Telehealth and Evidence-Based Practice
Telehealth is a form of digital technology where information and communication between patients and health practitioners and between the health practitioners themselves via digital communication tools. These tools include computers, mobile phones, online patient portals, mobile apps, and other appropriate information-gathering tools (Mauldon, 2007). These tools aid in information passage between these groups of people remotely and set a reminder for various crucial appointments. Most community-based patients have access to some of these tools, making communication easy and more reliable. They can plan for doctor’s appointments, treatment, and medication adherence. Our assignment writing help is at affordable prices to students of all academic levels and academic disciplines.
The Telehealth system is made up of three major players. The medical practitioners, including doctors and nurses, are the medium for communication and, finally, the patients. Medical practitioners use these mediums to communicate directly with patients without traveling to health facilities (Fischer, Ray, et al., 2020). The terms of treatment, management protocols, and safety methods are all passed via these media to the patients. The commonly used media are mobile phones, texts and calls, computers, and the patient online portal, where all patient information is kept via video conferencing. Other characteristics of telehealth include being more affordable, reliable, faster, and more accessible to use by both parties.
The use of telehealth in the health sector is increasingly gaining more followers. According to recent USA studies, about 70% of home-based patients prefer online digital communication tools to attend appointments and for information (Mauldon, 2007). Implementing such a move curbed the shortage of nurses as most patients are attended to online. Health facilities benefit from these implementations because emergency department visits and inpatient admissions are reduced. Nurses connect with patients without traveling, making physical appointments, and registering, increasing efficiency. Nurses also have an excellent opportunity to educate patients virtually on managing their diseases. Nurses form an appropriate and meaningful connection with their patients, improving care delivery. It also requires few nurses to manage these patients compared to the traditional approach, where a scarcity of nurses is experienced.
Figure 1: V-sensor and e-checkup app
Figure 2: PHware app
Telehealth is increasingly being integrated into the healthcare sector because of its efficiency. Through teleconference, virtual surveillance, digital consults, and wireless connections, telehealth links patients to critical healthcare services. Telehealth helps patients obtain the appropriate care at the right place by improving access to physicians and experts. Through telemonitoring of vital signs, there is a boost in reducing mortality and hospitalization of heart failure patients (Fischer, Ray, et al., 2020). This has improved the standard of living of these patients. There is the development of many online apps that monitor various activities within our body; an example is PHware V-, sensor, and e-check,p, which is available on smartphones. These online apps measure vital signs, including blood pressure and heart rate, calculate body calorie intake, and store personal patient information.
The current development in infrastructure and communication within rural areas has increased dramatically. Electrification of houses, good roads, and an improved economy have raised internet use and various communication tools such as mobile phones and computers because of internet availability. The internet availability allows mobile users to install the required apps and track vital body changes (Marcin, Shaikh & Steinhorn, 2016). Mobile health is used mainly because mobile phones are easily accessible to most people within rural areas. The acceptability of these tools by the patients has also played a major in their continuous usage. Patients prefer such because of their efficiency and cost reduction on transport and other hospital expenses.
There are many techniques I would love to implement. Community-based patients are primarily elderly and require specialized and immediate care in emergencies. These patients have heart problems, hypertension, diabetes, and other immunocompromised diseases and, therefore, need continuous care (Marcin, Shaikh & Steinhorn, 2016). The health sector may not have enough nurses to manage these patients due to the inadequate number of health practitioners. When continuously admitted within the facility, these patients are at high risk of developing a hospital-acquired infection. The use of telehealth will benefit these patients greatly and improve their standard of living.
I would recommend the use of mobile health services. These patients have access to mobile phones, and either the patient or the patient’s caretaker may request direct services from the nurses. Also, nurses can call and check on the patient’s condition. Another tool is the online mobile apps such as PHware, which measures the patients’ vital signs online. They will enable the patient to be cautious enough to prevent any further damage to themselves. These vital signs measurement is also crucial for medical approaches; the nearby health facility is notified in case of emergency. Implementing the use of the patient online portal, where patients’ information is kept, is essential in disease management in terms of drug usage. Telehealth is facing many difficulties in its implementation as of now. It is a new development within the health facility, and much research still concerns its application. The internet, the overall cost of remote services, and the lack of health insurance by most elderly patients limit its application. The benefits of telehealth are excellent, and it may dominate the health sector. Crowding of the hospital premises, the transmission of hospital-acquired infection, and the availability of enough nurses will be controlled when the system is applied appropriately. For example, during these times of coronavirus, telehealth was used on most occasions to prevent virus transmission. Mobile health, remote patient monitoring, online monitoring devices, E-visits, and telecare should be used increasingly with this current technology.
References
Mauldon, E. (2007). The Use of and Attitude Towards Telehealth in Rural Communities. Australian Journal of Primary Health, 13(3), 29-34.
Fischer, S. H., Ray, K. N., Mehrotra, A., Bloom, E. L., & Uscher-Pines, L. (2020). Prevalence and characteristics of Telehealth utilization in the United States. JAMA network open, 3(10), e2022302-e2022302.
Marcin, J. P., Shaikh, U., & Steinhorn, R. H. (2016). Addressing health disparities in rural communities using telehealth. Pediatric Research, 79(1), 169-176.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Purpose of Assignment
According to the American Association of Colleges of Nursing (2008), “Use telecommunication technologies to assist in effective.
Telehealth and Evidence-Based Practice
communication in a variety of healthcare settings…”
American Association of College of Nursing. (2008). The Essentials of Baccalaureate Education for Professional Nursing Practice. Retrieved from: https://www.aacnnursing.org/Education-Resources/AACN-Essentials
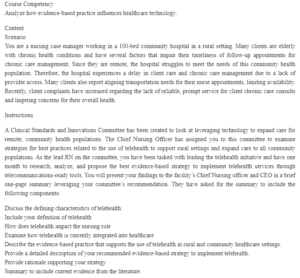
Course Competency
Analyze how evidence-based practice influences healthcare technology.
Content
Scenario
You are a nursing case manager working in a 100-bed community hospital in a rural setting. Many clients are elderly with chronic health conditions and have several factors that impair their timeliness of follow-up appointments for chronic care management. Since they are remote, the hospital struggles to meet the needs of this community health population. Therefore, the hospital experiences a delay in client care and chronic care management due to a lack of provider access. Many clients also report aligning transportation needs for their nurse appointments, limiting availability. Recently, client complaints have increased regarding the lack of reliable, prompt service for client chronic care consults and lingering concerns for their overall health.
Instructions
A Clinical Standards and Innovations Committee has been created to look at leveraging technology to expand care for remote, community health populations. The Chief Nursing Officer has assigned you to this committee to examine strategies for best practices related to the use of telehealth to support rural settings and expand care to all community populations. As the lead RN on the committee, you have been tasked with leading the telehealth initiative and have one month to research, analyze, and propose the best evidence-based strategy to implement telehealth services through telecommunications-ready tools. You will present your findings to the facility’s Chief Nursing officer and CEO in a brief one-page summary leveraging your committee’s recommendation. They have asked for the summary to include the following components:
Discuss the defining characteristics of telehealth.
Include your definition of telehealth
How does telehealth impact the nursing role
Examine how telehealth is currently integrated into healthcare
Describe the evidence-based practice that supports the use of telehealth in rural and community healthcare settings.
Provide a detailed description of your recommended evidence-based strategy to implement telehealth.
Provide rationale supporting your strategy
Summary to include current evidence from the literature.




