SOAP Note – Sleep-Wake Disorder
ID: B.D. Age: 68. Gender: Male. Race: Caucasian DOB: 1/1/1977
S: Subjective
- Chief Complaint: “I am really tired…my sleep disappears in the middle of the night. I can no longer maintain having a good sleep.”
- History of Present Illness: The case is of a 68-year-old Caucasian male. He is experiencing difficulty maintaining sleep at night. The sleep problem began three months ago and has been increasing in intensity. The sleep problems are characterized by multiple episodes of waking up at night. They also manifest on most days of the week. The problem has persisted despite the patient trying hard to sleep well. The patient also experiences fatigue and increasing episodes of daytime sleepiness. This has impacted his overall operationalizations during the day.
- Past Medical History:
- Type 2 Diabetes Mellitus: Diagnosed three years ago. The patient is currently on antidiabetic medications.
- Hypertension: Diagnosed mid-last year. He was started on medications.
- Medications:
- Metformin 1 g every 12 hours
- Enalapril 5 mg once daily
- Allergies: No known drug or food allergies.
- Social History: The patient is a social smoker. He takes at least two cigarettes during social events. He also drinks during social events and over the weekends. The patient prefers beer over other alcoholic beverages. He has never taken any controlled substances. The patient is married. He lives with his wife and two grandchildren. He is a retired Marine. He currently runs a wellness workshop for veterans.
- Family History: Family history is negative of any sleep-wake disorder. His father died of coronary heart disease. His mother is, however, alive and has no known chronic illness.
- Sleep History: The patient denies having difficulty falling asleep. He also reports going to bed early. He, however, notes that he mostly watches television before going to bed and is frequently on his phone just before sleeping. He used to take caffeine at night but has since stopped. He occasionally takes a bottle of alcohol in the evenings. He denies sleep apnea, restless leg syndrome, or nocturnal leg cramps. The patient also denied waking up with shortness of breath.
Review of Systems:
- Constitutional:
- ☐ Fever ☐ Weight loss ☐ Fatigue þ Weakness ☐ Other: ___No abnormalities__
- Head, Eyes, Ears, Nose, Throat (HEENT):
- þHeadache ☐ Vision changes ☐ Hearing loss ☐ Nasal congestion ☐ Sore throat ☐ Other: _________ No abnormalities __
- Cardiovascular:
- ☐ Chest pain ☐ Palpitations ☐ Shortness of breath ☐ Edema ☐ Other: ______No abnormalities __
- Respiratory:
- ☐ Cough ☐ Wheezing ☐ Hemoptysis ☐ Shortness of breath ☐ Other: _________ No abnormalities __
- Gastrointestinal:
- ☐ Nausea ☐ Vomiting ☐ Diarrhea ☐ Constipation ☐ Abdominal pain ☐ Other: _________ No abnormalities __
- Genitourinary:
- ☐ Dysuria þ Frequency ☐ Hematuria ☐ Urgency ☐ Incontinence ☐ Other: _________ No abnormalities __
- Musculoskeletal:
- ☐ Joint pain ☐ Muscle pain ☐ Stiffness ☐ Swelling ☐ Other: ____No abnormalities __
- Neurological:
- þ Headaches ☐ Dizziness ☐ Numbness ☐ Tremors ☐ Seizures ☐ Other: _________ No abnormalities __
- Skin:
- ☐ Rash ☐ Itching ☐ Dryness ☐ Lesions ☐ Other: ______No abnormalities __
- Endocrine:
- ☐ Weight changes ☐ Heat intolerance ☐ Cold intolerance þ Excessive thirst ☐ Other: _________ No abnormalities __
- Hematologic/Lymphatic:
- ☐ Easy bruising ☐ Bleeding ☐ Swollen glands ☐ Other: ___No abnormalities __
O: Objective
- Vital Signs:
- Blood Pressure: 140/89 mmHg
- Heart Rate: 79 beats per minute
- Respiratory Rate: 17 breaths per minute
- Temperature: 99.7 F
- Physical Examination: The patient is alert. He responds appropriately to the questions asked. He appears fatigued. No signs of scars or lesions on the head. His heart rate is elevated but rhythmic. No signs of difficulty breathing, wheezing, or labored breath.
