Case Study – Chronic Migraine
Chronic Migraine: A Comparative Analysis of Preventive Medications and Botox Injections
Chronic migraine is a serious neurological disorder that presents with recurrent, severe headaches that interfere with everyday performance and wellness. As classified by the International Classification of Headache Disorders (ICHD-3), it is a primary headache disorder that occurs 15 or more days per month, with at least eight days being migrainous in a month for three consecutive months or longer. This case study involves a 35-year-old female patient, Ms. Jane Doe, who has been diagnosed with chronic migraines for the past five years. The study aims to compare and contrast two primary treatment approaches: preventive medications such as beta-blockers and Botox injections, and choose an optimal treatment that will allow the patient to manage her health conditions without interrupting personal and professional activities.
Case Study
Patient Demographics and Initial Presentation
Ms. Jane Doe is a 35-year-old Caucasian female presenting with chronic migraines of a longstanding history now occurring for greater than 15 days monthly, lasting from 4 to 72 hours in duration. The nature of her headache is throbbing, unilateral left-sided, accompanied by aura-visual disturbances, nausea, photophobia, and phonophobia. Precipitating factors include stress, lack of sleep, and foods like chocolate and red wine. Her headache persists despite several over-the-counter medications and lifestyle adjustments; thus, the symptoms become so distressing and disruptive to her usual activities.
Medical and Family History
She has anxiety and a history of depression, currently on a maintenance dose of sertraline 50 mg daily for the last two years. She has no medical history of cardiovascular and cerebrovascular diseases. Apart from chronic migraines, Ms Doe is generally in excellent physical condition. Ms. Doe had one surgical experience years ago and delivered by cesarean section when one was complication-free throughout the said surgery and post-operatively. Family history includes a genetic background to migraine headaches since her mother was also suffering from the same disorder. Also, she has a family medical history significant for hypertension on the paternal side, so she may also be considered for other treatments due to the implications for cardiovascular health.
Lifestyle and Social History
Ms. Doe is married, has two small children, and works full-time as an elementary school teacher. She reported herself as an active person who enjoyed a regular exercise routine, but her migraines had worsened in frequency and severity in the last several months, forcing her to significantly curtail this activity. She also denies smoking, uses alcohol occasionally socially-and has never used recreational drugs. Ms. Doe related that she is very concerned about her inability to perform her job and take care of her family because of these chronic migraines. Yet, despite health adversities, she remains committed to finding an effective treatment that will allow her to regain control over her life.
Review of Systems and Physical Examination
On review of systems, the patient stated she frequently suffered from headaches with occasional dizziness; otherwise, she had no pertinent positives associated with the cardiovascular, respiratory, gastrointestinal, urinary, and musculoskeletal systems, while stating she has not experienced weight loss, fever, or chills recently. On physical examination, the patient demonstrated the following vital signs: BP 128/80 mmHg, HR 72 bpm, RR 16 breaths/min, and Temp 98.6°F. She had no evidence of focal neurological deficits. Gait and coordination were normal. Given the chronic nature of her migraine headaches and the total lack of any ominous physical examination findings, attention was turned to a discussion of targeted therapy options that might provide a long-term benefit.
Laboratory and Imaging Results
Laboratory investigations and imaging studies were carried out to exclude secondary causes of her migraines. A recent MRI of the brain was unremarkable, thereby excluding structural abnormalities or intracranial pathologies that may account for her symptoms. Complete Blood Count, Basic Metabolic Panel, and thyroid function tests were within normal limits. These findings supported the chronic migraine diagnosis, where further testing at this point was unnecessary.
Diagnosis and Clinical Impression
According to clinical symptoms and application of ICDH III-beta criteria, Ms Doe’s diagnosis was chronic migraine. Migraine with chronicity is still a complicated phenomenon that is beyond simple pharmacological control and may involve an individualized treatment plan (Pescador Ruschel & De Jesus, 2023). Considering the high frequency and severity of migraines in Ms Doe and the limited effectiveness of such basic medications and changes in behaviour strategies, it was understood that more comprehensive techniques of therapy were required to enhance the quality of her life.
