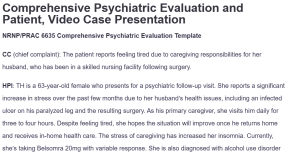
Comprehensive Psychiatric Evaluation and Patient, Video Case Presentation
NRNP/PRAC 6635 Comprehensive Psychiatric Evaluation Template
CC (chief complaint): The patient reports feeling tired due to caregiving responsibilities for her husband, who has been in a skilled nursing facility following surgery.
HPI: TH is a 63-year-old female who presents for a psychiatric follow-up visit. She reports a significant increase in stress over the past few months due to her husband’s health issues, including an infected ulcer on his paralyzed leg and the resulting surgery. As his primary caregiver, she visits him daily for three to four hours. Despite feeling tired, she hopes the situation will improve once he returns home and receives in-home health care. The stress of caregiving has increased her insomnia. Currently, she’s taking Belsomra 20mg with variable response. She is also diagnosed with alcohol use disorder and is presently on Naltrexone 50MG, and reports sobriety for six months. It also includes IED- Current Olanzapine 10mg, though, at times, the irritability does continue and with particular provocation under stress.
Past Psychiatric History:
- General Statement: TH first experienced psychiatric symptoms in her early 50s, including anxiety and irritability, which led to her diagnosis of IED.
- Caregivers (if applicable): None
- Hospitalizations: None
- Medication trials: Previous trials of sleep aids before settling on Belsomra for insomnia. No adverse reactions to current medications.
- Psychotherapy or Previous Psychiatric Diagnosis: The patient has not engaged in psychotherapy but was diagnosed with IED.
Substance Current Use and History: She has a history of alcohol use disorder, particularly excessive drinking during stressful times. The patient has remained abstinent over the past six months and upon initiation of Naltrexone. She denies the use of any illicit drugs.
Family Psychiatric/Substance Use History: Despite having a history of depression, her mother never received a formal diagnosis. There is no documented significant family history of substance use issues.
Psychosocial History: The patient grew up in Florida, where they were born. She is married with two grown children. She was a nursing professional for 30 years before retiring five years ago to take care of her husband. She does not have any legal issues or trauma history.
Medical History: TH is well-managed with medication for both hypertension and hyperlipidemia. A decade ago, she had a hysterectomy. She has no known allergies.
- Current Medications:
- Belsomra 20mg at bedtime for insomnia.
- Naltrexone 50 daily for alcohol use disorder.
- Olanzapine 10 daily for intermittent explosive disorder.
- Allergies: No known allergies.
- Reproductive Hx: The patient had a hysterectomy 10 years ago.
ROS:
- GENERAL: Nonappearance of weakness, fever, chills, weight loss, or weariness unrelated to caring for others.
- HEENT: Eyes: Yellow sclerae absent, blurred vision, or visual loss. No congestion, stinging throat, or hearing loss in the ears, nose, or throat.
- SKIN: There is no sign of a rash or irritation.
- CARDIOVASCULAR: There are no palpitations or pain in the chest.
- RESPIRATORY: There is no loss of breath or cough.
- GASTROINTESTINAL: Diarrhea, vomiting, nausea, or stomach pain absent.
- GENITOURINARY: No complaints about the urine or unusual discharge.
- NEUROLOGICAL: Absence of numbness, headaches, or dizziness.
- MUSCULOSKELETAL: No joint stiffness or muscular soreness.
- HEMATOLOGIC: No prior bleeding or anemia.
- LYMPHATICS: Not enlarged lymph node.
- ENDOCRINOLOGIC: No polydipsia or polyuria.
Physical exam: Not applicable as this was a psychiatric follow-up.
Diagnostic results: None available at this time. Lab tests or diagnostic imaging were not conducted during this visit.
Assessment
Mental Status Examination:
- Appearance: Well-groomed, looks the age she claims to be.
- Behavior: Cooperative yet seems worn out.
- Speech: Lucid and well-organized.
