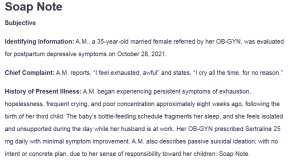
Soap Note
Subjective
Identifying Information: A.M., a 35-year-old married female referred by her OB-GYN, was evaluated for postpartum depressive symptoms on October 28, 2021.
Chief Complaint: A.M. reports, “I feel exhausted, awful” and states, “I cry all the time, for no reason.”
History of Present Illness: A.M. began experiencing persistent symptoms of exhaustion, hopelessness, frequent crying, and poor concentration approximately eight weeks ago, following the birth of her third child. The baby’s bottle-feeding schedule fragments her sleep, and she feels isolated and unsupported during the day while her husband is at work. Her OB-GYN prescribed Sertraline 25 mg daily with minimal symptom improvement. A.M. also describes passive suicidal ideation, with no intent or concrete plan, due to her sense of responsibility toward her children: Soap Note.
Past Psychiatric History: A.M. has no formal psychiatric history but did report transient depressive symptoms after previous pregnancies, which resolved independently within one month. Her family history includes a father who was hospitalized after a suicide attempt.
Psychosocial History: A.M. is currently on maternity leave from her job at State Farm Insurance. She has not resumed attending church since her baby’s birth, feeling fatigued and overwhelmed. Her support system includes her husband and sister-in-law, although she often feels isolated due to her family’s geographical distance.
Objective
Mental Status Exam:
- Appearance:M. is well-groomed, dressed casually, and appears her stated age. She avoids eye contact and appears tearful at times.
- Mood/Affect: Describes her mood as “exhausted”; affect is constricted but appropriate.
- Speech: Clear but slow and soft.
- Thought Process: Linear and goal-directed.
- Thought Content: There are no hallucinations or delusions; admits to brief, passive suicidal ideation without intent.
- Cognition:M. is alert and oriented to person, place, and time, with intact memory.
- Insight/Judgment: Shows knowledge about her symptoms and acknowledges the need for help. Her judgment is intact, given her commitment to her children.
Assessment
Primary Diagnosis: Major Depressive Disorder, Recurrent, Moderate, with Peripartum Onset (ICD-10 Code: F53.0)
Rationale: A.M. meets DSM-5-TR criteria for Major Depressive Disorder with Peripartum Onset, as she presents with persistent symptoms of low mood, fatigue, feelings of hopelessness, and suicidal ideation without intent (Marx et al., 2023). Her symptoms began shortly postpartum. She has a history of similar but transient postpartum depressive episodes, and her family history includes depression, further supporting this diagnosis.
Differential Diagnoses
- Adjustment Disorder with Depressed Mood (ICD-10 Code: F43.21):
- Rationale: Adjustment Disorder may be thought of as a result of the presence of emotional symptoms following a significant life event (birth of a child) (O’Donnell et al., 2020). However, Major Depressive Disorder with Peripartum Onset is a more appropriate diagnosis for A.M. because her symptoms are more severe and persistent than those of adjustment disorder.
- Persistent Depressive Disorder (Dysthymia) (ICD-10 Code: F34.1):
- Rationale: The hallmark of persistent depressive disorder is a protracted course of depression symptoms that lasts for at least two years, as noted by Patel and Rose (2023). A.M.’s symptoms have only been present for eight weeks postpartum and are acute rather than chronic, making this less likely.
- Bipolar II Disorder, Depressed Episode (ICD-10 Code: F31.81):
- Rationale: Although her depressive symptoms could overlap with Bipolar II Disorder, A.M. has no history of hypomanic or manic episodes, nor does she exhibit signs of mood instability that would suggest Bipolar Disorder (Jain & Mitra, 2023).
- Postpartum Psychosis (ICD-10 Code: F53.1):
- Rationale: Postpartum Psychosis can manifest within the first weeks postpartum with symptoms like delusions, hallucinations, and disorganized thinking, as indicated by Friedman et al. (2023). A.M. has no psychotic symptoms or impaired reality testing, so this diagnosis is unlikely. However, ongoing monitoring is necessary due to her passive suicidal ideation.
Plan
- Pharmacological Treatment:
- Medication: Continue Sertraline, increase to 50 mg daily as tolerated, and monitor for side effects and effectiveness.
