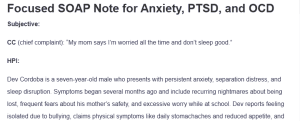
Focused SOAP Note for Anxiety, PTSD, and OCD
Subjective:
CC (chief complaint): “My mom says I’m worried all the time and don’t sleep good.”
HPI:
Dev Cordoba is a seven-year-old male who presents with persistent anxiety, separation distress, and sleep disruption. Symptoms began several months ago and include recurring nightmares about being lost, frequent fears about his mother’s safety, and excessive worry while at school. Dev reports feeling isolated due to bullying, claims physical symptoms like daily stomachaches and reduced appetite, and experiences ongoing nighttime enuresis: Focused SOAP Note for Anxiety, PTSD, and OCD.
He displays attachment concerns, avoids school, and shows difficulty concentrating. These symptoms have intensified following his father’s unexplained absence, which the family concealed as “vacation.” His mother reports a three-lb weight loss over the past three weeks and worsening functional impairment at home and school.
Substance Current Use: No reported use of substances.
Medical History:
Dev has been medically evaluated for his stomachaches, weight loss, and bedwetting; all physical causes were ruled out. He was prescribed DDAVP for enuresis with limited success.
- Current Medications: DDAVP for enuresis.
- Allergies: No known food or drug allergies.
- Reproductive Hx: Not applicable.
ROS:
- GENERAL: Reports fatigue, weight loss of three lbs, and poor appetite.
- HEENT: No visual or auditory complaints.
- SKIN: No rashes or lesions noted.
- CARDIOVASCULAR: No chest pain or palpitations.
- RESPIRATORY: No dyspnea, wheezing, or cough.
- GASTROINTESTINAL: Complaints of daily stomachaches; no vomiting or diarrhea.
- GENITOURINARY: Complaints of nighttime enuresis.
- NEUROLOGICAL: No dizziness, seizures, or paresthesia.
- MUSCULOSKELETAL: No joint/muscle pain.
- HEMATOLOGIC: No bleeding or bruising concerns.
- LYMPHATICS: No lymph node swelling was reported.
- ENDOCRINOLOGIC: No polydipsia or polyuria.
Objective:
Diagnostic Results:
No laboratory or imaging studies were ordered. The pediatric exam was unremarkable, ruling out medical etiologies for sleep and gastrointestinal complaints. The clinical interview and behavioral assessment align with DSM-5-TR criteria for anxiety-related disorders.
Dev’s functioning is impaired across multiple settings, such as home and school, supporting the need for psychiatric intervention. Standardized anxiety scales such as the Screen for Child Anxiety-Related Emotional Disorders may be utilized at follow-up for quantifying severity.
Assessment:
Mental Status Examination:
Dev is alert and cooperative during the interview, demonstrating engagement and appropriate responsiveness to questions. His speech is spontaneous, fluent, and consistent with developmental expectations for his age. Thought processes are organized, goal-directed, and logical, with no signs of derailment or tangential thinking.
His mood is anxious, and his affect is restricted but congruent with his emotional state. He denies any suicidal or homicidal ideation and shows no evidence of hallucinations or delusional thinking. Dev is oriented to person, place, and time, and his insight and judgment appear appropriate for his developmental level.
Diagnostic Impression:
Primary Diagnosis
The primary diagnosis is separation anxiety disorder (F93.0). Dev exhibits excessive and developmentally inappropriate fear of being separated from his mother, including constant worry about her safety and distress when apart. He experiences frequent nightmares about being lost, somatic symptoms such as stomachaches, and avoidance behaviors like refusing to attend school.
These symptoms have persisted for more than four weeks and significantly impair his daily functioning, especially in academic and social settings (Feriante et al., 2023). This clinical picture aligns with the DSM-5-TR diagnostic criteria for separation anxiety disorder.
