The Use of Clinical Systems to Improve Outcomes and Efficiencies
The technological era has ushered in a path toward effectiveness, efficiency, and convenience. In the healthcare sector, emerging technologies are increasingly shaping healthcare operationalization, with the focus being to enhance care delivery. Health information technologies are front runners in enhancing the efficiency and effectiveness of modern healthcare. Premised on patient-centeredness and convenience, these technologies are valuable in various healthcare engagements. Their ability to ease information flow, optimize care processes, and contribute towards quality enhancement measures makes them critical in patient care. As research continues to advance and configure the contemporary care landscape, further innovations are necessitated to better current global healthcare. This paper annotates four resources on the impact of clinical systems on outcomes and efficiency within the context of nursing. Do you need help with your assignment?
El Asmar, M. line, Dharmayat, K. I., Vallejo-Vaz, A. J., Irwin, R., & Mastellos, N. (2021). Effect of computerized, knowledge-based, clinical decision support systems on patient-reported and clinical outcomes of patients with chronic disease managed in primary care settings: A systematic review. BMJ Open, 11(12). https://doi.org/10.1136/bmjopen-2021-054659
This paper interrogates the effects of clinical systems on the clinical outcomes of patients with chronic illnesses under management in primary care settings. It is a systematic review article that summarizes the effects of computerized clinical decision support systems (C-CDSS) incorporated into EHR systems on patient-reported clinical outcomes of patients with chronic illnesses managed in outpatient care settings. Per the authors, several findings highlight the effectiveness of C-CDSS in EHR systems in improving clinical outcomes for patients with chronic illnesses presenting for outpatient care. C-CDSS and EHR systems are knowledge-based systems that generate actionable clinical-oriented patient-based outputs. These outputs are often in the form of recommendations. They help in clinical decision-making processes by giving caregivers care options to choose from. Besides, their ability to store and facilitate the flow of health information makes them valuable in minimizing medical errors by synchronizing current and past findings on the patients. C-CDSS incorporated in electronic health records remains valuable in chronic care. Besides guiding clinical decision-making processes, clinically meaningful improvements were noted in patients with chronic illnesses managed using these systems. These findings affirm the value of these systems in chronic care. Despite their effectiveness in improving the clinical outcomes for patients with chronic illnesses being managed via outpatient care, there is inconclusive evidence supporting the integration of CDSS in the EHR system. The authors further postulate that there is a need for more studies to further examine how CDSS in EHR can be better leveraged to improve chronic care in outpatient settings.
Upadhyay, S., & Hu, H. (2022). A qualitative analysis of the impact of electronic health records (EHR) on healthcare quality and safety: Clinicians’ lived experiences. Health Services Insights, 15, 117863292110707. https://doi.org/10.1177/11786329211070722
This article details the impact of electronic health records (EHRs) on the quality and safety of healthcare. It is a qualitative analysis paper aimed at exploring clinicians’ experiences with the system and the role of the EHR system in improving the quality and safety of healthcare. The authors note that EHR systems maintain effectiveness in enhancing the efficiency of healthcare operationalizations. The use of these systems has been implicated in a considerable reduction in medical and medication errors by improving data availability and accessibility as well as improved coordination of care between nurses and other caregivers. From the caregiver’s viewpoint, optimizing the use of these systems, as well as addressing intrinsic challenges presented with the use of the system, may provide a better guarantee of quality and safe healthcare. This paper was centered on safety and quality improvement in healthcare. It sought to address safety and quality gaps in the resolve to enhance care delivery. Findings from the paper affirm the need to adopt clinical systems and detail their value in improving clinical outcomes. By optimizing the use of EHR systems, care organizations and caregivers can better guarantee the safety of their patients and also ensure they receive high-quality care.
