Comprehensive Psychiatric Evaluation – Major Depressive Disorder
CC (chief complaint): “I am returning for my routine follow-up”.
HPI: EM is a 24-year-old female presenting to the clinic for follow up with Major Depressive Disorder. The symptoms began six weeks ago and have been present since. They manifest in the better part of the day especially when she is tending to family and work duties. She reports being anxious and having difficulty with self-care while managing family issues and work-related stress. She notes that her symptoms have improved following consistent self-care activities such as medication, journaling, and walking out.
Past Psychiatric History:
- General Statement: The patient has a history of psychiatric illness and is on medications.
- Caregivers (if applicable): N/A
- Hospitalizations: No reports of previous hospitalizations.
- Medication trials: The patient hasn’t had any trials with psychotropic medications.
- Psychotherapy or Previous Psychiatric Diagnosis: The patient is presenting for follow-up for major depressive disorder. She has a history of depression and mood fluctuations and raising concerns about bipolar disorder. The patient has experienced significant improvement in her wellness through self-care activities such as working out, journaling, and medication. She was also initiated on CBT to help address her symptoms.
Substance Current Use and History: No reports of alcohol use, cigarette smoking, or use of any other substance of abuse.
Family Psychiatric/Substance Use History: No history of substance use or psychiatric illnesses in the family.
Psychosocial History: The patient is a 24-year-old male. He contends with several work and family issues and verbalizes having difficulty with self-care when managing the family and work issues. The patient has a negative legal history. There are also no reports of involvement in any form of violence or any childhood traumas.
Sleep: The patient denies nightmares or any sleep disturbances.
Medical History: The patient is currently on medication and has not experienced any side effects from the drugs.
- Current Medications: The patient is currently on Adderall 10mg, Rexulti 2mg, Lamotrigine 200mg, and Venlafaxine 75mg. All the medications are taken orally in a once daily dosing.
- Allergies: No known drug allergies.
ROS:
- GENERAL: The patient is calm. No reports of fever or chills.
- HEENT: Denies head injuries, visual or hearing loss, nasal discharge, or difficulty swallowing.
- CARDIOVASCULAR: Denies chest pain, palpitations, or irregular heart rhythms.
- RESPIRATORY: Denies coughs, wheezing, congestion, or shortness of breath
- GASTROINTESTINAL: Reports eating well. Denies any GI disturbances or abdominal pain.
- GENITOURINARY: Denies dysuria, urinary frequency, or urgency,
- NEUROLOGICAL: Denies confusion, fogginess, or headaches.
- MUSCULOSKELETAL: Denies joint, skeletal, or muscle pain.
- HEMATOLOGIC: Denies anemia, or excessive bleeding.
- LYMPHATICS: Denies lymph node swelling or splenomegaly.
- ENDOCRINOLOGIC: Denies heat or cold intolerance, or diabetes.
- INTEGUMENTARY: Denies rashes, scars, or any skin lesions.
- Psychiatric: The patient has episodic depression symptoms and feelings of detachment.
Physical exam: if applicable
Diagnostic results: Not ordered. Diagnostic screening tools such as the Patient Health Questionnaire-9 and the Generalized Anxiety Disorder-7 may be necessitated to distinguish depression from anxiety disorders.
Assessment
Mental Status Examination: The patient is alert and oriented to place and event. She is cooperative and well-groomed. Her speech is intact and normal in tone. Her memory is intact, and her thought process is linear. Her judgment and insights are excellent. Her eye contact is also good. Her mood is labile. She denies having suicidal ideations or attempts.
Differential Diagnoses:
- Major depressive disorder: Major depressive disorder is a psychiatric illness characterized by persistent low mood. According to DSM-V, a diagnosis of MDD is made in the presence of anhedonia and depressed mood lasting beyond six months (Christensen et al., 2020). The patients in the case presented with episodic depression warranting the inclusion of this differential. Continued monitoring and assessment are necessitated to ascertain whether the case meets the criteria for MDD as outlined in DSM-V.
- Unspecified mood disorder: Mood disorders are a spectrum of psychiatric illnesses characterized by marked disruptions in the emotional state of an individual. A diagnosis is made in the presence of emotional disruptions lasting more than six months (Motichand & Ram, 2020). The patients in the case presented had mood lability and reported anxiety. These manifestations warrant the inclusion of a mood disorder. Continuous assessment is necessitated to rule out this diagnosis.