Differential Diagnosis
In a case like that of Ms. Doe, several differential diagnoses will have to be considered about chronic migraine. This includes tension-type headache, which presents with bilateral pressing-like pain; cluster headache, usually with severe unilateral pain drawings around the eye; and medication-overuse headache, which often occurs with frequent analgesic use. Other possibilities include trigeminal neuralgia and cervicogenic headaches, which can be ruled out through imaging and patient history. Although these symptoms are most consistent with chronic migraine, ruling out such conditions provides proper treatment and prevents mismanagement.
Comparative Treatment Options
Preventive Medications (Beta-Blockers)
- Medication: Propranolol 80 mg extended-release orally once daily.
- Route:
- Frequency: Once daily.
- Mechanism of Action: Beta-blockers, such as propranolol, work by blocking the effects of adrenaline on the cardiovascular system, leading to a reduction in heart rate and dilation of blood vessels as indicated by Farzam and Jan (2023). It is believed that this action decreases the occurrence and severity of migraines by normalizing blood flow in the brain and decreasing the susceptibility of the blood vessels to migraine-inducing stimuli. Beta-blockers are often employed as first-line prophylactic therapy for migraines, especially in patients with other disorders like hypertension (Tzankova et al., 2023).
- Efficacy: Reports from clinical trials have revealed that prophylactic use of beta blockers can significantly decrease the frequency of migraines by as much as half, thereby making them an effective long-term cure for migraine (Kumar & Kadian, 2020). However, their application may not be effective in cases of contraindications, including asthma, bradycardia, and depression, as beta-blockers may aggravate the condition.
Botox Injections
- Medication: OnabotulinumtoxinA (Botox) 100 units.
- Route: Intramuscular injection.
- Frequency: Every 12 weeks.
- Mechanism of Action: Botox acts by reducing the release of neurotransmitters associated with pain in muscles on the head and neck, as highlighted by Brin and Burstein (2023). Since these pain signals are not communicated to the brain, Botox successfully minimizes the occurrence and impact of migraine headaches. Botox is given through injections at several points in the head and neck area the areas in which muscles commonly considered to be involved in migraine are found.
- Efficacy: Botox has been FDA-approved for the treatment of chronic migraines and has been shown to reduce the number of headache days by approximately 8-9 days per month in patients with chronic migraines (Kępczyńska & Domitrz, 2022). This makes it a highly effective treatment option for patients who have not responded to other preventive therapies.
Comparative Analysis of Treatment Options
Efficacy and Research Support
Beta-blockers and Botox proved to be effective migraine prophylaxis; however, individual patient characteristics, comorbidities, and preferences should be the ultimate guide. Beta-blockers are well utilized for migraine prophylaxis, particularly given the fact that the patients in concern often present with hypertension or cardiovascular diseases as highlighted by Danesh & Gottschalk (2019). It is particularly useful in migraine with aura as its action of vasodilatation inhibits the onset of the migraine attack.
Notably, Botox is approved by the FDA for chronic migraines and is also sometimes considered for patients who fail to respond with other preventative measures. The application of Botox differs from most therapeutic agents since it functions by blocking neurogenic inflammation in migraines, positions Burstein et al. (2020) according to which Botox is useful in minimizing the frequency of headaches and enhancing the quality of life in patients with chronic migraines. Also, Botox is known not to have a systemic action, meaning that it has minimal impact when other systems in the body are involved, making it safer for patients with other health conditions that the use of other medications may exacerbate.
Side Effects and Patient Considerations
Despite being taken without any serious adverse reaction, beta-blockers may cause many side effects such as fatigue, bradycardia, hypotension, and worsening of depressive symptoms. These side effects are not desirable, especially in patients like Ms. Doe, who already suffers from anxiety and depression. As for the opposition to the use of beta-blockers, this is due to their ability to exacerbate these conditions, even though they are quite effective in the prevention of migraine attacks.
Subsequently, Botox injection therapy, although invasive, is generally associated with fewer side effects, such as mild and transient problems, including pain, muscle weakness, and discomfort in the loci of injection (Witmanowski & Błochowiak, 2020). Therefore, the localized action of Botox minimizes the side effects and could be good for Ms. Doe since she is concerned about the general side effects of the product and the extent to which the anti-wrinkle injection does not inhibit her activities. Furthermore, the dosing for Botox at 12 weeks apart may be easier to maintain as compared to daily beta-blockers.
