Pericarditis
Pericarditis is the inflammation of the pericardial layer of the chest cavity. This disease is the most common type of pericardial disease. The inflammation caused by pericarditis often stimulates a stereotyped immune response that is characterized by chest pain that is always associated with peculiar electromagnetic changes that are accomplished by pleural effusion. Pericarditis can be either acute, ongoing, recurrent, or chronic. Compared with pericardial effusion and tamponade, acute pericarditis can be generally self-limiting and not life-threatening, with the possibility of causing significant disabilities. Acute pericarditis always has a high chance of reoccurrence compared to chronic pericarditis. Pericarditis is defined as recurrent when there is a relapse of the symptoms after a minimum symptom relief interval of 4-6 weeks. The symptoms relapse after 4-6 weeks of an acute episode of pericarditis, which is defined as incessant pericarditis (Imazio et al., 2015).
There is a lack of accurate epidemiological data for acute pericarditis. However, acute pericarditis is always diagnosed in 0.2% of all cardiovascular disease hospital admissions. Acute pericarditis also accounts for 5% of emergency admissions for chest pain in North America. Although the causes of pericarditis are unknown (idiopathic), pericarditis can always be caused by noninfectious causes such as trauma, autoimmune diseases, auto-inflammatory diseases, and cancers. It can also be caused by infectious agents such as bacteria, viruses, or fungi. The joint contagious agent of pericarditis is viral infections. Pericarditis can also be a secondary complication of diseases of the gastrointestinal system or condition of the respiratory system. The viral cause of pericarditis is always caused by flu-like syndrome. The most common agents include mycobacterium tuberculosis, borrelia burgdorferi, parvovirus B19, and Epstein-Barr virus. Infectious causes only account for 14%, while noninfectious reasons contribute to 55. 31% always occur due to post-cardiac injury syndrome such as heart surgery.
The features responsible for the pathophysiology of pericarditis include cardiac pressure transmission through the pericardium and heightened vesicular independence. Constrictive pericarditis always limits the diastolic filling and results in dissociation of intracardiac and intrathoracic pressure. This process is continually strengthened by ventricular freedom. This results in diastolic dysfunction, ventricular diastolic pressure elevation, respiration variation in ventricular felling, and reduced cardiac output. The pan cycle compression, the primary abnormality of the cardiac tamponade, causes an increase in pericardial fluids, thus causing competition of the cardiac chambers for the intrapericardial volume. This always explains the diagnostic findings of the Doppler echocardiography (Rehman et al., 2017).
The most common symptom of pericarditis is chest pain. Sharp or stabbing sensations always characterize the pain. However, some people report dull, achy, or pressure-like chest pain. The pain is usually felt at the sternum and on the left side of the chest. It can also refer to other body parts (referred pain), such as the left shoulder and neck. This pain is permanently aggravated by chest wall activities and movements such as coughing and taking deep breaths. The pain is always relieved by sitting up while leaning forward. Other clinical features of pericarditis are oedema, dry cough, low-grade fever, shortness of breath, palpitations, increased heart rates, fatigue, and general body weakness.
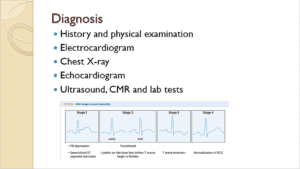
On physical examination, pericarditis patients are always uncomfortable and anxious and present with chest pain, tachycardia, palpitation, and low-grade fever; when the patient is leaning forward, pericardial friction rubs are always heard. Pericardial friction rubs are always caused by friction between two inflamed layers of the pericardium. However, when associated with systemic diseases, patients with pericarditis always present with additional symptoms such as loss of weight, skin rash, night sweats, and even arthritis. ECG is used to show the electrical activities of the heart. Sequential changes in electrocardiography are seen in 60% of patients because the parietal peritoneum is always silent. However, ECG always reports elevated ST segments with depressed PR segments. The ECG modifications can either be diffuse or localized with PR depression. Other diagnostic tests in pericarditis include an echocardiogram, chest X-ray, and ultrasound. A chest X-ray can clearly show fluid accumulation in the pericardium. Lab tests can also confirm the infectious agent—for example, CBC (Welch, 2018).