- General anxiety disorder: GAD is a psychiatric condition characterized by persistent anxiety. The affected persons often have difficulty controlling their anxiety. A diagnosis of GAD can be made in the presence of anxiety lasting for more than six months. The anxiety must be associated with other symptoms such as restlessness, fatiguability, irritability, sleep disturbance, and muscle tension, and result in impairment in the social and occupational areas (Mishra & Varma, 2023). The diagnosis is included because of the presence of anxiety. Continued assessment of the patient is warranted to rule out the diagnosis.
Reflections:
The presenting case is of a 24-year-old male presenting for a diagnostic assessment for MDD. I agree with my preceptor’s assessment of the case. Moving forward, I would focus on diagnostic screening using diverse screening tools to aid the diagnosis. A legal consideration that would be made in the case is competence. Competence in psychiatric care prevents caregivers from making decisions based on their emotions (Aftab et al., 2024). In this respect, they should not allow emotions to influence decision-making. An ethical consideration that interplays in the case is beneficence. Beneficence requires that caregivers act in the best interest of their patients.
Consistently, access to mental healthcare is a social determinant of health envisioned in Healthy People 2030 and applied to the case presented (Healthy People 2030., n.d.). Caregivers can enhance the patient’s access to healthcare by making the care acceptable. As a point of health promotion for the patient, she should be educated on healthy living and the significance of routine clinical visitations to aid the diagnosis and management.
PRECEPTOR VERFICIATION:
I confirm the patient used for this assignment is a patient that was seen and managed by the student at their Meditrek approved clinical site during this quarter course of learning.
Preceptor signature: ________________________________________________________
Date: ________________________
References
Aftab, A., Sadler, J. Z., Kious, B. M., & Waterman, G. S. (2024). Conceptual competence in psychiatric training: Building a culture of conceptual inquiry. BJPsych Bulletin, 1–6. https://doi.org/10.1192/bjb.2024.12
Christensen, M. C., Wong, C. M., & Baune, B. T. (2020). Symptoms of major depressive disorder and their impact on psychosocial functioning in the different phases of the disease: Do the perspectives of patients and healthcare providers differ? Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00280
Healthy People 2030. (n.d.). Mental Health and Mental Disorders. Mental Health and Mental Disorders – Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/browse-objectives/mental-health-and-mental-disorders#:~:text=Healthy%20People%202030%20focuses%20on,people%20affected%20by%20these%20conditions.
Mishra, A. K., & Varma, A. R. (2023). A comprehensive review of the Generalized Anxiety Disorder. Cureus. https://doi.org/10.7759/cureus.46115
Motichand, S., & Ram, D. (2020). Conceptual issues in mood disorder: An update. Industrial Psychiatry Journal, 29(1), 22. https://doi.org/10.4103/ipj.ipj_37_15
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
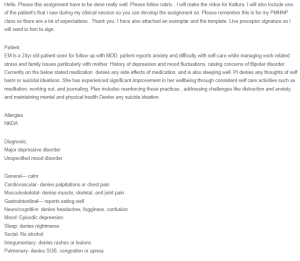
Hello. Please this assignment have to be done really well. Please follow rubric . I will make the vidoe for Kaltura. I will also include one of the patient’s that i saw during my clinical session so you can devolop the assignment on. Please remember this is for my PMHNP class so there are a lot of expectations . Thank you. I have also attached an examplar and the template. Live preceptor signature as i will send to him to sign.
Comprehensive Psychiatric Evaluation – Major Depressive Disorder
Patient
EM is a 24yr old patient seen for follow up with MDD. patient reports anxiety and difficulty with self-care while managing work related stress and family issues particularly with mother. History of depreesion and mood fluctuations, raising concerns of Bipolar disorder. Currenlty on the below stated medication. denies any side effects of medication, and is also sleeping well. Pt denies any thoughts of self harm or suicidal ideations. She has experienced significant improvement in her wellbeing through consistent self care activities such as meditation, working out, and journaling. Plan includes reenforcing these practices , addressing challenges like distraction and anxiety, and maintaining mental and physical health.Denies any suicida ideation.
