Soap Note Elias Leon Case
Subjective Data:
Current Medications:
Elias is currently taking Omeprazole, an over-the-counter medication, for gas reflux. He follows the instructions provided on the packaging. Additionally, he uses Ibuprofen 200 mg for joint pain in his knees, taking 2 to 4 tablets a couple of times a day as needed. He reported that he took his last dose of medication before coming to the clinic.
Review of Systems:
Constitutional: Denies daytime tiredness and fatigue.
Eyes: Denies visual loss, blurry vision, or discharge.
Ears/Nose/Mouth/Throat: Denies hearing loss, nasal congestion, sore throat, or mouth ulcers.
Cardiovascular: Denies chest pain, palpitations, or edema.
Pulmonary: Denies shortness of breath, coughing, or wheezing.
Gastrointestinal: Denies abdominal pain, nausea, vomiting, diarrhea, or constipation.
Genitourinary: Denies urinary frequency, urgency, or dysuria.
Musculoskeletal: Reports joint pain and achy knees.
Integumentary & Breast: No rashes, lesions, or breast changes reported.
Neurological: Denies headaches, dizziness, numbness, or tingling.
Psychiatric: Denies anxiety or depression.
Endocrine: Denies heat or cold intolerance, polyphagia, polyuria, or polydipsia.
Hematologic/Lymphatic: Denies bleeding, easy bruising or lymphadenopathy.
Allergic/Immunologic: Denies itchiness, sneezing, or rash.
Objective Data
Vital Signs:
• Weight: 195 lbs
• BMI: 28.8 (Overweight)
• Height: 69 inches
• Temperature: 98.6°F (oral)
• Blood Pressure: 172/94 mmHg (right arm)
• Respiration Rate: 14 breaths per minute, regular rhythm, unlabored effort
• Oxygen Saturation: 98% on room air
Physical Exam
General Appearance:
• Obese Hispanic male, alert, and in no respiratory distress.
Eyes:
• Fundoscopic examination notable for AV nicking; otherwise unremarkable.
Ears/Nose/Mouth/Throat:
• No abnormalities noted.
Cardiovascular:
• Normoactive precordium.
• No murmurs, gallops, or rubs.
• No peripheral edema.
Pulmonary:
• Clear to auscultation bilaterally.
• No wheezes, rales, or rhonchi.
• Respirations regular and unlabored.
Gastrointestinal:
• Abdomen soft, non-tender, and non-distended.
• Bowel sounds present in all quadrants.
Genitourinary:
• No abnormalities noted.
Musculoskeletal:
• No joint swelling or deformities.
• No knee joint tenderness or decreased range of motion on examination.
Integumentary:
• Skin warm and dry.
• No rashes or lesions observed.
Neurological:
• Alert and oriented to person, place, and time.
• Cranial nerves II-XII intact.
• Motor and sensory functions intact.
Psychiatric:
• Appropriate mood and affect.
Endocrine:
• No goiter or thyroid nodules palpable.
Hematologic/Lymphatic:
• No lymphadenopathy noted.
Management Plan:
1. Diagnostic Tests:
a. Complete Blood Count (CBC): To rule out anemia or other hematologic issues that could complicate hypertension management (Mann, 2020).
b. Basic Metabolic Panel (BMP): To evaluate kidney function (BUN, creatinine) and electrolytes, which can be affected by hypertension and its treatments (Xiong et al., 2021).
c. Lipid Profile: To assess cardiovascular risk factors (cholesterol levels) associated with hypertension (Xiong et al., 2021).
d. Electrocardiogram (ECG): To check for signs of left ventricular hypertrophy or other cardiac abnormalities associated with long-term hypertension (Mann, 2020).
e. Urinalysis: To screen for proteinuria or microalbuminuria, which can indicate hypertension-related kidney damage (Xiong et al., 2021).
2. Medications:
a. Nifedipine Extended-Release 20 mg orally once daily: Nifedipine is a calcium channel blocker that helps lower blood pressure by relaxing the blood vessels, making it easier for the heart to pump. It is effective in treating hypertension, particularly in patients with coexisting conditions like diabetes and those of African American or Hispanic descent (Xiong et al., 2021).
b. Ibuprofen (OTC) 200 mg: Continue with the medication. However, he should take 1-2 tablets every 6 hours for knee pain. Encourage limiting use due to potential adverse effects on blood pressure and kidney function (Mann, 2020).
c. Omeprazole (OTC) 20 mg orally once daily: Continue current regimen for gas reflux. Instruct to take 30 minutes before meals (Chapelle et al., 2021).
3. Suggested Consults/Referrals:
a. Dietitian/Nutritionist: For dietary counseling, focus on a heart-healthy diet (e.g., DASH diet) to help manage blood pressure and weight (Xiong et al., 2021).
b. Smoking Cessation Program: Referral to a smoking cessation program to provide support and resources for quitting smoking, which is essential for reducing cardiovascular risk (Hartmann-Boyce et al., 2021).
c. Cardiologist: Consider referral for further cardiovascular evaluation and management if indicated by diagnostic test results or if blood pressure remains uncontrolled (Xiong et al., 2021).
