The Use of Technology in Healthcare
Meaningful use of technology in the healthcare setting has numerous merits. Healthcare technology improves the quality of healthcare services and patient safety. This is accomplished by optimizing care coordination. Care coordination is achieved by an appropriate delegation of tasks among members of the interdisciplinary team (Schmutz et al., 2019). Patient safety is also improved via the automation of functions and reduced human errors in healthcare. All stakeholders should work in concert to acquire and implement appropriate healthcare technology. This paper analyzes the use of technology and the challenges it presents to delivering healthcare services.
Definition and Analysis of the Problem
Inappropriate use and the lack of optimized healthcare technology impact delivering quality healthcare services. Firstly, the lack of appropriate healthcare technology increases the risk of medication errors. These errors emanate from illegible handwriting, poor documentation, inappropriate history taking, and lack of interdisciplinary collaboration (Bates & Singh, 2018). Illegible handwriting is associated with the wrong interpretation of prescriptions. As such, medication errors can emanate during dispensing or administration. Standard mistakes are related to mistaken patient identity, wrong medication, wrong dosage, wrong routes of administration, and wrong administration frequency (Bates & Singh, 2018). Similarly, poor documentation due to inappropriate technology increases the risk of medication errors. For example, improper documentation of a patient’s name or administered medication increases the likelihood of duplicate or wrong medication administration (Bates & Singh, 2018).
Need assistance with assignment? Get in touch with us at eminencepapers.com.
Lack of appropriate healthcare technology is associated with inappropriate history taking. Notably, healthcare providers are unable to capture pertinent information about referrals. This increases the risk of medication errors, such as the possibility of polypharmacy, hypersensitivity reactions, and drug toxicities (Härkänen et al., 2019). The lack of appropriate technology is associated with inadequate interdisciplinary collaboration. Interdisciplinary collaboration is associated with a better clinical decision-making process.
Secondly, the lack of appropriate technology has negative financial implications. Inappropriate technology increases the risk of billing errors in healthcare facilities. By so doing, reimbursements from insurers are reduced. Furthermore, billing errors of out-of-pocket payments have negative financial implications. Healthcare facilities will likely incur losses and accrue a low return on investment. Inappropriate use of healthcare technology increases the risk of penalization from the Centers for Medicare and Medicaid Services for eligible healthcare facilities for Interoperability Programs (CMS.gov, n.d.).
Further, the lack of appropriate technology lowers the quality of healthcare services. This is attributed to poor patient monitoring and a lack of timely access to healthcare services. Patient monitoring enables healthcare providers to evaluate the patient’s response to the treatment plan (Garber & Gustin, 2022). This forms the basis for modifying treatment plans to optimize healthcare services. The lack of appropriate technology hinders this process by necessitating physical interactions between patients and healthcare providers. This is disadvantageous for patients with chronic conditions and those whose mobility is inhibited by geographical distance. Such patients are unable to access timely healthcare services. Lack of close monitoring and convenient access to healthcare services lowers the quality of healthcare services and worsens the patient’s prognosis (Garber & Gustin, 2022).
Lastly, inappropriate healthcare technology impedes the provision of continuing medical education among healthcare providers. Continuous medical education and training equip healthcare providers with current and evidence-based knowledge and skills (Carroll, 2018). This increases their competency and improves the quality of their services. By so doing, individual and organizational productivity is improved.
Possible Solutions
Various strategies can be implemented to improve the use of technology in healthcare. The first strategy is the implementation of certified electronic health record systems. Electronic health record (EHR) systems increase the quality of healthcare services by optimizing routine operations (Lin et al., 2019). EHR systems eliminate errors related to illegible handwriting by embracing computerized provider order entries (CPOE) (Lin et al., 2019). CPOEs eliminate medical errors related to medication administration and dispensing. EHR systems also provide Clinical Decision Support Systems (CDSS). CDSS enables prescribers to select the best evidence-based interventions that fulfil patients’ unique needs (Lin et al., 2019). This is based on the patient’s medical history and case study reports.
