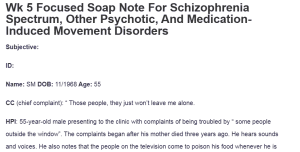
Wk 5 Focused Soap Note For Schizophrenia Spectrum, Other Psychotic, And Medication-Induced Movement Disorders
Subjective:
ID:
Name: SM DOB: 11/1968 Age: 55
CC (chief complaint): “ Those people, they just won’t leave me alone.
HPI: 55-year-old male presenting to the clinic with complaints of being troubled by “ some people outside the window”. The complaints began after his mother died three years ago. He hears sounds and voices. He also notes that the people on the television come to poison his food whenever he is watching and that he tricks them and locks everything in the fridge: Wk 5 Focused Soap Note For Schizophrenia Spectrum, Other Psychotic, And Medication-Induced Movement Disorders.
Substance Current Use: The patient smokes three packs of cigarettes per day. He also drinks alcohol. Denies using cocaine, marijuana, or other illicit substances
PMH: The patient is a known diabetic. He was suspected to be having a fatty liver.
Medical History:
- Current Medications: Metformin for the management of diabetes and Seroquel. He has tried Haldol, Thorazine, and risperidone.
- Allergies:No known drug or food allergies
Family and Social: The patient was raised by his mother and sister. The patient has never been married before and has no children and his highest level of education is tenth grade. His dad was rough on him till his death. His dad was diagnosed with schizophrenia.
ROS:
- GENERAL: The patient is alert. Denies weight loss, or weight gain.
- HEENT: Denies head visual and hearing loss, nasal congestion, or difficulty swallowing.
- SKIN: demies skin scars, lesions or color changes,
- CARDIOVASCULAR: Denies palpitation or chest pain.
- RESPIRATORY: Denies shortness or breath or wheezing.
- GASTROINTESTINAL: Denies bowel movement inconsistencies.
- GENITOURINARY: Denies incontinence.
- NEUROLOGICAL: Denies seizures or blackouts.
- ENDOCRINOLOGIC: Denies heat or cold intolerance. The patient is diabetic.
Objective:
Vital signs: Temp- 98.6 P- 86 RR 20 120/70 Ht 5’2 Wt 126lbs
Diagnostic results: A urinary toxicological screen to rule out possible intoxicants, along with the thyroid panel and CBC, may be necessitated. This may help eliminate thyroid disease, drug use, and other organic causes of psychosis (Orsolini et al., 2022).
Assessment:
Mental Status Examination: The patient is poorly oriented to the place, time, and event of the day and disheveled. He is also responsive to the questions asked. He, however, displays disorganized thought patterns and responds inappropriately to some interview questions asked. The patient is delusional and demonstrates persecutory delusions by claiming people outside the window are coming for him.
He also manifests with visual and auditory hallucinations. His affect is blunt. There are no signs of memory loss. The patient also denies any self-harm behaviors such as suicide ideations and tendencies.
Diagnostic Impression:
Differential diagnoses;
- Schizophrenia: The presence of hallucinations, delusions, blunted affect, and disorganized thought patterns warranted the inclusion of this differential. A positive substance use history, family history of the disorder, and history of early childhood trauma also pointed toward the diagnosis (DSM-V, n.d.).
- Schizophreniform disorder: The presence of psychotic symptoms warranted the inclusion of this differential. Schizophreniform disorder is, however, limited, often lasting less than six months or less (DSM-V, n.d.). This made the differential less probable.
- Substance-induced psychotic disorder: The presence of psychotic manifestations alongside substance use warranted the inclusion of this differential. Notwithstanding, the onset of the psychotic symptoms cannot be traced to drug use. This makes this diagnosis less probable (Fiorentini et al., 2021).
Diagnosis: The presumptive diagnosis is schizophrenia disorder.
Case Formulation and Treatment Plan:
The patient will be continued on quetiapine 50mg administered orally at bedtime. Quetiapine is a second-generation antipsychotic effective in alleviating symptoms (Rubio & Kane, 2022). He will be educated on the medication including common side effects, such as weight gain, dry mouth, and constipation (Makary et al., 2023). He will be advised to return to the clinic after two weeks to monitor his response to therapy.
