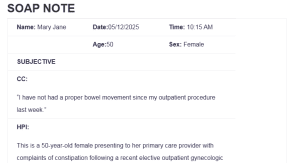
SOAP NOTE
| Name: Mary Jane | Date:05/12/2025 | Time: 10:15 AM |
| Age:50 | Sex: Female | |
| SUBJECTIVE | ||
| CC:
“I have not had a proper bowel movement since my outpatient procedure last week.” |
||
| HPI:
This is a 50-year-old female presenting to her primary care provider with complaints of constipation following a recent elective outpatient gynecologic procedure. She reports that she has not had a bowel movement for six days. Associated symptoms include abdominal bloating, mild cramping, and a sense of incomplete evacuation: SOAP NOTE. She denies nausea, vomiting, fever, or rectal bleeding. She notes minimal fiber and water intake since the procedure and attributes her symptoms to postoperative use of hydrocodone-acetaminophen for pain management. She denies any past history of chronic constipation. |
||
| Medications:
Hydrocodone-Acetaminophen 5-325 mg, 1 tablet every 6 hours PRN for postoperative pain Daily multivitamins for general health |
||
| PMH
No chronic illnesses or major medical diagnoses previously documented. Allergies: No known drug allergies (NKDA) Medication Intolerances: None reported Chronic Illnesses/Major traumas No history of chronic diseases or prior significant trauma Hospitalizations/Surgeries Recent elective outpatient gynecological procedure Denies history of diabetes, hypertension, ulcers, asthma, lung disease, heart disease, cancer, TB, thyroid problems, kidney disease, or psychiatric diagnosis. |
||
| Family History
Mother has hypertension, and father has type 2 diabetes. No known family history of gastrointestinal disorders, psychiatric conditions, or cancer. |
||
| Social History
The patient is a high school graduate and works part-time as a retail cashier. She is divorced and lives alone. She reports occasional tobacco use (~2-3 cigarettes per day) but denies alcohol consumption and illicit drug use. She feels safe at home and has no current psychosocial concerns. |
||
| ROS | |
| General
Reports fatigue and abdominal bloating. Denies weight change, fever, or night sweats. |
Cardiovascular
Denies chest pain, palpitations, or peripheral edema. |
| Skin
No rashes, discoloration, or delayed wound healing. |
Respiratory
Denies cough, shortness of breath, or wheezing. |
| Eyes
No blurring or vision changes. |
Gastrointestinal
Positive for constipation and bloating. Denies nausea, vomiting, or black stools. |
| Ears
No ear pain, discharge, or hearing loss. |
Genitourinary/Gynecological
Normal postoperative course. Denies dysuria or urinary changes. |
| Nose/Mouth/Throat
Denies sinus issues, sore throat, or dental concerns. |
Musculoskeletal
No joint pain, stiffness, or back pain. |
| Breast
Denies lumps or nipple discharge. |
Neurological
No weakness, dizziness, or paresthesia. |
| Heme/Lymph/Endo
Denies bruising, night sweats, or endocrine symptoms. |
Psychiatric
Denies depression, anxiety, or sleep disturbance. |
| OBJECTIVE | |
| Weight 174 lbs BMI 29.8 | Temp 98.4°F | BP 124/82 mmHg |
| Height 5’5″ | Pulse 78 bpm | Resp 16 breaths/min |
| General Appearance
Healthy-appearing woman in no acute distress. Alert, oriented, and cooperative. Slightly somber initially but brighter during the visit. |
||
| Skin
Warm, dry, intact. No rashes or lesions. |
||
| HEENT
Normocephalic, atraumatic. Eyes PERRLA, EOMs intact. TMs clear. Nasal mucosa pink, oral mucosa moist with healthy dentition. |
||
| Cardiovascular
Regular rate and rhythm, no murmurs or gallops. Pulses 3+ bilaterally, no edema. |
||
| Respiratory
Clear to auscultation bilaterally. Normal chest expansion. |
||
| Gastrointestinal
Abdomen is soft, mildly distended, non-tender, with hypoactive bowel sounds. No hepatosplenomegaly. |
||
| Breast
No masses or abnormalities on palpation. |
||
| Genitourinary
Normal post-gynecological exam findings. No CVA tenderness or discharge. |
||
| Musculoskeletal
Full range of motion in all extremities. |
||
| Neurological
Speech clear. Balance and gait normal. No focal deficits. |
||
| Psychiatric
Calm, cooperative, and maintains eye contact. No signs of acute distress. |
||
| Lab Tests
None were performed at this visit. No labs indicated at this stage. |
| Special Tests
None required during this encounter.