Electronic health record systems improve interdisciplinary collaboration. They allow multidisciplinary team members such as nurses, physicians, pharmacists, and laboratory technologists to consult each other (Lin et al., 2019). This promotes an interdisciplinary clinical decision-making process. Interdisciplinary clinical decision-making is associated with selecting the best and current evidence-based practices (Lin et al., 2019). As such, the quality of healthcare services is improved.
An example is an interdisciplinary collaboration in managing a patient with type 2 diabetes mellitus. Essentially, physicians play a crucial role in prescribing using the CPOEs, while pharmacists evaluate the accuracy and completeness of the prescriptions and check for possible drug interactions or contraindications. Similarly, nurses play a crucial role in safe medication administration, and laboratory technologists avail timely laboratory and radiological findings. Accordingly, EHR systems enable these healthcare providers to conduct perpetual consultations and develop the best treatment and care plans.
The second strategy is the use of telehealth technology. Telehealth technology improves the quality of healthcare services and care coordination. Telehealth embraces various tools such as remote patient monitoring, mobile health, store and forward, and video conferencing (Carroll, 2018). Remote patient monitoring embraces wearable devices that enable healthcare providers to evaluate patients perpetually. Subsequently, wearable technologies would allow patients to collect and transmit their health data (Carroll, 2018). Then, healthcare providers assess the transmitted data. As a result, they can initiate timely interventions to promote the well-being of patients.
Technologies such as mobile health have features such as text messages and reminders. These features improve adherence to treatment plans by allowing patients to set alarms (Carroll, 2018). Additionally, healthcare providers conduct continuous patient follow-ups through audio calls and text messages. These interventions improve adherence to the treatment plan. Further, store and forward technology enables asynchronous patient data transmission and delivery (Rutledge et al., 2021). Also, storing and delivering technology allows the delivery of health information, such as laboratory and radiological results, among authorized healthcare providers. It also facilitates timely access to accurate information (Rutledge et al., 2021). As such, healthcare providers initiate prompt treatment plans for patients.
Videoconferencing allows real-time interaction between patients and healthcare providers. Real-time interaction is critical because healthcare providers evaluate patients’ responses to the treatment plan and initiate pertinent treatment modifications (Rutledge et al., 2021). Video conferencing also enables patients to seek clarification about specific medical techniques. For example, appropriate inhalation techniques using a nebulizer can be demonstrated to patients via video conferencing. This information can help avert acute asthmatic attacks and improve the patient’s quality of life.
Proposed Solution
My proposed solution is the adoption of certified electronic health record systems. As mentioned, electronic health record (EHR) systems increase the quality of healthcare services by optimizing routine operations. EHR systems eliminate errors related to illegible handwriting by embracing computerized provider order entries (CPOE) (Lin et al., 2019). CPOEs eliminate medical errors related to medication administration and dispensing. EHR systems also provide Clinical Decision Support Systems (CDSS). CDSS enables prescribers to select the best evidence-based interventions that fulfil patients’ unique needs (Lin et al., 2019). Besides, an EHR system enables an interdisciplinary clinical decision-making process by allowing healthcare providers to consult among themselves. Notably, interdisciplinary decision-making is associated with selecting the best and current evidence-based practices (Lin et al., 2019).
Implementation Plan
The stakeholders involved in the implementation are healthcare providers and healthcare facility administrators. The first step is obtaining stakeholder buy-in. This will be accomplished by explaining the merits of an EHR system and how it will transform the delivery of healthcare services. The second step is resource allocation and budgeting, and the third is software and hardware acquisition. The fourth step is software and hardware installation, and the sixth is staff training. Healthcare providers will be trained on the appropriate use of hardware and software. Vendors and installation engineers will facilitate training. Training equips staff with relevant skills in the use of EHR systems. The scope of training will also include regulatory requirements such as the Health Insurance Portability and Accountability Act of 1996 and the guidelines for meaningful use (Moore & Frye, 2019).
