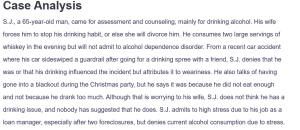
Case Analysis
S.J., a 65-year-old man, came for assessment and counseling, mainly for drinking alcohol. His wife forces him to stop his drinking habit, or else she will divorce him. He consumes two large servings of whiskey in the evening but will not admit to alcohol dependence disorder. From a recent car accident where his car sideswiped a guardrail after going for a drinking spree with a friend, S.J. denies that he was or that his drinking influenced the incident but attributes it to weariness. He also talks of having gone into a blackout during the Christmas party, but he says it was because he did not eat enough and not because he drank too much. Although that is worrying to his wife, S.J. does not think he has a drinking issue, and nobody has suggested that he does. S.J. admits to high stress due to his job as a loan manager, especially after two foreclosures, but denies current alcohol consumption due to stress.
Diagnostic: His past medical history includes hypertension, controlled with HCTZ, but no significant psychiatric history. He has never tried to stop drinking, citing no belief that he is addicted. He has made no complaint of insomnia or changes in appetite; he denies having any feelings of depression, hopelessness, or anxiety. Nonetheless, his refusal of any problem related to alcohol use, history of accident proneness, and fear expressed by his wife draw further assessment.
Diagnoses
Diagnosis #1: Alcohol Use Disorder (ICD-10 Code: F10.20)
Based on the DSM-5 criteria, S.J. meets the diagnostic threshold for Alcohol Use Disorder (AUD). The DSM-5 has categorized AUD as a set of problematic patterns of alcohol use that result in moderate or severe impairment or distress, as defined by the presence of two or more of the presented criteria within a year (Nehring & Freeman, 2024). Based on the DSM-IV criteria for AUD, S.J. displays some of the prime features, such as continued alcohol use despite negative effects, denial of a condition, and raised levels of risk related to alcohol consumption. S.J. drinks every day and has been observed consuming large quantities of whiskey without any desire to reduce or quit. Despite his wife’s concerns and the recent car accident, S.J. continues to drink, which fulfills the DSM-5 criteria of “continued alcohol use despite persistent interpersonal problems” (Nehring & Freeman, 2024).
Additionally, he has experienced blackouts and accidents, such as the guardrail collision, which are further signs of the physical dangers linked to his alcohol consumption. His daily drinking also demonstrates tolerance, though he denies experiencing withdrawal symptoms.
The patient’s denial of the severity of his drinking problem is common in those with AUD. His behavior reflects a pattern of impaired control over alcohol use and the inability to recognize its harmful impact on his life. This diagnosis is supported by his consistent alcohol consumption, minimization of its consequences, and increasing risks to his health and safety. As such, Alcohol Use Disorder is a fitting primary diagnosis for S.J., based on DSM-5 guidelines.
Diagnosis #2: Alcohol-Induced Cognitive Disorder (ICD-10 Code: F10.97)
S.J. may be experiencing Alcohol-Induced Cognitive Disorder. The New DSM-5 categorizes this affliction as an alcohol-induced persisting cognitive disorder and results in problems experienced in the areas of concentration, memory, and other cognitive domains from lasting use of alcohol. S.J. exhibits several key signs of Alcohol-Induced Cognitive Disorder, including persistent alcohol consumption despite the consequences, denial of the problem, and the increasing risk associated with his alcohol use (Meredith et al., 2020).
Neurocognitive impacts of chronic alcohol use on the affected individual are poor memory and low decision-making capabilities. Because S.J. has a history of previous blackouts, falls, and accidents, the given effects of alcohol might indicate that his cognitive function is already impaired. Also, he seems not to have any awareness of his drinking issue, and this could be a sign of some minimal brain damage because despite having a drinking problem and causing a car accident and pressure in his marriage, he discounts the effects of alcohol on his behavior.
Although S.J. does not describe significant gross cognitive dysfunction, his early evidence of cognitive dysfunction, together with heavy alcohol consumption, indicates he meets DSM-IV criteria for Alcohol-Induced Cognitive Disorder as a second diagnosis. This condition can gradually become worse for patients if they continue to drink at this level, therefore calling for early treatment.
Differential Diagnosis
Differential Diagnosis #1: Major Depressive Disorder (MDD) (ICD-10 Code: F32.9)
While S.J. denies feelings of depression, his chronic stress from work, the potential strain in his marriage, and his ongoing alcohol use raise concerns about underlying Major Depressive Disorder (MDD). The DSM-5 definition of MDD includes the processes of anhedonia, which might not necessarily indicate a patient’s sadness or depressed mood. As for depressive symptoms, S.J. does describe feeling stressed at work and strained in relation. Also, excessive drinking might be his way of dealing with these feelings since people with, for example, untreated depression often drink alcohol. Despite his denial of hopelessness and suicidal intent, it is elucidative to proceed with the assessment of his depression as a potential underlying factor for the abusive drinking and his general state of health (Bains & Abdijadid, 2023).