Uslu, A., & Stausberg, J. (2021). Value of the electronic medical record for hospital care: Update from the literature. Journal of Medical Internet Research, 23(12). https://doi.org/10.2196/26323
This article is premised on EHR use in hospital care and its essentiality in improving clinical outcomes and care efficiencies. The article is a scoping review that compiles empirical studies on the value of electronic medical records (EMR) in hospital care. Per the authors’ summary and compilation, electronic medical records remain relevant and valuable in contemporary healthcare. In addition to their economic advantages, these systems considerably improve the quality of hospital care, translating to better clinical outcomes, as demonstrated by shortened hospital stay days, reduced readmissions, and minimized hospital visitations. They also help in improving the efficiency of care processes in the hospital setup. As hospital care approaches tend towards patient-centeredness and quality care, integrating these systems into hospitals’ framework of operationalizations is necessitated for a better assurance of improved outcomes. This paper affirms the need for and the value of EMR in hospital care. EMR is a patient-oriented health information technology that facilitates easy flow of health information. These systems are impactful in improving clinical outcomes in hospital setups.
Vos, J. F., Boonstra, A., Kooistra, A., Seelen, M., & van Offenbeek, M. (2020). The influence of electronic health record use on collaboration among medical specialties. BMC Health Services Research, 20(1). https://doi.org/10.1186/s12913-020-05542-6
This article is premised on healthcare collaborations as a pathway towards enhancing the efficiency and effectiveness of care and a means towards improving clinical outcomes. It is aimed at examining how EHR systems facilitate and constrain healthcare collaborations at various points of care. Collaborative paradigms synchronize care processes with the patients. They are a means towards efficient care as they ensure that all specialties involved in patient care have a common goal of improving the outcomes of the patients. Centered on the principles of sound healthcare communications, teamwork, and accountability, this approach considerably improves care outcomes and patient experiences. Integral to the collaborative paradigm is information flow and sharing. EHR systems improve the flow of health information and sharing by ensuring that all specialties involved in the care processes get timely and accurate information about the patients. This helps in synchronizing care processes for the patients. EHR’s collaborative affordances are thus the cornerstone of comprehensive and quality care. A prerequisite to the use of EHR in collaborative care, however, is behavioral, organizational, and technical adaptations to these systems. The establishment of hospital policies that trust the use of EHR as part of the collaborative paradigm is a better way to guarantee efficient coordination of care for patients. This paper details several aspects of EHR use in collaborative care. Premised on the need to enhance care efficiency, it gives care organizations and caregivers an option of using health information technologies such as EHR to improve information flow among caregivers involved in patient care.
Conclusion
The annotated articles detail the use of various clinical systems in care operationalization. Clinical systems such as EMR and CDSS are valuable in healthcare. They enhance the efficiency and effectiveness of care processes and improve clinical outcomes. As evident in these sources, these technologies can be leveraged in wide clinical settings to optimize care processes. In the resolve to enhance the quality of healthcare and optimize clinical outcomes, leveraging these technologies provides a guarantee of enhanced safety and overall improvements in patient outcomes. Their implementation, however, is dependent on how well caregivers adapt to their functionality and embrace their use. As postulated by Vos et al., technical, behavioral, and organizational adaptations are required for the successful implementation of these systems. With increasing evidence of their effectiveness and adoption of these systems, expanding the knowledge base on the technicalities involved with the use of these systems is necessitated. This supports further and additional research on the impact of these systems on patient care and clinical outcomes.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
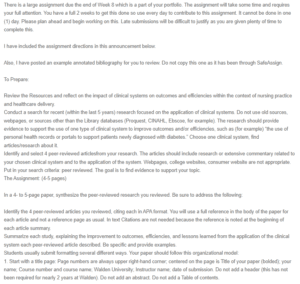
There is a large assignment due the end of Week 8 which is a part of your portfolio. The assignment will take some time and requires your full attention. You have a full 2 weeks to get this done so use every day to contribute to this assignment. It cannot be done in one (1) day. Please plan ahead and begin working on this. Late submissions will be difficult to justify as you are given plenty of time to complete this.
The Use of Clinical Systems to Improve Outcomes and Efficiencie
I have included the assignment directions in this announcement below.