Justification of Electronic Health Record (EHR) Systems in Solving the Identified Problem
The identified problem is inappropriate use and the lack of optimized healthcare technology, resulting in the delivery of poor-quality healthcare services. Using a certified EHR system is an evidence-based approach that optimizes the quality of healthcare services. This is achieved via three main strategies. They include computerized provider order entries, Clinical Decision Support Systems, and automated billing (Lin et al., 2019). According to Lin et al. (2019), CPOEs eliminate medical errors related to medication administration and dispensing. In contrast, CDSS enables prescribers to select the best evidence-based interventions that meet patients’ needs.
References
Bates, D. W., & Singh, H. (2018). Two decades since to err is human: An assessment of progress and emerging priorities in patient safety. Health Affairs, 37(11), 1736–1743. https://doi.org/10.1377/hlthaff.2018.0738
Carroll, K. (2018). Transforming the Art of Nursing: Telehealth Technologies. Nursing Science Quarterly, 31(3), 230–232. https://doi.org/10.1177/0894318418774930
CMS.gov. (n.d.). Promoting Interoperability Programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms
Garber, K., & Gustin, T. (2022). Telehealth Education: Impact on Provider Experience and Adoption. Nurse Educator, 47(2), 75–80. https://doi.org/10.1097/NNE.0000000000001103
Härkänen, M., Vehviläinen-Julkunen, K., Murrells, T., Rafferty, A. M., & Franklin, B. D. (2019). Medication administration errors and mortality: Incidents reported in England and Wales between 2007 ̶ 2016. Research in Social and Administrative Pharmacy, 15(7), 858–863. https://doi.org/10.1016/j.sapharm.2018.11.010
Lin, Y. K., Lin, M., & Chen, H. (2019). Do electronic health records affect the quality of care? Evidence from the HITECH Act. Information Systems Research, 30(1), 306–318. https://doi.org/10.1287/isre.2018.0813
Moore, W., & Frye, S. (2019). Review of HIPAA, Part 1: History, protected health information, and privacy and security rules. Journal of Nuclear Medicine Technology, 47(4), 269–272. https://doi.org/10.2967/JNMT.119.227819
Rutledge, C. M., O’Rourke, J., Mason, A. M., Chike-Harris, K., Behnke, L., Melhado, L., Downes, L., & Gustin, T. (2021). Telehealth Competencies for Nursing Education and Practice: The Four P’s of Telehealth. Nurse Educator, 46(5), 300–305. https://doi.org/10.1097/NNE.0000000000000988
Schmutz, J. B., Meier, L. L., & Manser, T. (2019). How effective is teamwork? The relationship between teamwork and performance in healthcare teams: A systematic review and meta-analysis. BMJ Open, 9(9), 1–16. https://doi.org/10.1136/bmjopen-2018-028280
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Research Paper: The Research Paper should be approximately five to seven pages, double-spaced in MS Word and include a minimum of six references in APA format.
PowerPoint Presentation: The PowerPoint presentation should be approximately 10–15 slides with relevant speaker’s notes and include a minimum of three audio-visual components (e.g., images, figures, tables, audio and video links, etc.). Follow these guidelines to create your PowerPoint presentation.
Include a cover slide with the course number, course title, title of the PowerPoint presentation, your full name, and date.
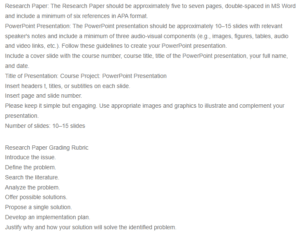
The Use of Technology in Healthcare
Title of Presentation: Course Project: PowerPoint Presentation
Insert headers t, titles, or subtitles on each slide.
Insert page and slide number.
Please keep it simple but engaging. Use appropriate images and graphics to illustrate and complement your presentation.
Number of slides: 10–15 slides
Research Paper Grading Rubric
Introduce the issue.
Define the problem.
Search the literature.
Analyze the problem.
Offer possible solutions.
Propose a single solution.
Develop an implementation plan.
Justify why and how your solution will solve the identified problem.

