Elias Leon Case Study
Elias Leon, a 62-year-old male with a past medical history of hypertension, type 2 diabetes mellitus, and dyslipidemia, was diagnosed with acute ST-segment elevation myocardial infarction, abbreviated as STEMI, which is a result of a blockage in the left anterior descending (LAD) coronary artery. STEMI is a severe type of heart attack category that causes a prolonged duration of ischemia that leads to the lethal endpoint of irreversible myocardial injury if the affected flow territory is not reperfusion emergently. This paper presents Elias’s specific management plan based on research evidence and entails the importance of early intervention and team mechanization when dealing with acute coronary syndromes.
Diagnostic Tests
The management plan starts with diagnostic testing aimed at verifying the diagnosis, determining the severity of myocardial involvement, and a further treatment strategy. A styled electrocardiogram is indispensable when diagnosing STEMI because this method reveals ST segment elevation in certain leads, which indicates acute myocardial ischemia (Whalen et al., 2019). Continued cardiac enzyme levels, especially troponin will be done to show the extent of myocardial damage at different time points to help with risk assessments, as well as other management decisions in the future. Also, a chest X-ray shall be conducted to check for features of chronic lung congestion due to heart failure that may further endeavor the presentation of STEMI.
Medications
There is a need for early pharmacological intervention in patients with STEMI in a bid to suppress the myocardial oxygen demand, prevent the development of thrombus, and /or increase the perfusion in the affected vessels. Elias will be given aspirin 325 mg, chewed start, and later 81 mg once a day to reduce the formation of thrombi on the inner lining of the coronary arteries. Also, for antithrombotic prevention, clopidogrel 300 mg loading dose, then 75 mg daily maintenance will be given due to the history of recurrent thrombotic episodes (Maqsood et al., 2023). Nitroglycerin sublingual 0.4 mg will be prescribed for the management of persistent chest pain, which will be given every five minutes for up to three doses; however, close supervision of blood pressure will be made due to its vasodilatory effect. Oxygen therapy will be started at 2-4 liters per minute by nasal cannula to keep the patient’s arterial oxygen saturation over 94% required for myocardial oxygenation and tissue perfusion for the acute phase of myocardial infarction.
Suggested Consults/Referrals
Due to the specific management of Elias’s case and the need for team coordination, a referral to the cardiology service will be made whenever necessary. The cardiology team will then decide on the mode of revascularization based on the results of coronary angiography, which involves a detailed description of the degree and site of coronary artery occlusion that is either by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) (Simard et al., 2021). A pulmonology consult will also be ordered for the management of pulmonary congestion noted during the physical assessment examination to reduce the chances of coming across the several complications associated with the worsening of heart failure.
Patient Education
Teaching interventions will be implemented to educate Elias and his family on necessary information about his treatment regime. Further elaboration will be devoted to involving the patient in the process and stressing the issue of medication compliance, specifically nonsteroidal anti-inflammatory agents and antithrombotic agents such as aspirin and clopidogrel to reduce the risk of recurrent cardiovascular events (Huriani, 2019). The potential lifestyle modifications that will be conveyed to Elias will comprise smoking cessation, dietary restrictions recommended for diabetes and dyslipidemia, and exercise regimens within his cardiac condition, which is under evaluation. Detailed guidelines for identification of the signs of angina pectoris, worsening of dyspnea, or signs of decompensated heart failure will be given to the patient to receive adequate medical assistance and prevent potential complications.
Follow-up
To ensure proper assessment of Elias’s progress after early release from the hospital, a structured follow-up plan will be developed. He will be seen within the next 48 hours after discharge to determine compliance with treatment and behavior of cardiac enzyme and to check for such complications as arrhythmia or recurrent ischemic episodes (Marbach et al., 2020). Other indications for earlier re-evaluation will be explained to Elias as well as his family, and they will be advised to note the following: persistent chest pain, increasing dyspnea on rest or minimal exertion, or if Elias presents other symptoms that indicate cardiac decompensation.
Rationales
Every modification concerning Elias’s management plan will be chosen according to the latest available interventions, best practices, and evidence-based clinical protocols concerning STEMI. Aspirin and clopidogrel are to be given early to prevent further thrombus formation and decrease the possibility of myocardial ischemia as regards landmark trials with STEMI patients under DAPT (Passacquale et al., 2022). Nitroglycerin will be recommended because of its vasodilation properties, which will help manage spasms of the coronary arteries and diminished oxygen demand by the myocardial tissue on account of pain arising from myocardial infarction. Oxygen administration will be ordered to help meet tissue oxygen demands, which are vital for increasing flow through the myocardium in Elias’s compromised cardiovascular status.
