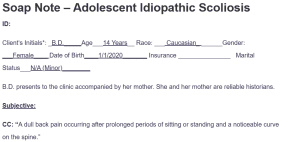
Soap Note – Adolescent Idiopathic Scoliosis
ID:
Client’s Initials*: _B.D._____Age___14 Years__ Race: ___ Caucasian_ ______Gender: ___Female____ Date of Birth____1/1/2020_______ Insurance _______________ Marital Status___N/A (Minor)________
B.D. presents to the clinic accompanied by her mother. She and her mother are reliable historians.
Subjective:
CC: “A dull back pain occurring after prolonged periods of sitting or standing and a noticeable curve on the spine.”
HPI:
B.D., a 14-year-old Caucasian female, presents to the clinic accompanied by her mother with a complaint of a noticeable curve in her spine. The mother reports that she first noticed the little curve around her thoracic region of the spine about six months ago. Since then, there have been not many changes, and she still has the curve. B.D. reports that the pain in her back feels like a dull ache, which majorly and primarily occurs after she has been standing or seated for a long time. She has a visible curvature and a rib hump on the side when she bends forward. She notes that the back pain and discomfort tend to get worse when she sits or stands for a prolonged period but gets better when she rests. Although she has had these symptoms for the last six months, she reports that she has not tried or received any treatments so far. She describes the pain as intermittent following activities she previously identified, such as sitting or standing for longer periods. B.D. denies any significant trauma or injury and reports no neurological symptoms such as numbness or tingling. She rates the pain as 3/10 on the 10-point pain scale. She reports that she is active in her school as a swimming team member. She has no history of tobacco, alcohol, or drug use.
Past Medical History:
- Medical problem list: No significant medical history.
- Preventative care: Up-to-date on vaccinations, including all childhood vaccines up-to her current age.
- Surgeries: None reported
- Hospitalizations: None reported
- LMP, pregnancy status, menopause, etc. for women: No reported LMP. No pregnancy.
Allergies:
Food- No known food allergies
Drug- No known drug allergies
Environmental- No known environmental allergies
Medications: The patient is currently not taking any prescribed or OTC medications.
Family History: The mother reports having mild scoliosis during her adolescence. No other reported joint disorders that run in the family.
Social History:
-Sexual history and contraception/protection: Not sexually active or history of contraception or protection use (Patient is a Minor)
-Chemical history (tobacco/alcohol/drugs): Denies tobacco, alcohol, and drug use
– Diet/Exercise: Takes a healthy diet. She is physically active and a member of the school’s swimming team
– Living arrangements: Currently lives with parents
– School/Work: Member of the school’s swimming team
– Developmental History: Met normal developmental milestones
– ADL: She is able to perform all her activities of daily living independently
ROS
- Constitutional: Reports no fevers or chills, no notable or significant changes in weight or skin pigmentation. She denies fatigue or episodes of general joint or muscle pain and weakness.
- Cardiovascular: Denies chest pain, abnormal heartbeats, dizziness, or fainting. No swelling of extremities, no claudication.
- Respiratory: Denies any shortness of breath, cough, or wheezing. No reported history of asthma or other respiratory conditions.
- Eyes: Denies any history of blurred vision, eye pain, or redness. No reported history of corrective lenses use or recent changes in visual acuity.
- Ears, Nose, Throat (ENT): No ear pain, tinnitus, or hearing loss. Denies nasal congestion or rhinorrhea. No sore throat, difficulty swallowing, or hoarseness. No history of ENT infections.
- Gastrointestinal: Denies nausea, vomiting, diarrhea, or constipation. No reported pain in the abdomen, bloating, or changes in appetite. Reports having regular bowel movements.
- Genitourinary: Denies blood in urine or changes in urinary frequency.
- Musculoskeletal: Reports dull discomfort, back pain, and a progressively visible spinal curvature. Denies joint pain, swelling, stiffness, or muscle weakness. No reported history of fractures or musculoskeletal injuries.
- Neurological: Denies experiencing headaches, dizziness, or numbness. Denies tingling, weakness in extremities, or changes in gait. No reported history of neurological conditions, including seizures or tremors.