Mental Status Exam:
- Appearance:
-
- þWell-groomed ☐ Disheveled ☐ Poor hygiene ☐ Other: _____No abnormalities __
- Behavior:
-
- þCalm ☐ Agitated þCooperative ☐ Uncooperative ☐ Other: ___No abnormalities__
- Speech:
-
- þ Normal rate ☐ Pressured ☐ Slow ☐ Incoherent ☐ Other: _________ No abnormalities __
- Mood:
-
- þ Euthymic ☐ Depressed ☐ Anxious ☐ Euphoric ☐ Other: _________ No abnormalities __
- Affect:
-
- þAppropriate ☐ Flat ☐ Labile ☐ Inappropriate ☐ Congruent with stated mood ☐ Other: _________ No abnormalities __
- Thought Process:
-
- þ Logical ☐ Disorganized ☐ Tangential ☐ Circumstantial ☐ Other: ___No abnormalities __
- Thought Content:
-
- þNo delusions ☐ Delusions ☐ Obsessions ☐ Preoccupations ☐ Other: _________ No abnormalities __
- Perceptions:
-
- þ No hallucinations ☐ Hallucinations ☐ Illusions ☐ Other: No abnormalities __
- Cognition:
- Orientation:
-
- þ Oriented to person þ Oriented to place þ Oriented to time þ Oriented to situation ☐ Other: _________ No abnormalities __
-
- Attention:
-
- þAble to focus ☐ Easily distracted ☐ Difficulty concentrating ☐ Other: _________ No abnormalities __
-
- Memory:
- þ Intact ☐ Recent memory impaired ☐ Remote memory impaired ☐ Immediate memory impaired
- Abstract Thinking:
- Memory:
-
- þAble to interpret proverbs ☐ Difficulty with abstract thinking ☐ Concrete thinking ☐ Other: _ No abnormalities __________
- Insight:
- þ Good ☐ Fair ☐ Poor ☐ No insight ☐ Other: _____No abnormalities_______
- Judgment:
- þ Good ☐ Fair ☐ Poor ☐ Impaired ☐ Other: _____No abnormalities_________
A: Assessment
- Summary of Findings: The subjective and objective findings in the case indicated significant difficulty in maintaining sleep for more than three months. Sleep problems occur on most nights. The patient also had a history of smoking and alcohol use. He is a known diabetic and hypertensive.
- Diagnosis: The presumptive diagnosis is insomnia disorder 780.52 (G47. 00). The difficulty maintaining sleep, lasting for more than three months and appearing on most nights of the week, is aligned with the DSM-V criteria for chronic insomnia (DSM-V). This affirms the diagnosis.
Differential Diagnoses:
- Substance-Induced Sleep Disorder F10.182: The difficulty maintaining sleep, warranted the inclusion of this differential (DSM-V). The sleep troubles occurred on multiple nights and impacted his daytime functioning. Furthermore, the patient had a history of consuming alcohol (Selsick et al., 2024).
- Central Sleep Apnea G47.31 (327.21): The frequent night awakenings warranted the inclusion of this differential. He also experienced daytime sleepiness and morning headaches. These manifestations are common in central sleep apnea. However, the negative history of apnea made this differential diagnosis less probable (Duffy et al., 2021).
- Sleeplessness and Circadian Rhythm Disorder F51.00 (G47.2): Patients with sleeplessness due to circadian rhythm disorder will commonly manifest with insomnia. This warranted the inclusion of this differential. The absence of evidence of sleep routine disruption in the patient makes this diagnosis less probable (Duffy et al., 2021).
Plan
- Treatment Plan:
- Non-pharmacological treatment: The patient will be educated on effective sleep hygiene. He will also be started on stimulus control therapy:
- Pharmacological treatment: The patient will be started on sleep medications. Eszopiclone is the medication of choice for the patient.
- Patient education: The patient will be educated on the disease process and the perceived risks of chronic insomnia. He will be told that chronic insomnia may predispose him to other health concerns, such as obesity, and should, therefore, be managed. He will also be advised to take his medications as prescribed for optimal effect.
- Laboratory testing: Thyroid function tests and CBC may only be necessary if the symptoms fail to improve with therapy. These tests may provide insight into underlying illnesses that may be causing insomnia.
- Referral: Referral to a neurologist may be necessary if the symptoms fail to improve with escalation of treatment.
- Medications: Eszopiclone 2 mg at bedtime.
- Follow-Up: The patient is scheduled to return for follow-up after two weeks.