Also, I have posted an example annotated bibliography for you to review. Do not copy this one as it has been through SafeAssign.
To Prepare:
Review the Resources and reflect on the impact of clinical systems on outcomes and efficiencies within the context of nursing practice and healthcare delivery.
Conduct a search for recent (within the last 5 years) research focused on the application of clinical systems. Do not use old sources, webpages, or sources other than the Library databases (Proquest, CINAHL, Ebscoe, for example). The research should provide evidence to support the use of one type of clinical system to improve outcomes and/or efficiencies, such as (for example) “the use of personal health records or portals to support patients newly diagnosed with diabetes.” Choose one clinical system, find articles/research about it.
Identify and select 4 peer-reviewed articlesfrom your research. The articles should include research or extensive commentary related to your chosen clinical system and to the application of the system. Webpages, college websites, consumer website are not appropriate. Put in your search criteria: peer reviewed. The goal is to find evidence to support your topic.
The Assignment: (4-5 pages)
In a 4- to 5-page paper, synthesize the peer-reviewed research you reviewed. Be sure to address the following:
Identify the 4 peer-reviewed articles you reviewed, citing each in APA format. You will use a full reference in the body of the paper for each article and not a reference page as usual. In text Citations are not needed because the reference is noted at the beginning of each article summary.
Summarize each study, explaining the improvement to outcomes, efficiencies, and lessons learned from the application of the clinical system each peer-reviewed article described. Be specific and provide examples.
Students usually submit formatting several different ways. Your paper should follow this organizational model:
1. Start with a title page: Page numbers are always upper right-hand corner; centered on the page is Title of your paper (bolded); your name; Course number and course name; Walden University; Instructor name; date of submission. Do not add a header (this has not been required for nearly 2 years at Walden). Do not add an abstract. Do not add a Table of contents.
2. On the second page add a Level 1 heading: Title of your paper (this first heading is bolded).
3. The first paragraph is the introduction to your topic. Include the main points to be found in your paper. Include a purpose statement: The purpose of this paper is…..
4. Body of the paper: Begin with each full reference; Left justified (Same as a Level 2 heading. Indent all lines after the first line. Then begin a new paragraph, which is the summary of your first article. In text citations are not necessary in an annotated bibliography because it is assumed all information came from the one source. However, if you use direct quotes (which I highly urge you not to), please add the proper formatted direct quote. Repeat this for every source you are summarizing.
5. The final paragraph is the conclusion. Heading: Conclusion (left justified or centered). The conclusion is a summary and reminds the reader of the main points. There is no new content added to a conclusion paragraph.
6. Lastly, Reference page. There is no reference page. All full references should be noted in the body of the paper.
Additional basic APA tips: Double space only; font is Times New Roman, size 12; page numbers on every page, upper right-hand corner; NEVER add an author’s full first name or the academic credentials in a reference- last name and initials only. Look at the APA text, the library sources, or to PurdueOwl website.
New technology—and the application of existing technology—only appears in healthcare settings after careful and significant research. The stakes are high, and new clinical systems need to offer evidence of positive impact on outcomes or efficiencies.
Nurse informaticists and healthcare leaders formulate clinical system strategies. As these strategies are often based on technology trends, informaticists and others have then benefited from consulting existing research to inform their thinking.
In this Assignment, you will review existing research focused on the application of clinical systems. After reviewing, you will summarize your findings.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare:
Review the Resources and reflect on the impact of clinical systems on outcomes and efficiencies within the context of nursing practice and healthcare delivery.
Conduct a search for recent (within the last 5 years) research focused on the application of clinical systems. The research should provide evidence to support the use of one type of clinical system to improve outcomes and/or efficiencies, such as “the use of personal health records or portals to support patients newly diagnosed with diabetes.”
Identify and select 4 peer-reviewed research articles from your research.
For information about annotated bibliographies, visit https://academicguides.waldenu.edu/writingcenter/assignments/annotatedbibliographiesLinks to an external site.
The Assignment: (4-5 pages not including the title and reference page)

