Case Study – Sexually Transmitted Infections Primary Care
Sexually transmitted infections (STIs) have a significant prevalence in today’s society, and primary care settings are likely to encounter patients with symptoms of STIs. The complexity of STI cases is due to the wide range of clinical manifestations, the multiple causative agents, and the fact that diagnosis must be precise to enable proper management. This case study examines the scenario of a patient with a chief complainant who falls under STIs to discuss differential diagnoses, the pathophysiology, and how national guidelines can be applied to the diagnosis.
Chief Complaint and Patient Background
The main presenting symptom, in this case, is a vaginal discharge which is a prevalent reason for women to show up in primary care. The patient is a sexually active 24-year-old female who came with a complaint of a foul-smelling vaginal discharge that has been troubling her for the past week. She says she has mild pelvic discomfort and pruritus but does not have a fever, chills, or any urinary complaints. The patient reports having multiple sexual partners in the past six months, inconsistent condom usage, and a prior history of chlamydia treated one year ago. She has not undergone any previous surgeries and has to be informed that she is an asthmatic patient with a penicillin allergy. Her lifestyle indicators are moderate alcohol drinking, non-smoking habits, and physical activity.
Risk Factors and Differential Diagnoses
Several risk factors lead to the patient’s chief complaint: sexual activity with multiple partners and irregular condom use. These factors place her at a higher risk of getting an STI, and this should be a part of the differential diagnosis. The three differential diagnoses for this clinical scenario include bacterial vaginosis (BV), trichomoniasis, and gonorrhea.
- Bacterial Vaginosis (BV)
- Pathophysiology: Bacterial vaginosis is defined by an alteration in the least in the lactobacilli population and the increase in anaerobic organisms, as indicated by Kairys and Garg (2023). This condition is often associated with sexual behavior, but it is not considered an average STI or STD.
- Rationale: In this case, the symptoms exhibited by the patient, such as foul-smelling discharge and mild discomfort in the pelvic region, suggest BV. The lack of inflammatory markers and general clinical manifestations also contribute to this diagnosis.
- Trichomoniasis
- Pathophysiology: Trichomoniasis is a sexually transmitted parasitic disease caused by the protozoan Trichomonas vaginalis. It manifests with symptoms such as frothy, greenish vaginal secretion, vulvar itching, and lousy smell (Schumann & Plasner, 2023).
- Rationale: These symptoms and sexual history may indicate that the patient has trichomoniasis. Accordingly, the presence of pruritus and discharge with a foul smell corresponds to this condition.
- Gonorrhea
- Pathophysiology: Gonorrhea is an STI resulting from Neisseria gonorrhoeae and affects the genital tract, rectum, and throat. In women, it typically manifests with purulent vaginal discharge, lower abdominal pain, and dysuria (Springer & Salen, 2023).
- Rationale: Since the patient has a history of multiple sexual partners and has previously contracted an STI, gonorrhea is strongly considered due to its complicating effects if not treated.
Comparison of Differential Diagnoses
Despite the similarities in their clinical manifestations in females, BV, trichomoniasis, and gonorrhea are distinct diseases with different etiologies, incidences, and management protocols. BV is known to be a disturbance in the balance of vaginal microbes and is not categorized as an STI, while trichomoniasis and gonorrhea are categorically transmitted through sexual contact. However, trichomoniasis is characterized by more severe vulvovaginal manifestations, such as itching and vaginal secretion, compared to the relatively asymptomatic presentation of BV. Gonorrhea may have more severe pelvic symptoms and purulent discharge, and thus, timely treatment is necessary to avoid severe conditions like pelvic inflammatory disease.
Diagnostic Testing and National Guidelines
The diagnosis of such conditions mandates serologic testing depending on the clinical manifestations and predisposing features. A saline wet mount or Gram stain should be performed for BV to look for clue cells and a reduced number of lactobacilli. Trichomoniasis can be diagnosed by examining wet mount microscopy of the genital discharge and searching for motile trichomonads, although nucleic acid amplification tests (NAATs) are more sensitive. Gonorrhea is usually confirmed by nucleic acid amplification tests or culture of the endocervical swabs; the latter can also be used for antibiotic susceptibility tests.
Current national guidelines from the CDC advise screening for both gonorrhea and chlamydia in all sexually active women under the age of 25 or with other risk factors, which applies to this patient (CDC, 2021). CDC also provides recommendations on managing these infections, such as metronidazole for BV and trichomoniasis and ceftriaxone for gonorrhea, illustrating the relevance of applied and quality management within the primary care context.
Conclusion
This case study involves a patient who complained of a vaginal discharge, which can be associated with common STIs such as BV, trichomoniasis, and gonorrhea. These differential diagnoses can be ascertained and well managed once the evaluation of both symptoms and risk factors has been coupled with diagnostic tests that are highly relevant to each condition. Integrating national guidelines helps place appropriate patient care for positive results with fewer complications. This approach demonstrates primary care clinicians’ importance and ability to coordinate all aspects of the individual’s adult life. It stresses the importance of lifelong learning and incorporating current knowledge into clinical practice.
References
CDC. (2021). STI screening recommendations. Www.cdc.gov. https://www.cdc.gov/std/treatment-guidelines/screening-recommendations.htm
Kairys, N., & Garg, M. (2023, July 4). Bacterial vaginosis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459216/
Schumann, J. A., & Plasner, S. (2023). Trichomoniasis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534826/
Springer, C., & Salen, P. (2023, April 17). Gonorrhea. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK558903/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Week 6CEA Pre-Diagnostic Study Discussion: Part 1
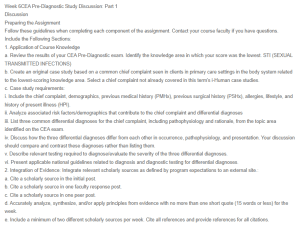
Sexually Transmitted Infections Primary Care
Discussion
Preparing the Assignment
Follow these guidelines when completing each component of the assignment. Contact your course faculty if you have questions.
Include the Following Sections:
1. Application of Course Knowledge
a. Review the results of your CEA Pre-Diagnostic exam. Identify the knowledge area in which your score was the lowest. STI (SEXUAL TRANSMITTED INFECTIONS)
b. Create an original case study based on a common chief complaint seen in clients in primary care settings in the body system related to the lowest-scoring knowledge area. Select a chief complaint not already covered in this term’s i-Human case studies.
c. Case study requirements:
i. Include the chief complaint, demographics, previous medical history (PMHx), previous surgical history (PSHx), allergies, lifestyle, and history of present illness (HPI).
ii. Analyze associated risk factors/demographics that contribute to the chief complaint and differential diagnoses
iii. List three common differential diagnoses for the chief complaint, including pathophysiology and rationale, from the topic area identified on the CEA exam.
iv. Discuss how the three differential diagnoses differ from each other in occurrence, pathophysiology, and presentation. Your discussion should compare and contrast these diagnoses rather than listing them.
v. Describe relevant testing required to diagnose/evaluate the severity of the three differential diagnoses.
vi. Present applicable national guidelines related to diagnosis and diagnostic testing for differential diagnoses.
2. Integration of Evidence: Integrate relevant scholarly sources as defined by program expectations to an external site.:
a. Cite a scholarly source in the initial post.
b. Cite a scholarly source in one faculty response post.
c. Cite a scholarly source in one peer post.
d. Accurately analyze, synthesize, and/or apply principles from evidence with no more than one short quote (15 words or less) for the week.
e. Include a minimum of two different scholarly sources per week. Cite all references and provide references for all citations.