Cardiac magnetic resonance (CMR) can show different heart sequences. These findings can significantly help diagnose pericarditis, starting with assessing the morphological structure of the seat until the individuation of the area of active inflammation of the pericardium. This diagnostic tool can identify regions of LV hypertrophy that ECG does not readily recognize. The technique enhances the assessment of LV hypertrophy, specifically the anterolateral LV free wall (Kramer et al., 2020).
Mild cases of pericarditis always resolve on their own. Pericarditis can be managed conservatively by encouraging prolonged rest, minimizing physical activity, and advocating for a lifestyle change. The minimal recommended time for abstaining from physical activity is usually three months for patients who do not participate in sporting activities. The treatment of acute pericarditis should always be started immediately with aspirin and non-steroidal anti-inflammatory drugs NSAIDs with gastroprotection upon laboratory results findings (600-800 mg of ibuprofen three times a day administered orally). Colchicine therapy should only be used as an adjuvant to aspirin and a steroidal anti-inflammatory drug. If the patient presents with contraindications of aspirin and NSAIDS, a low dose of corticosteroids should be used. The corticosteroids can also be used when infections do not cause pericarditis, and there is a specific indication of autoimmune disease. The CRP should always guide the treatment length and response to therapy. The poor prognosis of acute pericarditis is always associated with the following risk factors: high fever, sub-acute cause, pericardial effusion, cardiac tamponade, and non-response to NSAIDs after several days of therapy. In severe cases, pericarditis can be treated surgically through pericardiocentesis to aspirate the fluid build-up and, through pericardectomy, the surgical removal of the pericardium (Welch, 2018).
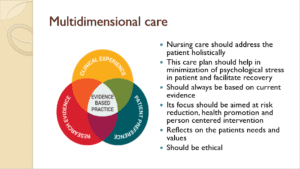
Prolonged hospitalization due to pericarditis and other chronic diseases always results in psychological difficulties for the patients. This, therefore, necessitate the need to configure patient care plan according to the patient’s needs and expectations rather than generalizing the needs of all the patients. To help develop a positive feeling and attitude among the patient, nurses must embrace multidimensional care. Multidimensional nursing care, therefore, provides nursing care to the patient to meet their needs holistically. This practice should address activities through which risks of developing pericarditis can be minimized/reduced, health promotion, and evidence-based nursing interventions. The critical component of nursing care is integrating nurses’ skills with the patient’s expectations and research evidence. Therefore, Evidence-based nursing care will enable the nurses to analyze the patient’s critical needs to guide the diagnosis of pericarditis and their plan for nursing interventions to address the identified needs. To facilitate the patient’s recovery, nurses should always be sensitive to the cultural and religious practices of the patients. Always have the patients at heart by doing good to the patients and avoiding harm (Schwier et al., 2020).
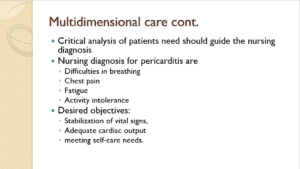
An accurate pericarditis nursing diagnosis depends on the nurses’ capability to critically analyze patients’ needs through a thorough physical examination. The nursing diagnosis for pericarditis patients is chest pain, fatigue, low-grade fever, activity intolerance, especially thoracic movements, and difficulty breathing in a severe case of pericarditis. Therefore, while formulating the nursing care plan, they should always be guided by the identified nursing diagnosis to meet their desired outcomes, such as stabilization of vital signs, adequate cardiac output pain management, and meeting the self-care needs of the patient.