4. Patient Education:
a. Hypertension Management: Explain the importance of controlling blood pressure to prevent complications such as heart disease, stroke, and kidney damage. Discuss medication adherence and potential side effects of Nifedipine (Xiong et al., 2021).
b. Lifestyle Modifications: Encourage regular physical activity (e.g., 30 minutes of moderate exercise most days of the week), weight loss, a low-sodium diet, and limiting alcohol intake (Mann, 2020).
c. Smoking Cessation: Emphasize the benefits of quitting smoking, provide resources, and discuss available pharmacotherapy and behavioral interventions (Hartmann-Boyce et al., 2021).
d. Monitoring Blood Pressure: Teach Elias to monitor his blood pressure at home and keep a log to bring to follow-up appointments (Xiong et al., 2021).
5. Follow-up:
a. Initial Follow-up: Schedule a follow-up appointment in 4 weeks to assess blood pressure response to Nifedipine, review home blood pressure logs, and evaluate for any side effects or complications (Xiong et al., 2021).
b. Ongoing Monitoring: Subsequent follow-ups every 3-6 months, depending on blood pressure control and overall health status. Adjust medication as necessary based on blood pressure readings and lab results (Xiong et al., 2021).
c. Prompt Return Visits: Advise Elias to return sooner if he experiences symptoms such as severe headache, chest pain, shortness of breath, significant leg swelling, or any other concerning symptoms.
References
Mann, J. (2020). Choice of drug therapy in primary (essential) hypertension. Published online.
Hartmann-Boyce, J., Livingstone-Banks, J., Ordóñez-Mena, J. M., Fanshawe, T. R., Lindson, N., Freeman, S. C., … & Aveyard, P. (2021). Behavioural interventions for smoking cessation: an overview and network meta‐analysis. Cochrane Database of Systematic Reviews, (1). https://doi.org/10.1002/14651858.CD013229.pub2
Chapelle, N., Ben Ghezala, I., Barkun, A., & Bardou, M. (2021). The pharmacotherapeutic management of gastroesophageal reflux disease (GERD). Expert Opinion on Pharmacotherapy, 22(2), 219-227. https://doi.org/10.1080/14656566.2020.1817385
Xiong, P., Liu, Z., Xiong, M., & Xie, F. (2021). Prevalence of high blood pressure under 2017 ACC/AHA guidelines: a systematic review and meta-analysis. Journal of Human Hypertension, 35(3), 193-206. https://doi.org/10.1038/s41371-020-00454-8
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Soap Note Elias Leon Case
Elias Leon Case
The patient is a 57 years old overweight Hispanic male construction worker and smoker who presents for evaluation of an elevated blood pressure 170/92 noted at a recent local health fair. He takes Ibuprofen for joint pain. He denies daytime somnolence and fatigue, interrupted sleep, snoring and apnea, chest pain, edema, or shortness of breath. Physical examination is notable for a BP 172/94 on right arm, Overweight BMI, Fundoscopic findings of AV nicking and otherwise negative cardiopulmonary examination.
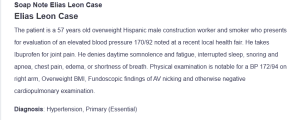
Soap Note Elias Leon Case
Diagnosis: Hypertension, Primary (Essential)
Vitals
– Weight: 195 lb
– BMI 28.8
– Height 69’’
– Age 57 years old Male
– Temp 98.6F (oral)
– BP 172/94 right arm
– Respiration 14bpm, rhythm: regular, effort: unlabored
– O2 98% on room air
Chief Complaints: “I was recently at a health fair in my community where I had my blood pressure checked. The nurse told me that I should see a doctor because My pressure is too high. I think she said 170/92 or something like that. Do those numbers sound right? Anyhow, my wife was concerned and made the appointment”
Allergies; NKDA
Medications:
– Take Omeprazole OTC for gas reflux, follow instruction on box.
– Ibuprofen 200mg: 2-4 of them couple times a day for achy knees.
– Last take medications before coming to Clinic.
Family History: Father died at age 62 from a stroke. Mom’s age 78 have diabetes, grandmother passed away at age 82 from Diabetes. Father’s Father died age 52 from heart attack. Brother’s age 48 have Hypertension, Uncle’s age 79 have Hypertension. Have a healthy age 19 year old son.
Please Enter your Assessment/ Management plan or SOAP note below
Rubric:
Subjective Data : Document Current Medications, Review of System: 5 criteria:
1.) Complete.
2.) Accurate.
3.) Written in Professional Language.
4.) Pertinent to the Chief Complaint.
5.) Includes Subjective findings only
Objective Data Document Physical Exam Findings: 5 criteria:
1.) Complete;
2.) Accurate;
3.) Written in Professional Language;
4.) Pertinent to the Chief Complaint;
5.) Includes Objective findings only
Management Plan: Use the expert diagnosis provided to create a pertinent, comprehensive, evidenced-based management plan. Address the following criteria in the plan:
1.) Diagnostic tests;
2.) Medications (write out a complete order, even for OTC meds);
3.) Suggested consults/referrals;
4.) Patient education;
5.) Follow-up, including time interval and specific symptoms to prompt a return visit sooner;
6.) Provide rationales for each intervention and include references to support your plan. Clinical practice guidelines should be utilized as applicable.
References and Format: Current APA citations for references in management plan. Use of clinical practice guidelines when applicable.

