Do you need any help for completing your assignment ? Contact us at eminencepapers.com. We endeavor to provide you with excellent service. Shared Decision-Making Policy:
In this presentation, we shall discuss the highlighted topics. These topics revolve around the introduction of the SHARE policy, which promotes shared decision making.
Shared decision-making is a central aspect of patient centered care. It is achieved through the collaboration of patients and health practitioners while making health related decisions. It promotes the patient’s ability to choose after accessing the necessary information. Through shared decision making, patients get an opportunity to be actively involved in their care. They have a chance to air their opinions and concerns and access critical information about their health. Following shared decision-making, physicians and patients are equally satisfied, while patients understand the physicians’ actions. This leads to creation of lasting relationships (British Medical Association, 2020).
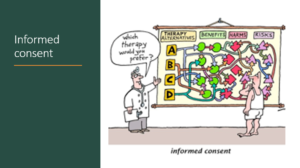
The main ethical principles that guide delivery of care include autonomy. Non-maleficience, beneficence, and justice. Autonomy refers to the health practitioner’s ability to respect the patient’s right to make choices regarding their health. This principle is closely connected to the patient’s right to informed consent. This right requires the patient to have access to all the necessary information regarding their health, which facilitates autonomy. Decisions that are made should benefit the patient and the wider community. Healthcare practitioners are legally obliged to observe these ethical principles during practice (Sedig, 2016).
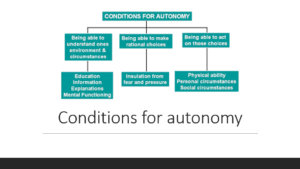
Autonomy of patients in healthcare settings is dependent on various factors. The patient must have the capacity to understand their circumstances, environment, and make rational choices. Acting on the choices is also important. To understand the environment and circumstances, education, explanations, and information are all critical. The ability to make choices should be free from pressure and fear. Additionally, acting on choices depends on their physical ability, personal, as well as social circumstances. These aspects can either promote or suppress the patients’ autonomy (Olejarczyk & Young, 2021).
Informed consent relates to access to information about potential harm to the body and the awareness about autonomy. The healthcare practitioners’ responsibility is to illuminate the patient on alternative therapies, treatments, and interventions, benefits of each , harms, as well as risks. Provision of this information enables the patient to actively participate in the process of decision making (Olejarczyk & Young, 2021).
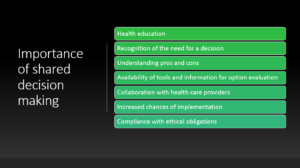
Shared decision-making promotes health education as patients learn about their conditions, causes, and possible treatments. The patients also recognize the need for a decision and understand the harms and benefits associated with each mode of treatment. Patients can easily access the required information through collaboration with health care providers. Once a decision is made collectively, the chances of implementation increase, and doctors are able to comply with the ethical obligations (British Medical Association, 2020).
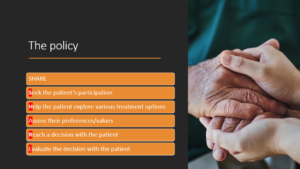
The SHARE policy is recommended as a way of promoting shared decision making. It involves the doctor/physician’s initiative to involve the patient’s active participation. Through collaboration, the discussion regarding various alternatives takes place. The assessment of values and preferences and a decision is reached. The same decision is evaluated to ensure that objectives will be met and both parties are satisfied (Agency for Healthcare Research and Quality, 2020).
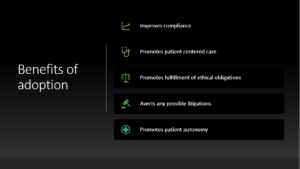
Adopting the SHARE policy is beneficial for the facility, patients, and healthcare practitioners. It promotes compliance of the facility and healthcare practitioners thus averting any possible litigations that may arise. It also enables the facility to offer patient centered care and acknowledgement of patient’s autonomy. The legal obligation to fulfill the ethical principles is fulfilled sufficiently (Sedig, 2016).
The SHARE policy is necessitated by various aspects that affect the health of patients and performance of the facility. Recent patient complains that highlight dissatisfaction with care and a total lack of understanding about their health issues have increased. Due to lack of involvement, patients barely adhere to the medication leading to negative outcomes and re-admissions. To change the current situation, it is necessary to implement shared decision-making as part of medical practice.
Collaborative decision-making is highly recommended for compliance with ethical principles, improved patient care, positive health outcomes, patient satisfaction, and physicians as well. Patients have the right to access information and actively participate in the decision-making process. Legal issues that could arise due to non-compliance are avoided. The SHARE policy is ideal in addressing each of these issues.
Agency for Healthcare Research and Quality. (2020). The SHARE Approach—Essential Steps of Shared Decisionmaking: Quick Reference Guide. Retrieved from AHRQ: https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tools/resource-1.html
British Medical Association. (2020). Autonomy or self-determination as a medical student. Retrieved from https://www.bma.org.uk/advice-and-support/ethics/medical-students/ethics-toolkit-for-medical-students/autonomy-or-self-determination
Olejarczyk, J. P., & Young, M. (2021). Patient Rights And Ethics. StatPearls[Internet].
Sedig, L. (2016). What’s the Role of Autonomy in Patient- and Family-Centered Care When Patients and Family Members Don’t Agree? AMA Journal of Ethics.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Shared Decision-Making Policy
Part II:
Create a presentation that briefly outlines the policy. Include your decision-making process for presenting the information contained in the policy.
Explain the specific policy compliance issues that occurred and why your proposed update will help improve the compliance issues.
Use two to three scholarly resources to support your decision-making process, some of the sources may be the same as sources used to support your recommendations in the policy memo.
You will turn in both your policy memo and presentation.
Your presentation will require an outline of your presentation speech or speaker notes depending on the format chosen for the presentation. For PowerPoint, 8-12 slides are required with speaker notes of 50-75 words for each slide. Reference information must be provided at the end of the presentation. Reference and title slides do not count as part of the slide count.
While APA style is not required for the body of this assignment, solid academic writing is expected, and documentation of sources should be presented using APA formatting guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.