The History of Behavioral Health
Behavioral health defines how routine cognitive habits affect individuals’ psychosocial and physical wellbeing within a society. Behavioral health is an expansive concept encompassing all measures utilizable in treating mental and physical issues and lifestyle remedies that are key to preserving health. Over time, there has been an evolution in the understanding of human behavioral health. The Middle age era, for instance, refuted claims that mental illnesses are attributable to religious curses and established that internal causes cause mental illnesses. The modern era has since embraced a more scientific approach to understanding behavioral health, utilizing scientific-based reasoning to define mental illnesses (BERTOLOTE, 2018). This paper discusses historical events that defined the understanding of behavioral health, emphasizing how these events impacted human health and changes to the behavioral health profession.
The History of Behavioral Health
The history of behavioral health reveals multiple events that enhanced human understanding of human behavior and contributed to establishing various institutions currently critical in preserving mental health. These events include deinstitutionalization, the establishment of the U.S. mental health policy, and the creation of the Diagnostic and Statistical Manual for Mental Disorders (DSM).
Deinstitutionalization is a historical event that commenced in the mid-1950s. The establishment of an institutional inpatient care model preceded this event. This model oversaw psychiatric patients bundled in various care institutions across America. Deinstitutionalization involved moving psychiatric patients from care institutions back to their families and then closing these care institutions (Novella, 2016). The deinstitutionalization process followed a policy provision that required only very ill patients to remain in care institutions. It also coincided with the development of the antipsychotic drug chlorpromazine, which maintains high efficacy against various mental disorders.
Deinstitutionalization remains a significant social experiment whose benefits may have been clouded by its ripple effects on active and newly diagnosed psych patients at that time. The policy provision on deinstitutionalization was targeted at improving the wellbeing of psychiatric patients. However, it created a psychiatric illness crisis by not defining a framework for these patients to continue their treatment and rehabilitative services. Closure of inpatient mental health institutions also denied care to persons who were newly diagnosed with mental disorders post-enactment of the deinstitutionalization policy. This further exacerbated the crisis by restricting access to psychiatric treatment for over 2 million people (Novella, 2016). This effect is still being felt to date since many psychiatric patients across numerous states do not have access to psych healthcare.
Another historical event is the establishment of the U.S. mental health policy. This policy was founded in the early 1900s as Mental Health America but was later enacted by President Harry Truman in 1946 as the National Mental Health Act. This policy provision is targeted at improving the wellbeing of mentally ill patients through research as well as lobbying efforts from governmental and non-governmental groups. This enactment saw the creation of the National Institute of Mental Health. Also, it directed its funding by the federal government to enable it to carry out research projects to improve psychiatric wellbeing.
The U.S. mental health policy has significantly impacted behavioral health science in the current predisposition. This act has enabled increased accurate diagnosis of mental disorders by ensuring the establishment of current evidence-based and scientifically sound diagnostic methods for mental illnesses. It has also increased access to psychiatric care by directing the creation of more care institutions across states that deal with mental disorders. It has also enhanced treatment approaches to mental conditions by promoting innovations and research projects aimed at coming up with novel therapeutic modalities utilizable in mental disorders and ensuring the reduction of the prevalence of mental disorders and consequential suicidal rates associated with these illnesses.
The creation of the Diagnostic and Statistical Manual for Mental Disorders (DSM) was also a landmark historical event that will forever shape approaches to psychiatric care. DSM is a diagnostic tool that aids in the accurate diagnosis of mental disorders by defining a specific set of symptoms that are characteristic of each mental illness. This diagnostic tool was created in 1917 by a joint committee of the National Commission on Mental Hygiene and the American Psychiatric Association. The committee defined various mental disorders and grouped them into 22 stratiforms. The findings were then compiled into the ‘Statistical Manual for the Use in the Institutions for the Insane. This manual underwent ten revisions between 1917 and 1942. A consensus on various mental disorders, their classification, and characterizing features was later arrived at, ushering in the birth of DSM-1 in 1952. DSM 1 has since undergone several reviews and updates up to the currently used edition of DSM called the DSM-5.
DSM has considerably impacted the modern approach to diagnosing and treating mental disorders. This manual has formed a powerful tool for accurately diagnosing these disorders. The effectiveness of psychiatric management is dependent on accurate and timely diagnosis of mental disorders and the subsequent initiation of evidence-based therapy. DSM has enabled fast and accurate diagnosis of these illnesses, improving patient care outcomes. It has also enabled the standardization of psychiatric diagnosis by outlining definite criteria for identifying various mental illnesses. DSM also guides research processes by providing a checklist for referencing mental disorders. It has also guided therapeutic approaches to psych patients’ care management, enabling optimal care outcomes.