Patient Preference and Cultural Considerations
Ms. Doe has indicated that she would like a treatment that does not significantly affect her functioning or worsen her anxiety and depression. She is especially worried about the side effects that come with oral medications and wants an alternative migraine treatment that is as effective but has no side effects. This treatment option fits her lifestyle well because it is localized and helps her address her concerns without much discomfort. Also, due to the long interval between the injections, Botox requires less frequent administration, once in three months, thus enhancing the patient’s compliance level and satisfaction with the treatment.
Selected Treatment Plan and Justification
After careful thinking and discussion, it was concluded that Botox injections were the most suitable treatment for Ms Doe. This is in alignment with her clinical presentation, evidencing the effectiveness of Botox in lessening migraines and her request for minimal numbers of systemic side effects. The lack of side effects, long intervals between injections and minimal risks allows the use of Botox as an advantageous option for treating chronic migraines and lead Ms Doe to a full life.
Treatment Plan
- Medication: OnabotulinumtoxinA (Botox) 100 units.
- Route: Intramuscular injection.
- Frequency: Every 12 weeks.
- Monitoring: Ms Doe will be observed for any signs of complications in the following days after Botox administration. Maintenance appointments will be fixed every 12 weeks to check on the effectiveness of the treatment and maybe fine-tune it. Also, Ms Doe will be advised to continue using a headache diary that will help her document the frequency and intensity of the migraines so that a better approach for the therapy can be adopted.
Patient Education and Follow-Up
Ms. Doe will be fully informed of the possible benefits and risks associated with botox injection treatment. She will also be informed of the expected effects of the treatment, such as a decrease in the number of headaches. Side effects of the treatment include injection site soreness and muscle weakness. Ms. Doe will be encouraged not to engage in certain activities that trigger migraines, such as certain meals and stress, and to sleep regularly to minimize such migraine attacks.
Besides, there shall be follow-up review appointments every 12 weeks to ensure that Ms Doe comprehensively responded to the treatment plan and to ensure she was adhering to the treatment goals as elucidated by Gonçalves-Bradley et al. (2022). During these visits, the healthcare provider will be able to assess the effectiveness of the procedures involving Botox injections, clarify concerns or issues that may exist or arise with Ms Doe, and adjust the management plan if necessary. Ms. Doe will also be urged to report any changes in her behavior or any other processes that may enhance migraine management.
Conclusion
Chronic migraine is a severe illness. Hence, the therapy must be individual and picked according to the client’s characteristics. Given the clinical characteristics of Ms Doe and her preferences for this particular approach to her treatment, and considering the effectiveness of Botox at reducing migraine frequency, botulinum neurotoxin injections were chosen. This case is showcased to demonstrate that it is important to address clinical reality as well as patient-centered matters, especially where the decision concerns treatment in chronic migraine. When a patient decides to start with a treatment that they can be comfortable with and can also cater to, then the results are usually better, improving the quality of life.
References
Brin, M. F., & Burstein, R. (2023). Botox (onabotulinumtoxinA) mechanism of action. Medicine, 102(S1), e32372. https://doi.org/10.1097/MD.0000000000032372
Burstein, R., Blumenfeld, A. M., Silberstein, S. D., Manack Adams, A., & Brin, M. F. (2020). Mechanism of Action of OnabotulinumtoxinA in Chronic Migraine: A Narrative Review. Headache: The Journal of Head and Face Pain, 60(7). https://doi.org/10.1111/head.13849
Danesh, A., & Gottschalk, P. C. H. (2019). Beta-Blockers for Migraine Prevention: a Review Article. Current Treatment Options in Neurology, 21(4). https://doi.org/10.1007/s11940-019-0556-3
Farzam, K., & Jan, A. (2023). Beta Blockers. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532906/
Gonçalves-Bradley, D. C., Lannin, N. A., Clemson, L., Cameron, I. D., & Shepperd, S. (2022). Discharge planning from hospital. Cochrane Database of Systematic Reviews, 2022(2). https://doi.org/10.1002/14651858.cd000313.pub6
Kępczyńska, K., & Domitrz, I. (2022). Botulinum Toxin—A Current Place in the Treatment of Chronic Migraine and Other Primary Headaches. Toxins, 14(9), 619. https://doi.org/10.3390/toxins14090619
Kumar, A., & Kadian, R. (2020). Migraine Prophylaxis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507873/
Pescador Ruschel, M. A., & De Jesus, O. (2023, August 23). Migraine Headache. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560787/
Tzankova, V., Becker, W. J., & Chan, T. L. H. (2023). Pharmacologic prevention of migraine. Canadian Medical Association Journal, 195(5), E187–E192. https://doi.org/10.1503/cmaj.221607
Witmanowski, H., & Błochowiak, K. (2020). The whole truth about botulinum toxin – a review. Advances in Dermatology and Allergology/Postȩpy Dermatologii I Alergologii, 37(6), 853–861. https://doi.org/10.5114/ada.2019.82795
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Week 7: Signature Assignment – Chronic Health Problem: Comprehensive Case Study
Points: 165 | Due Date: Week 7, Day 7 | CLO: 1, 2, 3, 4, 5, 6 | Grade Category: Assignments
Assignment Prompt
For your signature assignment, you will write a scholarly case study that will compare and contrast two possible ways of treating a chronic health condition.