Differential Diagnoses
- Post-Traumatic Stress Disorder, Preschool Subtype (F43.10):
The first differential diagnosis to consider is post-traumatic stress disorder, preschool subtype (F43.10). Dev’s ongoing nightmares and heightened sensitivity to perceived threats, such as intense fear when separated from his mother or when left in the dark, may reflect trauma-based anxiety. Although his symptoms mirror features common in post-traumatic stress disorder, a key diagnostic criterion is the child’s awareness of a life-threatening or traumatic event (Fariba & Gupta, 2024).
In Dev’s case, the loss of his father during military service has been concealed, and Dev has no conscious memory or understanding of the event. The absence of trauma processing, combined with a lack of dissociation or direct trauma reminders, makes post-traumatic stress disorder an unlikely primary diagnosis. However, further exploration of grief may be necessary as part of his therapeutic plan.
- Adjustment Disorder with Anxiety (F43.22):
The next possible diagnosis is adjustment disorder with anxiety (F43.22). Children frequently respond to stressful changes with emotional distress, especially when family dynamics shift. Dev’s symptoms might be viewed as a response to losing his father and changes in his mother’s availability following the birth of his younger sibling.
However, according to Geer (2023), adjustment disorder typically presents with less severity and tends to resolve within a short timeframe, particularly when support systems are strong. Dev’s symptoms have not only persisted for several months but also demonstrated escalation, with clear interference in academic and peer settings. Therefore, his symptom profile surpasses what would be expected for a normative adjustment reaction, suggesting that a more entrenched anxiety disorder is present.
- Obsessive-Compulsive Disorder (F42.9):
A third consideration is obsessive-compulsive disorder (F42.9). At first glance, Dev’s insistence on routines like sleeping with the door open or requiring a nightlight may resemble compulsions aimed at reducing distress. However, obsessive-compulsive disorder is typically defined by recurrent, intrusive thoughts or obsessions that provoke anxiety, followed by specific behaviors or rituals and compulsions intended to neutralize those fears (Nazeer et al., 2020).
Dev’s behaviors appear more rooted in attachment distress than in cognitive rituals. He does not describe intrusive thoughts, magical thinking, or distress about needing to perform actions in a certain way to prevent harm, which would be typical in pediatric obsessive-compulsive disorder. Given these distinctions, obsessive-compulsive disorder does not emerge as a strong diagnostic fit in this case.
Reflections:
If I could revisit this session, I would incorporate structured child-report tools like the Screen for Child Anxiety-Related Emotional Disorders to better capture Dev’s internal emotional experiences. These tools may help compensate for developmental limitations in verbal expression and offer greater insight into his anxiety severity. I would also initiate early collaboration with his teacher to understand how school dynamics contribute to his emotional distress.
Legal and Ethical Considerations
Dev must be given age-appropriate information about his father while ensuring that the mother has accepted and adjusted to her husband’s absence without negating her own needs. When making therapeutic disclosures, care should be given to the situation, and support must be provided (Pelacho-Rios & Bernabe-Valero, 2022). It is also important for clinicians to evaluate for emotional neglect since untreated conditions can damage Dev’s learning and emotional development.
Health Promotion and Disease Prevention
Encouraging routines and creating strategies that consider Dev’s feelings should be the main focus of health promotion. Creating calm bedtime habits and practicing children-oriented activities would help him relax and get more restful sleep. If symptoms are managed early, this lowers the chances of struggling in school and facing mental health concerns in the future.
Social Determinants of Health
Dev faces difficulties in life due to single parenthood, the possibility of economic struggles, and limitations in access to mental health care. His mother may find it challenging to go on with psychological care as a result of having many responsibilities or experiencing stigma. An effective way to deal with these challenges is by using a trauma-informed approach that takes into account both family and community resources.
Case Formulation and Treatment Plan:
Dev’s treatment plan is to start weekly trauma-informed play therapy and behavioral interventions that focus on children to help him relieve his anxiety and cope emotionally. Using parent-child interaction therapy, his parent can build better attachment and more stable behaviors at home. At the moment, medication is not needed; however, a pediatric psychiatric evaluation might be suggested if the therapy is not effective.