- Rationale: Postpartum depression can be effectively treated with sertraline, which also helps with anhedonia and low mood symptoms. More therapeutic advantages might come from a higher dosage (Singh & Saadabadi, 2023).
- Non-Pharmacological Treatment:
- Therapy: Implement Cognitive Behavioral Therapy (CBT) to teach A.M. skills of overcoming negative thoughts, increasing coping skills as well as developing resilience.
- Rationale: In postpartum depression, CBT is indicated to address distortions in cognition, improve coping skills, and deal with hopelessness (Sp et al., 2020).
- Patient/Family Education:
- Postpartum depression education with an emphasis on compliance with treatment and possible good results due to support from the family.
- Rationale: Educating A.M. and her family can facilitate understanding and engagement, reduce stigma, and promote treatment adherence (Stewart & Vigod, 2019).
- Consultation/Referral:
- Refer to a psychiatrist for complete evaluation and follow-up, more so in view of a history of passive suicidal ideation.
- Rationale: Psychiatric referral ensures the patient receives specialty care in managing depressive symptoms and assessing continued risk (American Psychiatric Association, 2024).
- Follow-Up:
- Schedule a two-week follow-up appointment to assess response to medication adjustment, therapy progress, and changes in symptomatology.
- Rationale: Regular follow-up provides the chance for early intervention, should there be any increase in symptoms or side effects (Mackintosh et al., 2020), and it helps in keeping to the treatment plan.
References
American Psychiatric Association. (2024). Home │ psychiatry.org. Psychiatry.org. https://www.psychiatry.org/
Friedman, S. H., Reed, E., & Ross, N. E. (2023). Postpartum Psychosis. Current Psychiatry Reports, 25(2). https://doi.org/10.1007/s11920-022-01406-4
Jain, A., & Mitra, P. (2023). Bipolar disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK558998/
Mackintosh, N. J., Davis, R. E., Easter, A., Rayment-Jones, H., Sevdalis, N., Wilson, S., Adams, M., & Sandall, J. (2020). Interventions to Increase Patient and Family Involvement in Escalation of Care for Acute life-threatening Illness in Community Health and Hospital Settings. Cochrane Database of Systematic Reviews, 23(12). https://doi.org/10.1002/14651858.cd012829.pub2
Marx, W., Penninx, B. W. J. H., Solmi, M., Furukawa, T. A., Firth, J., Carvalho, A. F., & Berk, M. (2023). Major depressive disorder. Nature Reviews Disease Primers, 9(1). https://doi.org/10.1038/s41572-023-00454-1
O’Donnell, M. L., Agathos, J. A., Metcalf, O., Gibson, K., & Lau, W. (2020). Adjustment disorder: Current developments and future directions. International Journal of Environmental Research and Public Health, 16(14), 2537. https://doi.org/10.3390/ijerph16142537
Patel, R. K., & Rose, G. M. (2023, June 26). Persistent Depressive Disorder (Dysthymia). PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK541052/
Singh, H. K., & Saadabadi, A. (2023, February 13). Sertraline. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547689/
Sp, C., Dp, K., & Mr, H. (2020, January 1). Cognitive Behavior Therapy (CBT). PubMed. https://pubmed.ncbi.nlm.nih.gov/29261869/
Stewart, D. E., & Vigod, S. N. (2019). Postpartum Depression: Pathophysiology, Treatment, and Emerging Therapeutics. Annual Review of Medicine, 70(1), 183–196. https://doi.org/10.1146/annurev-med-041217-011106
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Details
Use the case study provided for this assignment.
You will come up with the most appropriate diagnosis (only one) and the full treatment plan on this patient.
Criteria
Diagnosis
Correct diagnosis with appropriate specifiers and ICD-10 codes. All rationale includes with appropriate citations.
Pharmacological with rationale
Medication(s) appropriate. All prescribing information is included and correct. Rational supports decision.
Non-Pharmacological with rationale
Includes all non-pharmacological treatment appropriate for this patient with rationale.
Patient/Family Education with rationale
Patient and/or family education appropriate for this patient and includes rationale.
Consultation/Referral with rationale
Includes any referrals appropriate for this patient and including rationale.
Soap Note
Follow-up with Rationale
Follow up appointment time appropriate for this patient.
References
Includes at least three scholarly references in this assignment.
Grammar
No more than two spelling and/or grammatical errors.
APA Format
No more than 2 APA formatting errors.