Differential Diagnosis #2: Generalized Anxiety Disorder (GAD) (ICD-10 Code: F41.1)
Stress, which was observed in S.J.’s case at the initial stages of the complaint in relation to their job as a loan manager and a recent car accident coupled with the triad of symptoms, could suggest Generalized Anxiety Disorder (GAD). GAD is defined by anxiety and rumination, which is associated with transitional stress. Although S.J. has not mentioned anxiety, using alcohol on a regular basis after work to avoid stress or tension may indicate chronic anxiety. The no acknowledgment of his alcohol problem and underestimation of his stress levels may well indicate that he is minimizing his anxiety symptoms (Munir & Takov, 2022). A thorough evaluation for GAD would point out if his stress and drinking pattern are a result of anxiety.
Differential Diagnosis #3: Cognitive Disorder, NOS (ICD-10 Code: F09)
Cognitive Disorder, Not Otherwise Specified (NOS) is another possible differential diagnosis. S.J. reports some cognitive difficulties, particularly with concentration, which he attributes to aging. However, his chronic alcohol use could be contributing to these cognitive challenges. His blackouts, car accidents, and poor insight into his alcohol use could be early indicators of a cognitive disorder. While Alcohol-Induced Cognitive Disorder is the primary cognitive diagnosis, Cognitive Disorder NOS should be considered if cognitive impairments persist after alcohol use is reduced or stopped (First et al., 2022).
Treatment Plan
Pharmacological Treatment
S.J. should be prescribed medications to assist in managing his alcohol use and any potential withdrawal symptoms. One option is naltrexone, which can help reduce alcohol cravings by blocking the euphoric effects of alcohol. Dose: 50 mg orally once daily (Singh & Saadabadi, 2023). If S.J. is open to reducing his drinking, naltrexone could be effective in controlling his alcohol use. Additionally, a medication such as disulfiram could be considered, which discourages alcohol consumption by causing unpleasant reactions when alcohol is consumed. Dose: 250 mg orally once daily, taken in the morning. These medications should be closely monitored, and S.J. should be educated about their effects.
Non-Pharmacological Treatment
Cognitive Behavioral Therapy (CBT) should be introduced to address S.J.’s denial of his alcohol problem and challenge his thought patterns around drinking. CBT can also assist him in learning better ways to deal with stress related to his job. Couples therapy is also needed in order to enhance S. J’s relationship with his partner and help her overcome her fear of his alcohol drinking that negatively affected their marital satisfaction. Alcoholics Anonymous (A.A.) can offer peer support and accountability, helping S.J. realize the broader impact of his drinking.
Labs and Imaging
It is recommended that S.J.’s liver should be checked periodically so as to see the effect that alcohol has had on his liver, considering that he was a heavy drinker. Further investigations like CBC and electrolyte profile may unveil how his body is faring in regard to general well-being.
Patient/Family Education and Follow-up
S.J. and his family should undertake information and education regarding the dangers of long-term alcohol consumption, such as having a Lifetime impact on cognition and physical well-being. It is suggested that S.J. come back within 1-2 weeks to assess his compliance with both pharmacological interventions and therapy. Further changes to the treatment plan are possible depending on his reactions to the applied courses of action.
References
Bains, N., & Abdijadid, S. (2023). Major depressive disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559078/
First, M. B., Yousif, L. H., Clarke, D. E., Wang, P. S., Gogtay, N., & Appelbaum, P. S. (2022). DSM‐5‐TR: Overview of what’s new and what’s changed. World Psychiatry, 21(2), 218–219. https://doi.org/10.1002/wps.20989
Meredith, L. R., Lim, A. C., & Ray, L. A. (2020). Neurocognitive performance in alcohol use disorder using the NIH toolbox: Role of severity and sex differences. Drug and Alcohol Dependence, 216(79), 108269. https://doi.org/10.1016/j.drugalcdep.2020.108269
Munir, S., & Takov, V. (2022). Generalized anxiety disorder. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441870/
Nehring, S. M., & Freeman, A. M. (2024, March 16). Alcohol use disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK436003/
Singh, D., & Saadabadi, A. (2023, May 30). Naltrexone. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534811/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
This section should include a discussion/overview of the presented case study
Diagnoses
This section should contain at least two possible diagnoses based on the information available in the case study.
Identify how each diagnosis is supported based on the information provided and appropriate rational. Make sure to provide citations.
Diagnosis #1
Diagnosis #2
Differential Diagnosis
This section should contain possible differential diagnoses applicable to the case presentation that was reviewed.
- In this section list each of the differential diagnosis:
- Define each differential diagnosis
- Identify how the differential diagnosis is supported based on the information provided in the case study.
- Provide no less than 2 and no more than 4 differential diagnosis
Differential Diagnosis #1
Differential Diagnosis #2
Differential Diagnosis #3
Case Analysis
Treatment Plan
The treatment plan should include pharmacologic treatment, non-pharmacologic treatment, any lab or imaging, patient/family education, referrals, follow-up, etc. Be sure to include generic name, strength, form, dose, instructions, how many given and any refills.
When would you want to see this patient back?
References
References should be in APA 7th edition format; must provide scholarly support for all provided information.
References need to be on a separate page