Reflections: The case is of a 55-year-old male with possible schizophrenia. One thing I would do differently when managing the client is to order diagnostics such as the urine toxicological screen to rule out other causes of psychosis. During follow up I would inquire about the patient self care capabilities to determine the need for incarceration.
A legal consideration for the patient is competence as caregivers should provide the best care to the patient while recognizing apparent deficiencies in his cognitive and mental functioning. As a point of health promotion, the family will be involved in care and educated on the disease process to enhance their ability to care for their kin.
References
DSM-V. (n.d.). DSM. Psychiatry.org – DSM. https://www.psychiatry.org/psychiatrists/practice/dsm
Fiorentini, A., Cantù, F., Crisanti, C., Cereda, G., Oldani, L., & Brambilla, P. (2021). Substance-induced psychoses: An updated literature review. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.694863
Makary, S., Abd El Moez, K., Elsayed, M., & Hassan, H. (2023). Second-generation antipsychotic medications and metabolic disturbance in children and adolescents. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery, 59(1). https://doi.org/10.1186/s41983-023-00612-y
Orsolini, L., Pompili, S., & Volpe, U. (2022). Schizophrenia: A narrative review of etiopathogenetic, Diagnostic and treatment aspects. Journal of Clinical Medicine, 11(17),5040. https://doi.org/10.3390/jcm11175040
Rubio, J. M., & Kane, J. M. (2022). The pharmacological treatment of schizophrenia: How far have we come? Psychiatry and Clinical Neurosciences Reports, 1(2). https://doi.org/10.1002/pcn5.13
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
In two pages, develop a focused SOAP note, including your differential diagnosis and critical-thinking process to formulate a primary diagnosis. Incorporate the following into your responses in the template:
- Subjective: What details did the patient provide regarding their chief complaint and symptomology to derive your differential diagnosis? What is the duration and severity of their symptoms? How are their symptoms impacting their functioning in life?
- Objective: What observations did you make during the psychiatric assessment?
- Assessment: Discuss the patient’s mental status examination results. What were your differential diagnoses? Provide a minimum of three possible diagnoses with supporting evidence, and list them in order from highest priority to lowest priority.
Compare the DSM-5-TR diagnostic criteria for each differential diagnosis and explain what DSM-5-TR criteria rules out the differential diagnosis to find an accurate diagnosis. Explain the critical-thinking process that led you to the primary diagnosis you selected. Include pertinent positives and pertinent negatives for the specific patient case.Wk 5 Focused Soap Note For Schizophrenia Spectrum, Other Psychotic, And Medication-Induced Movement Disorders
- Plan: What is your plan for psychotherapy? What is your plan for treatment and management, including alternative therapies? Include pharmacologic and nonpharmacologic treatments, alternative therapies, and follow-up parameters, as well as a rationale for this treatment and management plan. Also incorporate one health promotion activity and one patient education strategy.
- Reflection notes: What would you do differently with this patient if you could conduct the session again? Discuss what your next intervention would be if you were able to follow up with this patient. Also include in your reflection a discussion related to legal/ethical considerations (demonstrate critical thinking beyond confidentiality and consent for treatment!), health promotion, and disease prevention, taking into consideration patient factors (such as age, ethnic group, etc.), PMH, and other risk factors (e.g., socioeconomic, cultural background, etc.).
- Provide at least three evidence-based, peer-reviewed journal articles or evidenced-based guidelines that relate to this case to support your diagnostics and differential diagnoses. Be sure they are current (no more than 5 years old).
Case study video link is below, use to complete assignment.
Case study: Sherman Tremaine. Walden University Canvas. https://waldenu.instructure.com
Resources:
- Case Study: Sherman Tremaine (See Attached Transcript)
- Zakhari, R. (2020). The psychiatric-mental health nurse practitioner certification review manual. Springer.
- Kaplan & Sadock’s synopsis of psychiatry