- Skin: Denies itching or a history of skin infections, including eczema, rashes, discoloration, or lesions
- Psychiatric: Denies anxiety, depression, or significant mood changes. No history of psychiatric disorders. Maintains good academic performance in college, including physical activities such as swimming.
- Allergic/Immunologic: No known food, drug, or environmental allergies. Denies recurrent infections or history of autoimmune disorders.
- Hematologic/Lymphatic: Denies ease of bruising or bleeding. Denies history of anemia or lymph node infections
Objective
Vital Signs: HR: 72 beats per minute BP: 110/70 mmHg Temp: 98.6°F RR: 16 breaths per minute SpO2: 98% on room air Pain: 3/10
Height: 5 feet 4 inches Weight: 120 lbs
BMI: 20.6 (50th and 75th percentiles)
Labs, radiology or other pertinent studies:
- Orthopedic examination: Positive Adam’s forward bend test indicating possible scoliosis. Further diagnostic imaging has been ordered to confirm this observation
- X-ray: Ordered for the confirmation of the adolescent idiopathic scoliosis. Results pending
Physical Exam
- General: B.D. appears alert and oriented to the space, time, and context of the current visit. She physically appears as per her stated age. She has been cooperative and engaged throughout the examination. Her posture is slightly altered due to the curvature of her spine. The mother appears distressed due to the curvature of D.D.’s spine and is eager and open to recommendations for treatment.
- Head: Normocephalic and atraumatic. No tenderness of the scalp upon palpation.
- Neck: No lymphadenopathy or masses. Trachea midline. Full range of motion without pain. No jugular venous distention. The thyroid is non-palpable and non-tender.
- Eyes: Pupils Equal, Round, Reactive to Light and Accommodation. Extraocular movements are intact. No apparent visual deficits were noted during the exam.
- ENT: Normal appearing external ears, no deformities. Hearing is grossly intact in conversation. Nasal passages clear, no polyps observed. Mucous membranes moist and pink. Dentition in good condition. No ulcers or enlarged tonsils.
- Cardiovascular: Regular HR, 72 beats per minute, BP 110/70 mmHg, S1 and S2 audible without murmurs, rubs, or gallops. No bruits auscultated in the carotid arteries.
- Respiratory: RR 16 breaths per minute. lungs clear to auscultation bilaterally, no crackles, wheezes, or rhonchi. Breathing non-labored. A mild thoracic asymmetry noted due to the curvature without notable impairment of chest expansion.
- Gastrointestinal: Abdomen soft, non-tender, non-distended. Bowel sounds normoactive in all four quadrants.
- Musculoskeletal: Noticeable curvature of the spine noted on inspection with prominence of a hump on the side of thoracic rib when bending forward. No muscle or joint tenderness on palpation. Full range of motion in all extremities. No joint swelling or deformities.
- Neurological: Cranial nerves II-XII grossly intact. Sensation intact to light touch and temperature. Strength 5/5 in all extremities. No tremors or involuntary movements. Normal gait. Reflexes 2+ and symmetric in biceps, triceps, patellar, and Achilles tendons.
- Skin: Skin warm, dry, and intact. No rashes, lesions, or abnormal pigmentation.
- Lymphatic: No cervical, axillary, or inguinal lymphadenopathy. No palpable lymph nodes or tenderness in any lymphatic regions.
Assessment
Differentials
- Congenital Scoliosis (ICD-10: Q76.3):
- Congenital scoliosis is a possible diagnosis as it develops as a result of abnormal growth of the vertebral column during embryogenesis, leading to vertebral malformations present at birth and a spinal curvature (Bagheri et al., 2021). This means it is present from birth and can typically be identified earlier in life. Therefore, congenital scoliosis is often diagnosed early during infancy or early childhood. However, it can be ruled out in the case of B.D. as she is currently 14 years old. Her mother also noticed the curvature only 6 months ago. If this was a case of congenital scoliosis, it would have been identified by the time she was 5. Additionally, given the presented symptoms and considering her current and reported onset of the curvature, adolescent idiopathic scoliosis can be considered over rather than congenital scoliosis.
