SOAP Note – Depression
Patient Demographic Information
Name: Jane Sheraton | Age: 48 | Race: Not specified | Marital Status: Not specified | Employment Status: Recently lost her job | Date of Visit: [Insert Date]
Subjective:
Chief Complaint: “I’ve been feeling really sad and can’t stop crying.”
HPI:
Jane Sheraton is 48 years old and describes her chief complaint as sadness with crying, which started a few weeks ago. This was concurrent with losing her job, which she described as emotionally devastating. Jane describes feelings of guilt, hopelessness, and worthlessness, but most of all, she is concerned about being unable to keep her son at university. She has become reclusive and withdrawn from activities she used to enjoy, such as running and socializing with friends. Her sleep pattern is interrupted: She wakes frequently at night; this can be due to thoughts of failure ruminating in her mind. Jane admitted to hoarding paracetamol but denied any immediate intention of harming herself. She described repeated suicidal ideation. She denies a history of previous psychiatric treatment and diagnosis of depression.
Past Psychiatric History
- No prior diagnoses or treatments were reported.
- There is no history of inpatient or outpatient treatment.
- Suicidal ideation is present, but no history of attempts is mentioned.
Substance Abuse: There is no reported history of tobacco, alcohol, or illicit drug use.
Review of Systems:
- Appetite: Reduced; patient reports only eating small amounts, such as toast.
- Sleep: Disrupted sleep with frequent awakenings due to distressing thoughts.
- No significant surgeries or chronic conditions were noted.
Current Medication List:
- None reported
- No known drug allergies
Objective Information:
Vital Signs:
Height: Not provided.
Weight: Not provided.
Pulse: Not provided.
Respiratory Rate: Not provided.
Blood Pressure: Not provided.
Temperature: Not provided.
Physical Examination
Jane presents as tearful with poor eye contact and psychomotor retardation, exhibiting slowed speech and movement. She demonstrated reduced engagement and energy during the consultation.
MSE:
- Appearance: Jane appeared sad and tearful, with poor eye contact.
- Behavior: Psychomotor retardation, slow movements, reduced engagement.
- Speech: Slow, monotonous, reflecting low mood.
- Mood: Depressed
- Affect: Blunted
- Thought Process: Linear but centered on hopelessness and shame sentiments.
- Thought Content: Suicidal thoughts are present; patient reports stockpiling paracetamol but no definite plan to act.
- Attention & Concentration: Poor concentration, likely due to ruminating thoughts.
- Memory: Intact for both short- and enduring memory.
- Orientation: In tune with time, place, and people.
- Insight: Partial insight; recognizes feelings of depression but does not fully attribute it to mental health.
- Judgment: Impaired judgment related to self-worthlessness and suicidal ideation.
Assessment
Diagnoses:
- Major Depressive Disorder, Recurrent, Severe, with Suicidal Ideation (ICD-10 Code: F33.2)
Rationale: Jane displays a number of DSM-5 signs of significant depression, such as low mood, loss of interest or enjoyment, significant distress, social withdrawal, suicidal ideation, guilt, and worthlessness, as indicated by Cai et al. (2021). She denies substance use, and she has never been diagnosed with any mental illness.
- Adjustment Disorder with Depressed Mood (ICD-10 Code: F43.21)
Rationale: The beginning of depressive symptoms presented by Jane was initially brought on by some significant life event, such as a job loss. She has shown poor adjustment to this stressor and evidences symptoms of depressed mood and impairment in social functioning (O’Donnell et al., 2020).
Differential Diagnoses:
- Generalized Anxiety Disorder (ICD-10 Code: F41.1)
Rationale: Jane shows excessive worry about her son’s education and financial security, which could be suggestive of co-occurring generalized anxiety (Munir & Takov, 2022). However, anxiety is not the chief complaint, and she does not meet the full DSM-5 criteria for GAD.
- Panic Disorder (ICD-10 Code: F41.0)
Rationale: While at this point Jane does not overtly mention experiencing panic attacks, the feelings of doom and anxiety around her situation may indicate a panic disorder (Cackovic et al., 2020). In such a way, she might require further screening to confirm it.
Treatment Plan:
- Pharmacologic Treatment
- Fluoxetine (Prozac) 20 mg/day: This SSRI is the standard of care for first-line treatment of Jane’s major depressive disorder with suicidal ideation. Fluoxetine is indicated in severe depression and will be titrated to response.
