelsberg & Sadlon, 2022).
Follow-up
- The patient will be advised to return to the clinic after one week. This will allow caregivers to assess whether the infection is cleared. He will also be advised to seek consultation whenever he develops untoward side effects (Engelsberg & Sadlon, 2022).
References
Chan, V. F., Yong, A. C., Azuara-Blanco, A., Gordon, I., Safi, S., Lingham, G., Evans, J., & Keel, S. (2021). A systematic review of Clinical Practice Guidelines for infectious and non-infectious conjunctivitis. Ophthalmic Epidemiology, 29(5), 473–482. https://doi.org/10.1080/09286586.2021.1971262
Chi, Y.-C., Lin, C.-C., & Chiu, T.-Y. (2024). Microbiology and antimicrobial susceptibility in adult dacryocystitis. Clinical Ophthalmology, Volume 18, 575–582. https://doi.org/10.2147/opth.s452707
Das, A. V., & Dave, T. V. (2020). Demography and clinical features of chalazion among patients seen at a multi-tier eye care network in India: An electronic medical records driven big data analysis report. Clinical Ophthalmology, Volume 14, 2163–2168. https://doi.org/10.2147/opth.s263146
Engelsberg, K., & Sadlon, M. (2022). First-onset dacryocystitis: Characterization, treatment, and prognosis. Ophthalmology and Therapy, 11(5), 1735–1741. https://doi.org/10.1007/s40123-022-00544-5
Johnson, D., Liu, D., & Simel, D. (2022). Does this patient with acute infectious conjunctivitis have a bacterial infection? JAMA, 327(22), 2231. https://doi.org/10.1001/jama.2022.7687
Vanga, S., Daniel, A. R., Gould, M. B., Ramlatchan, S. R., & Ganti, L. (2023). A diagnostic challenge: Periorbital or orbital cellulitis? Cureus. https://doi.org/10.7759/cureus.48439
Zhang, C., Cui, Y., Wu, Q., & Li, L. (2019). Computed tomography for guidance in the diagnosis and surgical correction of recurrent pediatric acute dacryocystitis. Pediatric Investigation, 3(1), 39–44. https://doi.org/10.1002/ped4.12115
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
SOAP NOTE Instructions
- Create a pretend SOAP NOTE on an adult about Acute dacryocystitis of the left eye (H04.301)
Some details I can share is below:
CHIEF COMPLAINT: “ I have swelling and pain near my left eye.”
KX, a 40-year-old Hispanic male, presents with symptoms that began suddenly three days ago. The swelling and pain are located at the inner corner of his left eye. These symptoms have persisted continuously over the past three days. The patient describes the pain as throbbing, with noticeable swelling and purulent discharge, along with increased tearing from the affected eye. The area is tender to touch, which aggravates the pain, but he denies any associated symptoms such as fever, vision changes, or recent trauma. Over-the-counter pain relief has provided minimal relief. The symptoms have been constant since their onset, and the patient rates the pain as 6/10 in severity.
DIFFERENTIAL DIAGNOSIS
- Acute bacterial conjunctivitis
- Preseptal Cellulitis
- Chalazion
MAIN DIAGNOSIS: Acute Dacryocystitis
SOAP Note – Acute Dacryocystitis
OTHER INSTRUCTIONS:
PLEASE FOLLOW THE TEMPLATE ATTACHED
PLEASE KINDLY USE THE INITIAL of patient ON THE HISTORY OF PRESENT ILLNESS SECTION ONLY AND THE REST. PLEASE USE the word “patient” instead of the initial B.D.
PLEASE MAKE SURE TO PUT THE APA 7 REFERENCES CORRECTLY. PLEASE PUT INTEXT CITATIONS ON PLANS AND TREATMENT
THIS IS A FOCUS SOAP NOTE SO PLEASE ONLY INCLUDE WHAT IS PERTINENT
PLEASE CHECK TO MAKE IT PLAGIARISM FREE
PLEASE USE THE TEMPLATE ATTACHED TO CREATE SOAP NOTE
PLEASE USE A TITLE PAGE AND DO NOT PUT THE LOGO OF THE SCHOOL
THANKS A LOT