- Postural Kyphosis (ICD-10: M40.0):
- Postural kyphosis is another considerable diagnosis. The condition is majorly characterized by an exaggerated forward rounding of the back due to irregular and asymmetrical posture that deviates from normal alignment without structural constraints or generally poor posture (Zećirović et al., 2021). It is common in school-age children. However, it is ruled out in B.D.’s case as there is a visible rib hump confirmed through the Adam’s forward bend test and the specific lateral curvature observed. Such confirmed presentation are more aligned to and suggestive of scoliosis rather than kyphosis.
- Scheuermann’s Disease (Juvenile Kyphosis) (ICD-10: M42.0):
- Scheuermann’s disease can be considered as a possible diagnosis that leads to a noticeable curvature and back pain that is a result of it being a more rigid form of kyphosis that develops due to uneven vertebral growth (Sebaaly et al., 2022). However, it is dismissed in B.D.’s case rather than it being on the lateral plane (side bending), as with the various types of scoliosis, it is more pronounced in the sagittal plane (forward bending). Additionally, a rib hump was observed in B.D. during the Adam’s forward bend test, which aligns with scoliosis.
Diagnosis
- Adolescent Idiopathic Scoliosis (ICD-10: 124)
The primary diagnosis is adolescent idiopathic scoliosis. This diagnosis is based on the symptoms and history that the patient presented, as well as Adam’s forward bend test examination. However, the other differentials can be considered because they present overlapping manifestations. However, considering specific aspects of the symptoms, B.D. presents such as the type of curvature, the presence of a rib hump, her age, timing, and the onset of the symptoms, rule out the other diagnoses making idiopathic scoliosis the more likely primary diagnosis.
Plan
Diagnostic Studies:
Spinal X-ray to confirm the diagnosis of scoliosis (Kuznia et al., 2020). The patient will also be referred to an orthopedic specialist for a more comprehensive diagnosis of scoliosis and the development of a more specialized management plan.
Treatment:
Physical therapy, upon the confirmation of scoliosis, will be utilized to improve the patient’s muscle imbalances and improve posture. The patient will also be provided information on other possible methods of managing the condition upon confirmation, including back brace and surgery (Addai et al., 2020; Grivas et al., 2022)
Patient Education:
The patient and her mother were educated on:
- Adolescent idiopathic scoliosis and possible and available treatment options.
- The need for regular follow-up in monitoring the progression of the condition and allow for any corrections and adjustments for the selected treatment modality.
- Importance of maintaining a good posture and strength training for back muscles
- Self-care is an important aspect of managing the condition (Dufvenberg et al., 2021)
- The patient was also advised to continue with her swimming exercises
- The patient was also educated on various aspects of treating and management of adolescent idiopathic scoliosis including:
- Surgery as a corrective approach has the possibility of serious complications (Al-Mohrej et al., 2020) and related post-surgical pain and related experiences (Navarrete-Zampaña et al., 2019). In this, the patient and the mother were more enlightened on the possible complications related to the use of surgery as a treatment of scoliosis if confirmed, and the current capacity of the healthcare provider to manage such complications if need be. They were also educated on approaches to manage and control post-surgical pain through improved self-care strategies and the available post-surgical support.
- The use of brace treatment for the scoliosis if confirmed. The patients were educated on the possible risk factors that can lead to the braces failing to correct the curvature including removing the braces early, accelerated physical growth of the patient, and poor bone development (Hawary et al., 2019). The patient and the mother were educated on how to manage the braces in case they chose to use braces for correcting the curvature.
Follow-up Plan:
- Patient to return to the clinic in 4 weeks
- Follow-up to focus on evaluating the patient’s response to the interventions and adjust the treatment plan as necessary.
- Patient to be referred to a scoliosis specialist based on results of the X-ray
- The patient and mother were referred to a mental health support program (Essex et al., 2022).
The diagnosis and treatment of adolescent idiopathic scoliosis has a substantial physical and mental health impact on adolescents and their families.