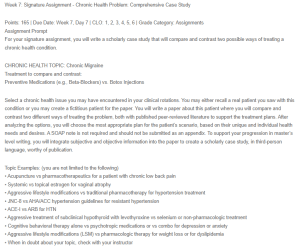
Case Study – Chronic Migraine
CHRONIC HEALTH TOPIC: Chronic Migraine
Treatment to compare and contrast:
Preventive Medications (e.g., Beta-Blockers) vs. Botox Injections
Select a chronic health issue you may have encountered in your clinical rotations. You may either recall a real patient you saw with this condition or you may create a fictitious patient for the paper. You will write a paper about this patient where you will compare and contrast two different ways of treating the problem, both with published peer-reviewed literature to support the treatment plans. After analyzing the options, you will choose the most appropriate plan for the patient’s scenario, based on their unique and individual health needs and desires. A SOAP note is not required and should not be submitted as an appendix. To support your progression in master’s level writing, you will integrate subjective and objective information into the paper to create a scholarly case study, in third-person language, worthy of publication.
Topic Examples: (you are not limited to the following)
• Acupuncture vs pharmacotherapeutics for a patient with chronic low back pain
• Systemic vs topical estrogen for vaginal atrophy
• Aggressive lifestyle modifications vs traditional pharmacotherapy for hypertension treatment
• JNC-8 vs AHA/ACC hypertension guidelines for resistant hypertension
• ACE-I vs ARB for HTN
• Aggressive treatment of subclinical hypothyroid with levothyroxine vs selenium or non-pharmacologic treatment
• Cognitive behavioral therapy alone vs psychotropic medications or vs combo for depression or anxiety
• Aggressive lifestyle modifications (LSM) vs pharmacologic therapy for weight loss or for dyslipidemia
• When in doubt about your topic, check with your instructor
Include the following information in your case study:
• Introduction: Introduce the patient demographics, complaints, and discuss key concepts related to the topic
• Setting and social dynamics (community clinic, private practice, skilled nursing facility, support system, etc.)
• Subjective information: Chief complaint, HPI, PMH, PSH, FH, SH, ROS
• Objective information: Physical exam and any known results
• Medical decision-making and clinical impression (diagnosis)
• Introduction of two different evidence-based, peer-reviewed articles or treatment guidelines for the chosen diagnosis
• Compare and contrast the two treatment options or approaches
• Assess and include analysis of the merit and soundness of research (i.e. discuss which treatment has more research or better research)
• Indicate which treatment option was chosen for the patient scenario and provide justification on why it was better for them
• Include specific plans or interventions, recommendations, education, health promotion, and follow-up as needed for the case
• Discuss possible or real cultural and socioeconomic considerations or how you would ensure equitable, inclusive care for your patient
• Conclusion: Include a summary of the case study and lessons learned
Submit a scholarly paper, written in the third person with APA 7th edition writing style at the graduate level. Include a title page, text with correct headings, and references. Do not include an abstract. Do not write the paper as a SOAP note, and do not include a SOAP note as an appendix. This is a scholarly case study. Limit the paper to 5-8 pages of text, not including the title page or references. Your instructor is not required to read or include grading beyond 8 pages of text so plan accordingly.
Expectations
• Length: 5-8 pages, excluding cover page & references,
• Format: APA 7th edition format, including citations and references
• Research: For average/competent score, a minimum of two primary or secondary peer-reviewed literature sources, preferably clinical practice guidelines