Allergies
NKDA
Diagnosis;
Major depressive disorder
Unspecified mood disorder
General— calm
Cardiovascular- denies palpitations or chest pain
Musculoskeletal- denies muscle, skeletal, and joint pain
Gastrointestinal— reports eating well
Neuro/cognitive: denies headaches, fogginess, confusion
Mood: Episodic depreesion
Sleep: denies nightmares
Social: No alcohol
Integumentary- denies rashes or lesions
Pulmonary- denies SOB, congestion or apnea
Medication:
Adderall 10mg
Rexulti 2mg
Lamotrigine 200mg
Venlafaxine 75mg
EM a 24yr old patient who is A&O intelligent, cooperative,pleasant female , well-groomed, ps speech and thought process is clear and concrete, thought process is linear Memory is intact, judgment, insight, concentration, attention is good. Eye Contact good., Psychotherapy talk/CBT and active listening were provided. Patient exibit mood laibiity, episodic depression symptoms and feelings of detachment.Increase shift from episodic depression to feeling normal or happy.
TReatment plan
Adding Latuda 20mg, monitoring symptoms.
Potentially d/c Rexulti after a month.
Follow up in four weeks.
Assignment instructions
Comprehensive psychiatric evaluations are a way to reflect on your practicum experiences and connect the experiences to the learning you gain from your weekly Learning Resources. Comprehensive notes, such as the ones required in this practicum course, are often used in clinical settings to document patient care.
For this Assignment, you will document information about a patient that you examined during the last 5 weeks, using the Comprehensive Psychiatric Evaluation Template provided. You will then use this note to develop and record a case presentation for this patient.
Resources
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCE
To Prepare
Select a patient that you examined during the last 5 weeks. Review prior resources on the disorder this patient has.
It is recommended that you use the Kaltura Media tool to record and upload your assignment.
Review the Kaltura Media resource in the Classroom Support Center area (accessed via the Help button).
Conduct a Comprehensive Psychiatric Evaluation on this patient using the template provided in the Learning Resources. There is also a completed exemplar document in the Learning Resources so that you can see an example of the types of information a completed evaluation document should contain. All psychiatric evaluations must be signed by your Preceptor. You will submit your document in Week 5 Assignment, Part 2 area and you will include the complete Comprehensive Psychiatric Evaluation as well as have your preceptor sign the completed assignment. You must submit your documents using Turnitin. Please Note: Electronic signatures are not accepted. If both files are not received by the due date, Faculty will deduct points per the Walden Late Policies.
Develop a video case presentation, based on your progress note of this patient, that includes chief complaint; history of present illness; any pertinent past psychiatric, substance use, medical, social, family history; most recent mental status exam; and current psychiatric diagnosis, including differentials that were ruled out.
Include at least five (5) scholarly resources to support your assessment and diagnostic reasoning.
Ensure that you have the appropriate lighting and equipment to record the presentation.
Assignment
Record yourself presenting the complex case for your clinical patient.
Do not sit and read your written evaluation! The video portion of the assignment is a simulation to demonstrate your ability to succinctly and effectively present a complex case to a colleague for a case consultation. The written portion of this assignment is a simulation for you to demonstrate to the faculty your ability to document the complex case as you would in an electronic medical record. The written portion of the assignment will be used as a guide for faculty to review your video to determine if you are omitting pertinent information or including non-essential information during your case staffing consultation video.
In your presentation:
Dress professionally and present yourself in a professional manner.
Display your photo ID at the start of the video when you introduce yourself.
Ensure that you do not include any information that violates the principles of HIPAA (i.e., don’t use the patient’s name or any other identifying information).
Present the full case. Include chief complaint; history of present illness; any pertinent past psychiatric, substance use, medical, social, family history; most recent mental status exam; and current psychiatric diagnosis, including differentials that were ruled out.
Report normal diagnostic results as the name of the test and “normal” (rather than specific value). Abnormal results should be reported as a specific value.
Be succinct in your presentation, and do not exceed 8 minutes. Address the following:
Subjective: What details did the patient provide regarding their personal and medical history? What are their symptoms of concern? How long have they been experiencing them, and what is the severity? How are their symptoms impacting their functioning?
Objective: What observations did you make during the interview and review of systems?
Assessment: What were your differential diagnoses? Provide a minimum of three (3) possible diagnoses. List them from highest to lowest priority. What was your primary diagnosis, and why?
Reflection notes: What would you do differently in a similar patient evaluation? Reflect on one social determinant of health according to the HealthyPeople 2030 (you will need to research) as applied to this case in the realm of psychiatry and mental health. As a future advanced provider, what are one health promotion activity and one patient education consideration for this patient for improving health disparities and inequities in the realm of psychiatry and mental health? Demonstrate your critical thinking.