References
Addai, D., Zarkos, J., & Bowey, A. J. (2020). Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Child’s Nervous System, 36(6), 1111–1119. https://doi.org/10.1007/S00381-020-04608-4/TABLES/1
Bagheri, F., Razi, A., Birjandinejad, A., Amel Farzad, S., Peivandi, M. T., & Habibzade Shojaei, S. R. (2021). Congenital Scoliosis: A Current Concepts Review. Journal of Pediatrics Review, 9(2), 127–136. https://doi.org/10.32598/JPR.9.2.876.1
Dufvenberg, M., Diarbakerli, E., Charalampidis, A., Öberg, B., Tropp, H., Ahl, A. A., Möller, H., Gerdhem, P., & Abbott, A. (2021). Six-Month Results on Treatment Adherence, Physical Activity, Spinal Appearance, Spinal Deformity, and Quality of Life in an Ongoing Randomised Trial on Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS). Journal of Clinical Medicine 2021, Vol. 10, Page 4967, 10(21), 4967. https://doi.org/10.3390/JCM10214967
Essex, R., Bruce, G., Dibley, M., Newton, P., Thompson, T., Swaine, I., & Dibley, L. (2022). A systematic scoping review and textual narrative synthesis of the qualitative evidence related to adolescent idiopathic scoliosis. International Journal of Orthopaedic and Trauma Nursing, 45, 100921. https://doi.org/10.1016/J.IJOTN.2022.100921
Grivas, T. B., Negrini, S., Aubin, C. E., Aulisa, A. G., De Mauroy, J. C., Donzelli, S., Hresko, M. T., Kotwicki, T., Lou, E., Maruyama, T., Parent, E. C., Rigo, M., Thometz, J. G., Wong, M. S., & Zaina, F. (2022). Nonoperative management of adolescent idiopathic scoliosis (AIS) using braces. Prosthetics and Orthotics International, 46(4), 383–391. https://doi.org/10.1097/PXR.0000000000000117
Kuznia, A. L., Hernandez, A. K., & Lee, L. U. (2020). Adolescent Idiopathic Scoliosis: Common Questions and Answers. American Family Physician, 101(1), 19–23. https://www.aafp.org/pubs/afp/issues/2020/0101/p19.html
Sebaaly, A., Farjallah, S., Kharrat, K., Kreichati, G., & Daher, M. (2022). Scheuermann’s kyphosis: update on pathophysiology and surgical treatment. EFORT Open Reviews, 7(11), 782–791. https://doi.org/10.1530/EOR-22-0063
Zećirović, A., Bjelica, B., Pajović, L., & Aksović, N. (2021). Postural Status And Kyphosis In School-Age Children. International Journal of Academic Health and Medical Research, 11, 90. www.ijeais.org/ijahmr
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
SOAP NOTE Instructions
- Create a pretend SOAP NOTE on a pediatric patient (teenager with idiopathic scoliosis)
Some details I can share is below:
B.D. is a 14-year-old Caucasian female who presents to the clinic with her mother, concerned about a noticeable curve in her spine.
- Onset: The curvature was first noticed by her mother approximately six months ago.
- Location: The curvature is observed in the thoracic region of the spine.
- Duration: The condition has been present for about six months.
- Characteristics/Context: B.D. describes the back pain as a dull ache, primarily occurring after prolonged periods of sitting or standing. The curvature is visible, and there is a rib hump noted on the right side during the Adam’s forward bend test.
- Aggravating Factors: Prolonged sitting or standing seems to exacerbate the back pain.
- Relieving Factors: Rest alleviates the discomfort.
- Treatment: No treatments have been tried yet.
- Timing: The back pain is intermittent, occurring mainly after activities that involve extended periods of sitting or standing.
- Severity: The pain is mild, rated as 3/10 on the pain scale.
C.D. denies any significant trauma or injury and reports no neurological symptoms such as numbness or tingling. She is active in her school swimming team and has no history of tobacco, alcohol, or drug use.
Past Medical History (PMH):
J.D. has no significant medical history. She is up-to-date on vaccinations. She has had no surgeries or hospitalizations. She has no known drug, food, or environmental allergies and takes no medications.
Family History (FH):
Her mother had mild scoliosis during her adolescence.
Social History (SH):
J.D. is active in her school swimming team. She denies any use of tobacco, alcohol, or drugs.
Review of Systems (ROS):
Constitutionally, J.D. denies experiencing fever, chills, weight loss, or fatigue. Musculoskeletally, she reports back pain and visible spinal curvature but denies joint pain or muscle weakness. Neurologically, she denies experiencing headaches, dizziness, or numbness. Psychiatrically, she denies experiencing depression or anxiety.