Structured bedtime strategies, friendship at school, and reliable communication from parents or caregivers will be used to help him deal with change and feel less stressed. Follow-up will involve close coordination with authorities involved in care, who will regularly evaluate the child’s progress and change interventions if required.
References
Fariba, K., & Gupta, V. (2024). Post-traumatic stress disorder in children. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559140/
Feriante, J., Bernstein, B., & Torrico, T. (2023). Separation anxiety disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560793/
Geer, K. (2023). Adjustment disorder. Primary Care: Clinics in Office Practice, 50(1), 83–88. https://doi.org/10.1016/j.pop.2022.10.006
Nazeer, A., Latif, F., Mondal, A., Azeem, M. W., & Greydanus, D. E. (2020). Obsessive-compulsive disorder in children and adolescents: Epidemiology, diagnosis and management. Translational Pediatrics, 9(S1), S76–S93. https://doi.org/10.21037/tp.2019.10.02
Pelacho-Rios, L., & Bernabe-Valero, G. (2022). The loss of a child, bereavement and the search for meaning: A systematic review of the most recent parental interventions. Current Psychology, 42. https://doi.org/10.1007/s12144-022-03703-w
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
In assessing patients with anxiety, obsessive-compulsive, and trauma and stressor-related disorders, you will continue the practice of looking to understand chief symptomology in order to develop a diagnosis. With a differential diagnosis in mind, you can then move to a treatment and follow-up plan that may involve both psychopharmacologic and psychotherapeutic approaches.
In this Assignment, you use a case study to develop a focused SOAP note based on evidence-based approaches.
Resources
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
To Prepare
- Review this week’s Learning Resources. Consider the insights they provide about assessing and diagnosing anxiety, obsessive compulsive, and trauma-related disorders.
- Review the Focused SOAP Note template, which you will use to complete this Assignment. There is also a Focused SOAP Note Exemplar provided as a guide for Assignment expectations.
- Review the video, Case Study: Dev Cordoba . You will use this case as the basis of this Assignment. In this video, a Walden faculty member is assessing a mock patient. The patient will be represented onscreen as an avatar.
- Consider what history would be necessary to collect from this patient.
- Consider what interview questions you would need to ask this patient.
Focused SOAP Note for Anxiety, PTSD, and OCD
Develop a Focused SOAP Note, including your differential diagnosis and critical-thinking process to formulate a primary diagnosis. Incorporate the following into your responses in the template:
- Subjective: What details did the patient provide regarding their chief complaint and symptomology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss the patient’s mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses with supporting evidence, listed in order from highest priority to lowest priority. Compare the DSM-5-TR diagnostic criteria for each differential diagnosis and explain what DSM-5 -TR criteria rules out the differential diagnosis to find an accurate diagnosis. Explain the critical-thinking process that led you to the primary diagnosis you selected. Include pertinent positives and pertinent negatives for the specific patient case.
- Plan: What is your plan for psychotherapy? What is your plan for treatment and management, including alternative therapies? Include pharmacologic and nonpharmacologic treatments, alternative therapies, and follow-up parameters, as well as a rationale for this treatment and management plan. Also incorporate one health promotion activity and one patient education strategy.
- Reflection notes: What would you do differently with this patient if you could conduct the session again? Discuss what your next intervention would be if you could follow up with this patient. Also include in your reflection a discussion related to legal/ethical considerations (demonstrate critical thinking beyond confidentiality and consent for treatment!), health promotion, and disease prevention, taking into consideration patient factors (such as age, ethnic group, etc.), PMH, and other risk factors (e.g., socioeconomic, cultural background, etc.).
- Provide at least three evidence-based, peer-reviewed journal articles or evidenced-based guidelines that relate to this case to support your diagnostics and differential diagnoses. Be sure they are current (no more than 5 years old).