Project Implementation – Fall prevention
Patient falls are one of the most concerning healthcare problems. They represent significant compromises to the quality and safety of care operationalizations. Fall prevention programs, such as the fall TIPS toolkit, lowers fall rates within long-term care facilities (Shao et al., 2023). The proposed project sought to implement fall TIPS in nursing care facilities.
Implementation
Implementing the Fall TIPS program followed a multi-step process that began with staff recruitment. Staff members from the nursing care facility under research were recruited through a formal invitation (Appendix A). All recruits were informed of the project’s goals and their roles in ensuring its success.
The second step was to secure a buy-in from the stakeholders. This involved communicating the need for the fall TIPS program in fall prevention and how the intervention will contribute to the safety improvement efforts. Periodic educational sessions on fall TIPS and the program were also organized to help create excitement and ensure all participants had a robust understanding of the project (Burnes, 2019). This helped secure a buy-in from the participants.
The third step was to create an implementation plan. Here, nurse leaders conducted a fall risk assessment on all the residents and identified their fall risk status and the risk factors for falls. The elucidated factors were then compiled into a checklist. Further, evidence-based fall interventions aligned with the fall risks and risk factors were determined for each resident. Participants were trained on their roles, the three-step fall prevention process, and how they can use the fall TIPS tool to prevent falls (Misaghian et al., 2024).
The fall TIPS tool was then implemented. This entailed printing the identified checklist of fall risk status and factors in a poster design. The fall TIPS instruction detailing the three-stepped fall prevention process and a fall information sheet for each resident were also printed. Each printout was then dispersed to the bedside of the respective resident. Staff members were then educated on the tool. During the training session, members were informed of the components of the printout, their significance, and how they can be used to curtail patient falls within the facility.
Diverse communication channels were established to ensure steady communication between all stakeholders involved. A dedicated call line was created to handle all queries that the team may be having regarding the tool. Likewise, virtual groups, such as WhatsApp groups, were created to enhance the visibility of all group activities. Data was collected every three days through survey forms.
Project Cost
The project cost 52 dollars. The funds went into designing and printing the posters and patient information sheets. There was a return on investment from the project as the project helped reduce fall rates within the nursing care facility by 62%. This helped save costs that would otherwise be used to treat injuries associated with patient falls (Lee et al., 2024).
Instruments for Data Collection
Data was collected through summative surveys administered after the program (Appendix B). The items on the survey form were adopted from the working objectives of the program and the expected outcomes. Participants, in this respect, were interrogated for their understanding of the fall TIPS tool.
Human Subject Protection and IRB Approval
The project integrated human participants. Participants were protected through anonymity. Informed consent was obtained from each subject before the initiation of the project (Appendix C). IRB approval was also sought.
Data Protection
Data from the project was collected and stored in a secure laptop. The data collection processes were facilitated by the investigators. The laptop used had security features, such as user verification processes. Access to the laptop and subsequent folder containing the recording was preserved by the project manager. The project does not require the collection of personally identifiable data. Data will be destroyed after 12 months.
Data Analysis
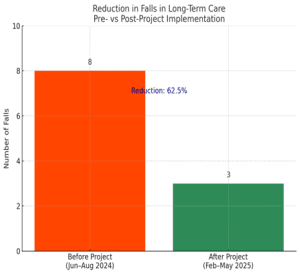
Data obtained from the survey forms was analyzed through content analysis. The data obtained demonstrated the impact of fall TIPS on fall prevention over six months. It revealed a 62.5% reduction in fall rates within the review period.
Project Sustainability
The project is sustainable. This is because it utilizes ready resources, such as staff members, and can be executed with limited resource considerations. Likewise, fall prevention interventions remain necessary across care settings (Bargmann & Brundrett, 2020).
Project Evaluation
Formative Evaluation
Formative evaluation was attained through weekly staff meetings. This enabled emerging concerns to be addressed. Through these evaluations, the DNP manager was able to ascertain members’ understanding of the deliverables and track their progress in meeting the projected outcomes.
Summative Evaluation
The project was summatively evaluated against the expected outcomes and objectives. The program was successful as it met its goal of reducing fall rates. A 62.5% reduction in fall rates was noted after implementing the fall TIPS program.
Dissemination of Information
The project will be published in the university’s journal. This will enhance its visibility to other learners. Likewise, findings will be tabulated, and the table will be displayed on the hospital’s notice boards to enhance the facility’s adoption of the fall TIPS toolkit.
References
Bargmann, A. L., & Brundrett, S. M. (2020). Implementation of a multicomponent fall prevention program: Contracting with patients for fall safety. Military Medicine, 185(Supplement_2), 28–34. https://doi.org/10.1093/milmed/usz411
Burnes, B. (2019). The origins of Lewin’s three-step model of change. The Journal of Applied Behavioral Science, 56(1), 32–59. https://doi.org/10.1177/0021886319892685
Lee, H., Hsieh, C., & Jerng, J. (2024). Incidence and factors associated with falls in older people in a long-term care facility: A prospective study in Taiwan. Healthcare, 12(10), 959. https://doi.org/10.3390/healthcare12100959
Misaghian, K., Lugo, J. E., & Faubert, J. (2024). Immediate fall prevention: The missing key to a comprehensive solution for falling hazard in older adults. Frontiers in Aging Neuroscience, 16. https://doi.org/10.3389/fnagi.2024.1348712
Shao, L., Shi, Y., Xie, X., Wang, Z., Wang, Z., & Zhang, J. (2023). Incidence and risk factors of falls among older people in nursing homes: Systematic review and meta-analysis. Journal of the American Medical Directors Association, 24(11), 1708–1717. https://doi.org/10.1016/j.jamda.2023.06.002
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Project Implementation – Fall prevention
Project review period was June -August of 2024. 10 falls were recorded during this period and 8 of those were in the long tern care.
Project implementation occurs from Feb 24, 2025 to May 5 2025.
Project Implementation – Fall prevention
During this time, the total number of falls recorded in the long term care was 3 falls
This is more than 50% decrease in falls
Please include the pre and post fall numbers in a chart or graph fomat and attached to paper.