Emotional and Mental Status:
J.D. appears to be a well-adjusted adolescent with no signs of emotional distress or mental health concerns. She is cooperative and engaged during the consultation.
Patient’s Beliefs and Preferences:
J.D. and her mother are concerned about the spinal curvature and are eager to explore treatment options. They have not tried any treatments yet and are open to recommendations.
Objective:
– Vital Signs:
– Blood Pressure: 110/70 mmHg [Normal: 90-120/60-80 mmHg]
– Heart Rate: 72 beats per minute [Normal: 60-100 beats per minute]
– Respiratory Rate: 16 breaths per minute [Normal: 12-20 breaths per minute]
– Temperature: 98.6°F [Normal: 97.8-99.0°F]
– Oxygen Saturation: 98% on room air [Normal: 95-100%]
– General Appearance:
– J.D. is alert and oriented, appears her stated age. She is cooperative and engaged during the examination.
– Physical Examination:
– Head, Eyes, Ears, Nose, Throat (HEENT): Normocephalic, atraumatic, pupils equal, round, reactive to light and accommodation. No erythema or discharge in the ears or nose. Throat is clear.
– Cardiovascular: Regular rhythm, no murmurs, rubs, or gallops. Peripheral pulses are 2+ bilaterally.
– Respiratory: Clear to auscultation bilaterally, no wheezes, rales, or rhonchi.
– Gastrointestinal: Abdomen soft, non-tender, non-distended. Bowel sounds present in all quadrants.
– Musculoskeletal: Noticeable curvature of the spine noted on inspection. No tenderness on palpation. Full range of motion in all extremities. No joint swelling or deformities.
– Neurological: Cranial nerves II-XII grossly intact. Sensation intact to light touch. Strength 5/5 in all extremities. No tremors or involuntary movements.
– Skin: Warm, dry, and intact. No rashes, lesions, or abnormal pigmentation.
– Height and Weight:
– Height: 5 feet 4 inches [Normal for age]
– Weight: 120 lbs [Normal for age]
– Wound or Incision Assessment: Not applicable.
– Specialized Examinations:
– Orthopedic examination: Positive Adam’s forward bend test indicating possible scoliosis. Further diagnostic imaging recommended.
– Diagnostic Test Results:
– Pending: X-ray of the spine for definitive diagnosis of scoliosis.
– Monitoring Devices: Not applicable.
Assessment:
Diagnosis: Based on the patient’s history, physical examination, and positive Adam’s forward bend test, the preliminary diagnosis is Adolescent Idiopathic Scoliosis.
Clinical Impression: B.D. is a 14-year-old female with a noticeable curvature of the spine, which was first observed by her mother six months ago. The patient reports mild, intermittent back pain that worsens with prolonged sitting or standing. The patient denies any neurological symptoms and has no significant past medical history. Family history is notable for mild scoliosis in the mother. The patient is active in her school swimming team and denies any use of tobacco, alcohol, or drugs. Physical examination reveals a visible curvature of the spine in the thoracic region and a rib hump on the right side. The patient’s vital signs are within normal limits.
Analysis of Findings: The patient’s age, the visible curvature of the spine, and the positive Adam’s forward bend test are indicative of Adolescent Idiopathic Scoliosis. The patient’s mild, intermittent back pain is likely related to her scoliosis. The absence of neurological symptoms such as numbness or tingling is a good sign, indicating that there is likely no nerve compression at this time.
Severity and Complexity: The severity of the scoliosis and its impact on the patient’s daily activities will need to be further evaluated with an X-ray of the spine. The complexity is moderate given the need for ongoing monitoring, potential treatment options, and the impact on the patient’s quality of life.
Multidisciplinary Considerations: Management of Adolescent Idiopathic Scoliosis may involve a multidisciplinary team including an orthopedic specialist, physical therapist, and potentially a psychologist to address any emotional distress related to the diagnosis and its impact on the patient’s life.
Response to Interventions: No interventions have been tried yet. The patient and her mother are open to treatment recommendations.