|
| Diagnosis |
| Differential Diagnoses
o 1-Functional Constipation (ICD-10: K59.00) – Functional constipation is considered a differential diagnosis, especially in individuals with dietary and lifestyle factors that impair regular bowel movements (Kilgore & Khlevner, 2024). In this patient’s case, her recent history of low fiber intake, reduced water consumption, and limited physical activity following surgery all contribute to transient functional bowel slowing. Although she has no prior history of chronic constipation, these acute behavioral changes mimic the conditions under which functional constipation can manifest. o 2-Postprocedural Ileus (ICD-10: K91.89) – Postprocedural ileus refers to a temporary impairment of bowel motility following surgical intervention. This is more common after intra-abdominal surgeries, but it can occur with any procedure involving anesthesia (Buchanan & Tuma, 2023). Symptoms include absent bowel movements, abdominal distention, and often nausea or vomiting. While this diagnosis is considered due to the patient’s recent procedure, it is less likely in this case. The presence of hypoactive bowel sounds (rather than absent), a soft non-tender abdomen, and no associated nausea or vomiting reduce the likelihood of ileus. o 3- Functional Diarrhea (ICD-10: K59.1) – Functional diarrhea is ruled out as a potential diagnosis. The patient has no complaints of loose stools, increased stool frequency, urgency, or nocturnal bowel movements. Her condition reflects hypoactivity of the bowels rather than the hypermotility seen in diarrhea. Therefore, this diagnosis is inconsistent with her symptoms and has been excluded (Savarino et al., 2022). Diagnosis o Drug-induced constipation (ICD-10: K59.09) is the primary diagnosis. This condition is a well-documented side effect of opioid medications, particularly those prescribed postoperatively. Opioids exert their constipating effects by binding to μ-opioid receptors in the gastrointestinal tract, which leads to delayed colonic transit, reduced peristalsis, and harder stool consistency (Sizar et al., 2021). In this case, the patient began experiencing significant constipation shortly after initiating hydrocodone-acetaminophen therapy for postoperative pain, making the temporal relationship between medication use and symptom onset clinically significant. Her report of not having a bowel movement for six days, along with abdominal bloating and discomfort, aligns with the presentation of drug-induced constipation. |
| Plan/Therapeutics |
| o Plan:
§ Further testing At present, no further diagnostic testing is necessary due to the absence of alarming symptoms. However, if there is no bowel movement within 5 to 7 days or symptoms worsen, imaging studies or laboratory work will be considered for further evaluation. § Medication The patient was prescribed Senna 17.2 mg to be taken orally twice daily for three days. She was advised to stop hydrocodone if pain permits and use acetaminophen instead. Over-the-counter docusate sodium was discussed as an optional stool softener. § Education Education was provided on opioid-induced constipation, emphasizing how opioids impact gut motility. The patient was instructed on the proper use of laxatives and stool softeners, and the importance of fiber, fluid intake, and movement. She understood and agreed with all components of the care plan. § Non-medication treatments She was advised to increase daily fiber intake (fruits, vegetables, whole grains), drink at least eight glasses of water, walk daily for physical activity, and try natural remedies like prune juice to promote regular bowel movements without relying solely on medications. |
| Evaluation of patient encounter
The patient was calm, attentive, and engaged during the consultation. She maintained good eye contact, asked appropriate questions, and clearly understood her diagnosis and treatment plan. She committed to following the plan and agreed to return if symptoms persisted or worsened. |
References
Buchanan, L., & Tuma, F. (2023). Postoperative Ileus. StatPearls. https://pubmed.ncbi.nlm.nih.gov/32809615/
Kilgore, A., & Khlevner, J. (2024). Review article: Functional constipation: Pathophysiology, evaluation and management. Alimentary Pharmacology & Therapeutics, 60(S1). https://doi.org/10.1111/apt.17852
Savarino, E., Zingone, F., Barberio, B., Marasco, G., Akyuz, F., Akpinar, H., Barboi, O., Bodini, G., Bor, S., Chiarioni, G., Cristian, G., Corsetti, M., Di Sabatino, A., Dimitriu, A. M., Drug, V., Dumitrascu, D. L., Ford, A. C., Hauser, G., Nakov, R., & Patel, N. (2022). Functional bowel disorders with diarrhoea: Clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility. United European Gastroenterology Journal, 10(6), 556–584. https://doi.org/10.1002/ueg2.12259
Sizar, O., Genova, R., & Gupta, M. (2021). Opioid Induced Constipation. PubMed; StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/29630236/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question 
| Name: | Date: | Time: |
| Age: | Sex: | |
| SUBJECTIVE | ||
| CC:
Reason given by the patient for seeking medical care “in quotes” |
||
| HPI:
Describe the course of the patient’s illness, including when it began, character of symptoms, location where the symptoms began, aggravating or alleviating factors; pertinent positives and negatives, other related diseases, past illnesses, surgeries or past diagnostic testing related to present illness. |
||
| Medications: (list with reason for med ) | ||
| PMH
Allergies:
Medication Intolerances:
Chronic Illnesses/Major traumas
Hospitalizations/Surgeries
“Have you every been told that you have: Diabetes, HTN, peptic ulcer disease, asthma, lung disease, heart disease, cancer, TB, thyroid problems or kidney disease or psychiatric diagnosis.” |
||
| Family History
Does your mother, father or siblings have any medical or psychiatric illnesses? Anyone diagnosed with: lung disease, heart disease, htn, cancer, TB, DM, or kidney disease. |
||
| Social History
Education level, occupational history, current living situation/partner/marital status, substance use/abuse, |
||
| ETOH, tobacco, marijuana. Safety status | |
| ROS | |
| General
Weight change, fatigue, fever, chills, night sweats, energy level |
Cardiovascular
Chest pain, palpitations, PND, orthopnea, edema |
| Skin
Delayed healing, rashes, bruising, bleeding or skin discolorations, any changes in lesions or moles |
Respiratory
Cough, wheezing, hemoptysis, dyspnea, pneumonia hx, TB |
| Eyes
Corrective lenses, blurring, visual changes of any kind |
Gastrointestinal
Abdominal pain, N/V/D, constipation, hepatitis, hemorrhoids, eating disorders, ulcers, black tarry stools |
| Ears
Ear pain, hearing loss, ringing in ears, discharge |
Genitourinary/Gynecological
Urgency, frequency burning, change in color of urine.