- Mood: Feeling anxious and worn out.
- Affect: Mood-appropriate; somewhat constrained.
- Thought Process: Rational and purpose-driven.
- Thought Content: No hallucinations or delusions.
- Cognition: Aware of the time and location.
- Insight/Judgment: Acknowledges the impact of stress on her well-being but struggles to cope with the caregiving responsibility.
- SI/HI: Denies having thoughts of suicide or murder.
Differential Diagnoses:
- Adjustment Disorder with Mixed Anxiety and Depressed Mood (ICD-10 code F43.23): The patient’s symptoms of stress, exhaustion, and difficulty coping are consistent with this diagnosis, as they have emerged in response to her husband’s illness and caregiving burden, as noted by O’Donnell et al. (2020).
- Major Depressive Disorder (MDD) (ICD-10 code F32.9): The patient’s fatigue, insomnia, and stress could suggest depression, but the absence of a persistent low mood or anhedonia makes this less likely (Bains & Abdijadid, 2023).
- Generalized Anxiety Disorder (GAD) (ICD-10 code F41.1): Although the patient experiences significant stress and worry about her husband’s health, her anxiety does not meet the full criteria for GAD, as it is situational and linked to a specific stressor as stressed by Munir and Takov (2022).
Primary Diagnosis:
- Intermittent Explosive Disorder (IED) (ICD-10 code F63.81): The patient’s history of verbal outbursts and irritability, particularly in stress response, aligns with the DSM-5 criteria for IED, as indicated by Scott et al. (2020). While her symptoms have improved with Olanzapine, they occasionally reappear under heightened stress.
Reflections: This case highlights the significant emotional toll that caregiving can take on individuals, especially those with pre-existing psychiatric conditions. In future evaluations, more emphasis could be placed on identifying caregiver burnout early and providing resources, such as support groups and counseling, to alleviate the burden. One social determinant of health relevant to this case is access to healthcare and social support. According to Leykum et al. (2022), reducing caregiver stress through better access to support services can help improve health outcomes. As a future advanced provider, I emphasize health promotion activities that focus on stress management and coping strategies, along with patient education on the importance of self-care and seeking external support when needed.
PRECEPTOR VERFICIATION:
I confirm the patient used for this assignment is a patient that was seen and managed by the student at their Meditrek approved clinical site during this quarter course of learning.
Preceptor signature: ________________________________________________________
Date: ________________________
References
Bains, N., & Abdijadid, S. (2023). Major depressive disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559078/
Leykum, L. K., Penney, L. S., Dang, S., Trivedi, R. B., Noël, P. H., Pugh, J. A., Shepherd-Banigan, M. E., Pugh, M. J., Rupper, R., Finley, E., Parish-Johnson, J., Delgado, R., Peacock, K., Kalvesmaki, A., & Van Houtven, C. H. (2022). Recommendations to Improve Health Outcomes Through Recognizing and Supporting Caregivers. Journal of General Internal Medicine, 37(5), 1265–1269. https://doi.org/10.1007/s11606-021-07247-w
Munir, S., & Takov, V. (2022). Generalized anxiety disorder. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441870/
O’Donnell, M. L., Agathos, J. A., Metcalf, O., Gibson, K., & Lau, W. (2020). Adjustment disorder: Current developments and future directions. International Journal of Environmental Research and Public Health, 16(14), 2537. https://doi.org/10.3390/ijerph16142537
Scott, K. M., de Vries, Y. A., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Bromet, E. J., Bunting, B., Caldas-de-Almeida, J. M., Cía, A., Florescu, S., Gureje, O., Hu, C-Y., Karam, E. G., Karam, A., Kawakami, N., Kessler, R. C., Lee, S., McGrath, J., Oladeji, B., & Posada-Villa, J. (2020). Intermittent explosive disorder subtypes in the general population: association with comorbidity, impairment and suicidality. Epidemiology and Psychiatric Sciences, 29(138). https://doi.org/10.1017/S2045796020000517
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Comprehensive psychiatric evaluations are a way to reflect on your practicum experiences and connect the experiences to the learning you gain from your weekly Learning Resources. Comprehensive notes, such as the ones required in this practicum course, are often used in clinical settings to document patient care.