Soap Note – Adolescent Idiopathic Scoliosis
For B.D., a 14-year-old female with a noticeable spinal curvature and mild back pain, here are three differential diagnoses along with explanations for why they are considered differentials rather than the primary diagnosis:
- Postural Kyphosis:
- Explanation: Postural kyphosis is characterized by an exaggerated forward rounding of the back, often due to poor posture. It is more flexible and can be corrected with postural adjustments. In B.D.’s case, the presence of a rib hump during the Adam’s forward bend test and the specific lateral curvature observed suggest scoliosis rather than kyphosis. Postural kyphosis typically does not present with a rib hump, which is more indicative of scoliosis.
- Scheuermann’s Disease (Juvenile Kyphosis):
- Explanation: Scheuermann’s disease involves a more rigid form of kyphosis due to uneven vertebral growth, leading to a noticeable curvature and back pain. While it can occur in adolescents, the curvature in Scheuermann’s is typically more pronounced in the sagittal plane (forward bending) rather than the lateral plane (side bending), which is more characteristic of scoliosis. Additionally, the rib hump observed in B.D. is more aligned with scoliosis.
- Congenital Scoliosis:
- Explanation: Congenital scoliosis results from vertebral malformations present at birth, leading to spinal curvature. It is typically identified earlier in life, often during infancy or early childhood, rather than first being noticed at age 14. B.D.’s presentation aligns more with adolescent idiopathic scoliosis, which is common during the growth spurt before puberty, rather than congenital scoliosis, which would likely have been detected earlier.
These differentials are considered because they share some overlapping symptoms with idiopathic scoliosis, such as spinal curvature and back pain. However, the specific characteristics of B.D. presentation, including the age of onset, the type of curvature, and the presence of a rib hump, make idiopathic scoliosis the more likely primary diagnosis. Further evaluation, including imaging, would help confirm the diagnosis and rule out these differentials.
Plan:
Therapeutic Interventions:
1. Order an X-ray of the spine for definitive diagnosis (ICD-10 code Z12.39).
2. If scoliosis is confirmed (ICD-10 code M41.9), refer to an orthopedic specialist for further evaluation and treatment planning.
3. Recommend physical therapy for back pain (ICD-10 code M54.5) and to improve posture.
Diagnostic Studies:
1. Spinal X-ray to confirm the diagnosis of scoliosis.
Referrals and Consultations:
1. Referral to an orthopedic specialist if the diagnosis of scoliosis is confirmed.
Patient Education and Counseling:
1. Educate the patient and her mother about scoliosis, its potential causes, and treatment options.
2. Discuss the importance of regular follow-up visits to monitor the progression of the condition.
3. Counsel the patient on the importance of maintaining good posture and participating in exercises that strengthen the back muscles.
Self-Care and Lifestyle Modifications:
1. Advise the patient to continue with her swimming activities as it can help strengthen the back muscles.
2. Encourage the patient to take breaks during long periods of sitting or standing to alleviate back pain.
Collaboration and Coordination:
1. Coordinate with the orthopedic specialist and physical therapist to ensure a comprehensive and effective treatment plan for the patient.
Emergency or Contingency Plans:
1. Instruct the patient and her mother to seek immediate medical attention if the back pain significantly worsens or if the patient develops any neurological symptoms such as numbness or tingling.
Follow-up Plan:
1. Schedule a follow-up appointment in 4 weeks to evaluate the patient’s response to the interventions and adjust the treatment plan as necessary.
PLEASE KINDLY USE THE INITIAL B.D. ON THE HISTORY OF PRESENT ILLNESS SECTION. THE REST. PLEASE USE the word “patient” instead of the initial B.D.
PLEASE MAKE SURE TO PUT THE APA 7 REFERENCES CORRECTLY. PLEASE PUT INTEXT CITATIONS ON PLANS AND TREATMENT
THIS IS A FOCUS SOAP NOTE SO PLEASE ONLY INCLUDE WHAT IS PERTINENT
PLEASE CHECK TO MAKE IT PLAGIARISM FREE
PLEASE USE THE TEMPLATE ATTACHED TO CREATE SOAP NOTE
PLEASE USE A TITLE PAGE AND DO NOT PUT THE LOGO OF THE SCHOOL
THANKS A LOT