Contraception, sexual activity, STDS
Fe: last pap, breast, mammo, menstrual complaints, vaginal discharge, pregnancy hx
Male: prostate, PSA, urinary complaints |
| Nose/Mouth/Throat
Sinus problems, dysphagia, nose bleeds or discharge, dental disease, hoarseness, throat pain |
Musculoskeletal
Back pain, joint swelling, stiffness or pain, fracture hx, osteoporosis |
| Breast
SBE, lumps, bumps or changes |
Neurological
Syncope, seizures, transient paralysis, weakness, paresthesias, black out spells |
| Heme/Lymph/Endo
HIV status, bruising, blood transfusion hx, night sweats, swollen glands, increase thirst, increase hunger, cold or heat intolerance |
Psychiatric
Depression, anxiety, sleeping difficulties, suicidal ideation/attempts, previous dx |
| OBJECTIVE | |
| Weight BMI | Temp | BP |
| Height | Pulse | Resp |
| General Appearance
Healthy appearing adult female in no acute distress. Alert and oriented; answers questions appropriately. Slightly somber affect at first, then brighter later. |
||
| Skin
Skin is brown, warm, dry, clean and intact. No rashes or lesions noted. |
||
| HEENT
Head is normocephalic, atraumatic and without lesions; hair evenly distributed. Eyes: PERRLA. EOMs intact. No conjunctival or scleral injection. Ears: Canals patent. Bilateral TMs pearly grey with positive light reflex; landmarks easily visualized. Nose: Nasal mucosa pink; normal turbinates. No septal deviation. Neck: Supple. Full ROM; no cervical lymphadenopathy; no occipital nodes. No thyromegaly or nodules. Oral mucosa pink and moist. Pharynx is nonerythematous and without exudate. Teeth are in good repair. |
||
| Cardiovascular
S1, S2 with regular rate and rhythm. No extra sounds, clicks, rubs or murmurs. Capillary refill 2 seconds. Pulses 3+ throughout. No edema. |
||
| Respiratory
Symmetric chest wall. Respirations regular and easy; lungs clear to auscultation bilaterally. |
||
| Gastrointestinal
Abdomen obese; BS active in all 4 quadrants. Abdomen soft, non-tender. No hepatosplenomegaly. |
||
| Breast
Breast is free from masses or tenderness, no discharge, no dimpling, wrinkling or discoloration of the skin. |
||
| Genitourinary
Bladder is non-distended; no CVA tenderness. External genitalia reveals coarse pubic hair in normal distribution; skin color is consistent with general pigmentation. No vulvar lesions noted. Well estrogenized. A small speculum was inserted; vaginal walls are pink and well rugated; no lesions noted. Cervix is pink and nulliparous. Scant clear to cloudy drainage present. On bimanual exam, cervix is firm. No CMT. Uterus is antevert and positioned behind a slightly distended bladder; no fullness, masses, or tenderness. No adnexal masses or tenderness. Ovaries are non-palpable. (Male: both testes palpable, no masses or lesions, no hernia, no uretheral discharge. ) (Rectal as appropriate: no evidence of hemorrhoids, fissures, bleeding or masses—Males: prostrate is smooth, non-tender and free from nodules, is of normal size, sphincter tone is firm). |
||
| Musculoskeletal
Full ROM seen in all 4 extremities as patient moved about the exam room. |
||
| Neurological
Speech clear. Good tone. Posture erect. Balance stable; gait normal. |
||
| Psychiatric
Alert and oriented. Dressed in clean slacks, shirt and coat. Maintains eye contact. Speech is soft, though clear and of normal rate and cadence; answers questions appropriately. |
||
| Lab Tests
Urinalysis – pending Urine culture – pending Wet prep – pending |
| Special Tests |
| Diagnosis |
| Differential Diagnoses
o 1- o 2- o 3- Diagnosis o |
| Plan/Therapeutics |
| o Plan:
§ Further testing § Medication § Education § Non-medication treatments |
| Evaluation of patient encounter |
SOAP NOTE
Client’s Notes:
- 50 year old female with a diagnosis of “drug induced constipation” presents to primary care provider after a recent elective outpatient procedure with another provider. Patient is treated with options that can be done at home
- Please use the same format from previous soap note assignments