- Alprazolam (Xanax) 0.25 mg PRN: Prescribed for immediate relief of anxiety symptoms related to her depression (George & Tripp, 2019). Given the risk of dependence, Jane should use Alprazolam sparingly, and a small initial prescription will be provided.
- Non-Pharmacologic Treatment
-
- Cognitive Behavioral Therapy (CBT): CBT would help in restructuring negative thinking and overcoming overwhelming feelings of guilt, hopelessness, and worthlessness. CBT has been effective in treating depression and preventing suicide attempts, as indicated by Bentum et al. (2021).
- Psychiatry Referral and Crisis Services: Urgent referral to psychiatric care for close monitoring, given Jane’s suicidal ideation and stockpiling of paracetamol. A crisis intervention plan may be considered necessary to ensure her safety.
-
Patient/Family Education:
Medication adherence to early warning signs of worsening depression significantly increased suicidal ideation will be taught to Jane and her family. They will be informed when to seek urgent care or mental health services.
Follow-Up:
The patient will return in a week to evaluate her drug response and the worsening of her symptoms. Special consideration will be given to potential fluoxetine adverse effects, such as the potential for an increase in suicidal thoughts during the first phase of SSRI medication.
References
Bentum, J. S., Bronswijk, S. C., Sijbrandij, M., Lemmens, L. H. J. M., Peeters, F. F. P. M. L., Drukker, M., & Huibers, M. J. H. (2021). Cognitive therapy and interpersonal psychotherapy reduce suicidal ideation independent from their effect on depression. Depression and Anxiety, 38(9), 940–949. https://doi.org/10.1002/da.23151
Cackovic, C., Nazir, S., & Marwaha, R. (2020). Panic disorder. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/28613692/
Cai, H., Xie, X.-M., Zhang, Q., Cui, X., Lin, J.-X., Sim, K., Ungvari, G. S., Zhang, L., & Xiang, Y.-T. (2021). Prevalence of suicidality in major depressive disorder: A systematic review and meta-analysis of comparative studies. Frontiers in Psychiatry, 12(2). https://doi.org/10.3389/fpsyt.2021.690130
George, T., & Tripp, J. (2019, October 11). Alprazolam. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538165/
Munir, S., & Takov, V. (2022, October 17). Generalized anxiety disorder. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/28722900/
O’Donnell, M. L., Agathos, J. A., Metcalf, O., Gibson, K., & Lau, W. (2020). Adjustment disorder: Current developments and future directions. International Journal of Environmental Research and Public Health, 16(14), 2537. https://doi.org/10.3390/ijerph16142537
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
After watching the video, please complete a Case Analysis Evaluation using the provided SOAP Note Template. Video Link: https://youtu.be/5fK3IDR-Rp8
SOAP Note – Depression
In the treatment section list the medication(s) you would prescribe at this visit. Make sure you provide a rationale for your decision.
Student Case Analysis Example .
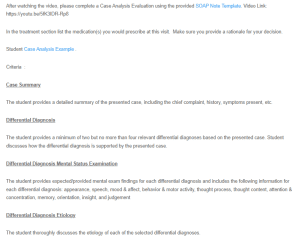
Criteria :
Case Summary
The student provides a detailed summary of the presented case, including the chief complaint, history, symptoms present, etc.
Differential Diagnosis
The student provides a minimum of two but no more than four relevant differential diagnoses based on the presented case. Student discusses how the differential diagnosis is supported by the presented case.
Differential Diagnosis Mental Status Examination
The student provides expected/provided mental exam findings for each differential diagnosis and includes the following information for each differential diagnosis: appearance, speech, mood & affect, behavior & motor activity, thought process, thought content, attention & concentration, memory, orientation, insight, and judgement
Differential Diagnosis Etiology
The student thoroughly discusses the etiology of each of the selected differential diagnoses.
Differential Diagnosis Diagnostic Screening Tools
The student identifies and discusses the screening tools that would be utilized to support each of the differential diagnoses.
Case Analysis
The student thoroughly discusses the likely diagnosis and how that diagnosis is supported by the presented case/patient.
Treatment Plan
The student provides a thorough treatment plan that includes all of the following elements: pharmacologic treatment, non-pharmacologic treatment, patient/family education, referrals, follow-up, and other information as applicable.
Grammar/APA