In summary, as an acute STEMI patient, Elias Leon’s treatment required a quick and evidence-based decision-making process. The elaborate plan involved quick access to diagnostic tests, early prescription of medications to recanalize the blocked coronary artery, consultations from other specialists for more invasive procedures, health inculcation of the patient on the need to change lifestyle, and identifying symptoms of the disease, as well as providing structured follow-up to check on the patient’s progress and screen for possible complications. Through these strategies incorporating Elias’s medical history and current symptoms, this management plan sought to prevent further myocardial injury and promote proper healing without triggering a relapse of the cardiac event in the future.
References
Huriani, E. (2019). Myocardial infarction patients’ learning needs: Perceptions of patients, family members, and nurses. International Journal of Nursing Sciences, 6(3), 294–299. https://doi.org/10.1016/j.ijnss.2019.05.001
Maqsood, M. H., Levine, G. N., Kleiman, N. D., Hasdai, D., Uretsky, B. F., & Birnbaum, Y. (2023). Do we still need aspirin in coronary artery disease? Journal of Clinical Medicine, 12(24), 7534. https://doi.org/10.3390/jcm12247534
Marbach, J. A., Alhassani, S., Chong, A.-Y., MacPhee, E., & Le May, M. (2020). A novel protocol for very early hospital discharge after STEMI. Canadian Journal of Cardiology, 36(11), 1826–1829. https://doi.org/10.1016/j.cjca.2020.08.012
Passacquale, G., Sharma, P., Perera, D., & Ferro, A. (2022). Antiplatelet therapy in cardiovascular disease: Current status and future directions. British Journal of Clinical Pharmacology, 88(6). https://doi.org/10.1111/bcp.15221
Simard, T., Jung, R. G., Di Santo, P., Harnett, D. T., Abdel-Razek, O., Ramirez, F. D., Motazedian, P., Parlow, S., Labinaz, A., Moreland, R., Marbach, J., Poulin, A., Levi, A., Majeed, K., Boland, P., Couture, E., Sarathy, K., Promislow, S., Russo, J. J., . . . Hibbert, B. (2021). Modifiable risk factors and residual risk following coronary revascularization. Mayo Clinic Proceedings. Innovations, Quality & Outcomes, 5(6), 1138–1152. https://doi.org/10.1016/j.mayocpiqo.2021.09.001
Whalen, D., Dunne, C., Dubrowski, A., Mohamed, L., & Parsons, M. H. (2019). Diagnosis and management of an inferior st-elevation myocardial infarction: A simulation scenario. Cureus, 11(2). https://doi.org/10.7759/cureus.3995
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Elias Leon Case Study
Patient Information:
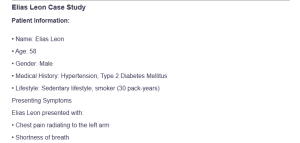
Elias Leon Case Study
• Name: Elias Leon
• Age: 58
• Gender: Male
• Medical History: Hypertension, Type 2 Diabetes Mellitus
• Lifestyle: Sedentary lifestyle, smoker (30 pack-years)
Presenting Symptoms
Elias Leon presented with:
• Chest pain radiating to the left arm
• Shortness of breath
• Profuse sweating
• Nausea
These symptoms are indicative of a potential acute coronary syndrome (ACS), a spectrum of conditions associated with sudden, reduced blood flow to the heart
ELIAS LEON I HUMAN CASE STUDY IS A 62-YEAR-OLD MALE WITH A HISTORY OF HYPERTENSION, TYPE 2 DIABETES, AND DYSLIPIDEMIA. HE IS A NON-SMOKER AND CONSUMES ALCOHOL OCCASIONALLY. HE REPORTS EXPERIENCING SHORTNESS OF BREATH, FATIGUE, AND SWELLING IN HIS LEGS FOR THE PAST FEW WEEKS.
ELIAS LEON I HUMAN CASE STUDY IS A 62-YEAR-OLD MALE WITH A HISTORY OF HYPERTENSION, TYPE 2 DIABETES, AND DYSLIPIDEMIA. HE IS A NON-SMOKER AND CONSUMES ALCOHOL OCCASIONALLY. HE REPORTS EXPERIENCING SHORTNESS OF BREATH, FATIGUE, AND SWELLING IN HIS LEGS FOR THE PAST FEW WEEKS.
Diagnosis: Acute ST – Segment elevation Myocardial Infarction (STEMI), caused by blockage in LAD artery.
Write SOAP
Management Plan: Use the expert diagnosis provided to create a pertinent, comprehensive, evidenced-based management plan. Address the following criteria in the plan:
1.) Diagnostic tests;
2.) Medications (write out a complete order, even for OTC meds);
3.) Suggested consults/referrals;
4.) Patient education;
5.) Follow-up, including time interval and specific symptoms to prompt a return visit sooner;
6.) Provide rationales for each intervention and include references to support your plan. Clinical practice guidelines should be utilized as applicable.
This criterion is linked to a Learning Outcome References and Format: Current APA citations for references in management plan. Use of clinical practice guidelines when applicable.