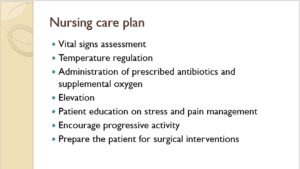
The nurse should continually assess and document the vital signs of the patient after every 4 hours. In addition to the vitals, always consider dehydration, cyanosis, pallor, oedema, and capillary refill. The nurses can regulate the patient’s temperature through regular baths, removal of excessive clothing, and administering fluids orally as can be tolerated by the patient. In cases where the cause of pericarditis was bacteria, always administer antibiotics as prescribed by the medical doctor. In addition to the antibiotics, nurses should always administer aspirins, NSAIDs, and corticosteroids as indicated. Oxygen supplements should always be issued when the saturation levels are low. Another critical aspect of the nursing care plan is patient education. Educate the patient on stress management by doing breathing and relaxation exercises, educate them on the importance of avoiding physical activities when diagnosed with pericarditis, and educate the patients on the risk factors of pericarditis and how to avoid them. Always elevate the head of the patient’s bed to ease the work of breathing. In cases where the infection is severe, always prepare the patient for the surgical procedure both mentally and physically. Ensure that the patient has enough knowledge of the surgical procedure by explaining to them the expected outcomes.
References
Imazio, M., Gaita, F., & LeWinter, M. (2015). Evaluation and treatment of pericarditis: a systematic review. Jama, 314(14), 1498-1506. https://jamanetwork.com/journals/jama/article-abstract/2456172
Rehman, K. A., Betancor, J., Xu, B., Kumar, A., Rivas, C. G., Sato, K., … & Klein, A. L. (2017). Uremic pericarditis, pericardial effusion, and constrictive pericarditis in end‐stage renal disease: Insights and pathophysiology. Clinical cardiology, 40(10), 839-846. https://heart.bmj.com/content/104/9/725.abstract
Kramer, C. M., Barkhausen, J., Bucciarelli-Ducci, C., Flamm, S. D., Kim, R. J., & Nagel, E. (2020). Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. Journal of Cardiovascular Magnetic Resonance, 22(1), 1-18. https://jcmr-online.biomedcentral.com/articles/10.1186/s12968-020-00607-1
Welch, T. D. (2018). Constrictive pericarditis: diagnosis, management and clinical outcomes. Heart, 104(9), 725-731. https://heart.bmj.com/content/104/9/725.abstract
Schwier, N. C., Cannedy, J. J., & Skrepnek, G. H. (2020). Management of Acute Idiopathic (Viral) Pericarditis in the Emergency Department: A Review for the Nursing Professional. Advanced Emergency Nursing Journal, 42(1), 17-29. https://cdn.journals.lww.com/aenjournal/Fulltext/2020/01000/Management_of_Acute_Idiopathic__Viral_.5.aspx
Chiabrando, J. G., Bonaventura, A., Vecchié, A., Wohlford, G. F., Mauro, A. G., Jordan, J. H., … & Abbate, A. (2020). Management of acute and recurrent pericarditis: JACC state-of-the-art review. Journal of the American College of Cardiology, 75(1), 76-92. https://www.jacc.org/doi/abs/10.1016/j.jacc.2019.11.021
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Competency
Pericarditis
Prioritize nursing care strategies for clients with cardiovascular disorders.
Scenario
Cardiac disease is one of the leading causes of death in the United States. Since it is so prevalent, you want to ensure your co-workers are fully prepared to care for patients. You are hosting a lunch to provide a refresher on heart disease and how to care for patients. During the lunch, you will present a PowerPoint Presentation to your co-workers.
Instructions
Please choose one of the cardiac diseases we covered in the last two modules. Within your presentation, include the following:
-
- Provide a detailed overview of the disease process
- Diagnosis
- Treatment
- Multidimensional care, including risk reduction, health promotion, and nursing interventions specific to the disease process
- Provide voiceovers for your PowerPoint presentation or presenter notes under each slide.
- The presentation should have a minimum of 10-12 slides, including a title and reference slides.
- Submit a Grammarly report with your presentation.