Rationale
- Justification for Treatment Plan: Ensuring effective sleep hygiene is the first line in managing chronic insomnia. Here, the patient will be educated on lifestyle modifications that will help him improve his sleep. Foremost, he will be advised to maintain regular sleep schedules. He will also be told to limit daytime napping and taking caffeine and alcoholic beverages a night. These measures may help him improve his sleep.
- Stimulus control therapy may also help the patient improve his sleep. It involves advising the patient to restrict behaviors that may disrupt sleep. Such behaviors include using mobile phones and other digital devices before going to bed (Edinger et al., 2021).
- Pharmacotherapy was necessitated in this case. This is because non-pharmacological measures alone are insufficient in maintaining sleep (Del Rio Verduzco et al., 2023). Eszopiclone is a sleep pill that is effective in reducing nighttime awakenings. This makes it a suitable option for use.
References
Del Rio Verduzco, A., Salari, A., & Haghparast, P. (2023). Efficacy and safety of pharmacotherapy in chronic insomnia: A review of clinical guidelines and case reports. Mental Health Clinician, 13(5), 244–254. https://doi.org/10.9740/mhc.2023.10.244
DSM-V. (n.d.). DSM. Psychiatry.org – DSM. https://www.psychiatry.org/psychiatrists/practice/dsm
Duffy, J. F., Abbott, S. M., Burgess, H. J., Crowley, S. J., Emens, J. S., Epstein, L. J., Gamble, K. L., Hasler, B. P., Kristo, D. A., Malkani, R. G., Rahman, S. A., Thomas, S. J., Wyatt, J. K., Zee, P. C., & Klerman, E. B. (2021). Workshop report. Circadian rhythm sleep–wake disorders: Gaps and opportunities. Sleep, 44(5). https://doi.org/10.1093/sleep/zsaa281
Edinger, J. D., Arnedt, J. T., Bertisch, S. M., Carney, C. E., Harrington, J. J., Lichstein, K. L., Sateia, M. J., Troxel, W. M., Zhou, E. S., Kazmi, U., Heald, J. L., & Martin, J. L. (2021). Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of Sleep Medicine Clinical Practice guideline. Journal of Clinical Sleep Medicine, 17(2), 255–262. https://doi.org/10.5664/jcsm.8986
Selsick, H., Heidbreder, A., Ellis, J., Ferini-Strambi, L., García-Borreguero, D., Leontiou, C., Mak, M. S. B., O’Regan, D., & Parrino, L. (2024). Assessment and management of chronic insomnia disorder: An algorithm for primary care physicians. BMC Primary Care, 25(1). https://doi.org/10.1186/s12875-024-02381-w
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
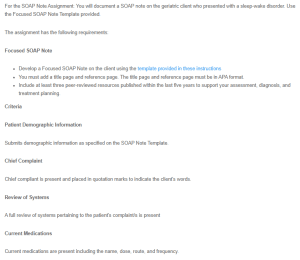
For the SOAP Note Assignment: You will document a SOAP note on the geriatric client who presented with a sleep-wake disorder. Use the Focused SOAP Note Template provided.
SOAP Note – Sleep-Wake Disorder
The assignment has the following requirements:
Focused SOAP Note
- Develop a Focused SOAP Note on the client using the template provided in these instructions
- You must add a title page and reference page. The title page and reference page must be in APA format.
- Include at least three peer-reviewed resources published within the last five years to support your assessment, diagnosis, and treatment planning.
Criteria
Patient Demographic Information
Submits demographic information as specified on the SOAP Note Template.
Chief Complaint
Chief compliant is present and placed in quotation marks to indicate the client’s words.
Review of Systems
A full review of systems pertaining to the patient’s complaint/s is present
Current Medications
Current medications are present including the name, dose, route, and frequency.
Subjective Information
All subjective information is documented appropriately and thoroughly
Objective Information
A focused exam related to the client’s chief complaint is presented. A full mental status exam is documented.
Assessment
This includes DSM-V-TR diagnosis/diagnoses, and ICD-10 code/s. Assessment data/diagnosis must correspond to the chief complaint and subjective information given by the patient
Plan
Must include full treatment plan (pharmacological, non-pharmacological treatments, patient education, referrals, laboratory testing, and follow-up). A rationale is required to support your treatment plan based on the diagnosis.
APA Format and References
A title page and reference page in APA format must be included. The APA 7th edition should be used. References should be published within the last five years.