Historical revolutions in behavioral health have been informed considerably by these historical events. These events have enhanced the understanding of human mental disorders and their presentations as well as remedy approaches. These events have also shaped the behavioral health profession by defining the roles of behavioral health professionals. Such roles can be elucidated from these events’ findings, as detailed below.
Historical events in behavioral health have informed the need to create and integrate mental health experts into the mainstream care provision system. Unlike the traditional disposition where mental illness patients were subjected to harsh treatment, the modern dispensation sees mentally ill patients as human beings who are incarcerated by their disease process. In addition, specialties in healthcare have evolved that are targeted at the ethical handling of these patients and working with them to realize optimal care outcomes (Buscemi & Hendrick, 2018). Further, mental illnesses are no longer a source of societal ridicule but are now considered illnesses like any other that require healthcare attention.
Moreover, these events have enhanced public awareness of mental illnesses. Despite still lagging, public awareness of mental illness has made great strides as far as the detection and consequent treatment of these diseases are concerned. Various strategies have been instituted by governments and other non-governmental groups that reach out to people who may be suffering from these illnesses and offer safe spaces in which their problems can be identified and solved.
Historical events have also informed the appropriateness of strategies utilizable in psychiatric management that ensure optimal outcomes. The revolution of psychiatric management followed the institutionalization of psychiatric patients and subsequent deinstitutionalization. Both systems realized specific gains but had considerable downfalls. However, the lessons obtained from their rollout have continuously defined psychiatric care. The realization that psychiatric patients required specialized care was the highlight of these two systems. Additionally, deinstitutionalization considered the significance of social cycles and social wellbeing in the overall management of these patients (Shen & Snowden, 2016). Currently, the management of psychiatric patients considers both their psychological, social, and physical well-being.
Understanding behavioral health remains critical in enhancing the care outcomes of psych patients. This understanding has been shaped considerably by historical events on behavioral health. Such events as the creation of DSM and the establishment of the Mental Health Act in the U.S. still impact care provision processes for psychiatric patients. These events have also enabled the redefinition of behavioral health professionals.
References
A Brief History of Mental Illness and the U.S. Mental Health Care System. Uniteforsight.org. (2022). Retrieved 4 February 2022, from https://www.uniteforsight.org/mental-health/module2.
BERTOLOTE, J. (2018). The roots of the concept of mental health. World Psychiatry, 7(2), 113-116. https://doi.org/10.1002/j.2051-5545.2008.tb00172.x
Buscemi, D., & Hendrick, S. (2018). Relation of behavioral health to quality health care. Baylor University Medical Center Proceedings, 31(2), 240-243. https://doi.org/10.1080/08998280.2018.1444248
Novella, E. (2016). Mental Health Care in the Aftermath of Deinstitutionalization: A Retrospective and Prospective View. Health Care Analysis, 18(3), 222-238. https://doi.org/10.1007/s10728-009-0138-8
Shen, G., & Snowden, L. (2016). Institutionalization of deinstitutionalization: a cross-national analysis of mental health system reform. International Journal Of Mental Health Systems, 8(1). https://doi.org/10.1186/1752-4458-8-47
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
The History of Behavioral Health
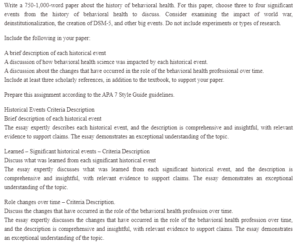
Write a 750-1,000-word paper about the history of behavioral health. For this paper, choose three to four significant events from the history of behavioral health to discuss. Consider examining the impact of world war, deinstitutionalization, the creation of DSM-5, and other big events. Do not include experiments or types of research.
Include the following in your paper:
A brief description of each historical event
A discussion of how behavioral health science was impacted by each historical event.
A discussion about the changes that have occurred in the role of the behavioral health professional over time.
Include at least three scholarly references, in addition to the textbook, to support your paper.
Prepare this assignment according to the APA 7 Style Guide guidelines.
Historical Events Criteria Description
Brief description of each historical event
The essay expertly describes each historical event, and the description is comprehensive and insightful, with relevant evidence to support claims. The essay demonstrates an exceptional understanding of the topic.
Learned – Significant historical events – Criteria Description
Discuss what was learned from each significant historical event
The essay expertly discusses what was learned from each significant historical event, and the description is comprehensive and insightful, with relevant evidence to support claims. The essay demonstrates an exceptional understanding of the topic.
Role changes over time – Criteria Description.
Discuss the changes that have occurred in the role of the behavioral health profession over time.
The essay expertly discusses the changes that have occurred in the role of the behavioral health profession over time, and the description is comprehensive and insightful, with relevant evidence to support claims. The essay demonstrates an exceptional understanding of the topic.