For this Assignment, you will document information about a patient that you examined during the last 2 weeks, using the Comprehensive Psychiatric Evaluation Template provided. You will then use this note to develop and record a case presentation for this patient.
To Prepare
- Review this week’s Learning Resources and consider the insights they provide about assessment and diagnosis. Also review the Kaltura Media resource in the Classroom Support Center (accessed via the Help button).
- Select a patient that you examined during the last 2 weeks who presented with a disorder other than the one present in your selected case for Week 5.
- Conduct a Comprehensive Psychiatric Evaluation on this patient using the template provided in the Learning Resources. There is also a completed exemplar document in the Learning Resources so that you can see an example of the types of information a completed evaluation document should contain. All psychiatric evaluations must be signed by your Preceptor. When you submit your document, you should include the complete Comprehensive Psychiatric Evaluation as a Word document and the completed assignment signed by your Preceptor. You must submit your document using Turn It In.
- Please Note: Electronic signatures are not accepted. If both files are not received by the due date, Faculty will deduct points per the Walden Late Policies.
- Develop a video case presentation, based on your evaluation of this patient, that includes chief complaint; history of present illness; any pertinent past psychiatric, substance use, medical, social, family history; most recent mental status exam; and current psychiatric diagnosis, including differentials that were ruled out.
- Include at least five (5) scholarly resources to support your assessment and diagnostic reasoning.
- Ensure that you have the appropriate lighting and equipment to record the presentation.
Comprehensive Psychiatric Evaluation and Patient, Video Case Presentation
Assignment
Record yourself presenting the complex case for your clinical patient.
Do not sit and read your written evaluation! The video portion of the assignment is a simulation to demonstrate your ability to succinctly and effectively present a complex case to a colleague for a case consultation. The written portion of this assignment is a simulation for you to demonstrate to the faculty your ability to document the complex case as you would in an electronic medical record. The written portion of the assignment will be used as a guide for faculty to review your video to determine if you are omitting pertinent information or including non-essential information during your case staffing consultation video.
In your presentation:
- Dress professionally and present yourself in a professional manner.
- Display your photo ID at the start of the video when you introduce yourself.
- Ensure that you do not include any information that violates the principles of HIPAA (i.e., don’t use the patient’s name or any other identifying information).
- Present the full case. Include chief complaint; history of present illness; any pertinent past psychiatric, substance use, medical, social, family history; most recent mental status exam; and current psychiatric diagnosis including differentials that were ruled out.
- Report normal diagnostic results as the name of the test and “normal” (rather than specific value). Abnormal results should be reported as a specific value.
- Be succinct in your presentation, and do not exceed 8 minutes. Address the following:
- Subjective: What details did the patient provide regarding their personal and medical history? What are their symptoms of concern? How long have they been experiencing them, and what is the severity? How are their symptoms impacting their functioning?
- Objective: What observations did you make during the interview and review of systems?
- Assessment: What were your differential diagnoses? Provide a minimum of three (3) possible diagnoses. List them from highest to lowest priority. What was your primary diagnosis and why?
- Reflection notes: What would you do differently in a similar patient evaluation? Reflect on one social determinant of health according to the HealthyPeople 2030 (you will need to research) as applied to this case in the realm of psychiatry and mental health. As a future advanced provider, what are one health promotion activity and one patient education consideration for this patient for improving health disparities and inequities in the realm of psychiatry and mental health? Demonstrate your critical thinking.
By Day 7
Submit your Video Case Presentation.
Note: In Week 7: Assignment 2, Part 2 you will the Comprehensive Psychiatric Evaluation including two (2) files for the evaluation, including a Word document and scanned PDF/images of the completed assignment signed by your Preceptor.