Regulation for Nursing Practice Staff Development Meeting
Is your assignment devastating you ? Get in touch with us at eminencepapers.com. Our homework help will save you tons of time and energy required for your assignment papers.
Hello, and welcome to this kickoff presentation. In this presentation, we will discuss the regulation of nursing practice, emphasizing the difference between a board of nursing and a professional association of nurses. We will also discuss the regulation of Advanced Practice Registered Nurses.
Nursing practice in the U.S. is a regulated field. The Nursing Practice Act (NPA) sets forth the standards and rules to ensure the overall safety of the public. In the pursuit of quality healthcare, these regulations are central to establishing quality improvement frameworks and guaranteeing safe and effective care to all American citizens (Cassiani et al., 2020). NPA is interpreted into regulations by territorial nursing boards across the U.S. In most territories, nursing boards regulate all levels of nursing practice. As nursing practice gains prominence in the U.S. and globally, there has been a need to foster high standards of nursing practice. This has been earmarked by the establishment of various nursing associations. These associations serve to advocate for pertinent issues in nursing and improve the wellness of nurses.
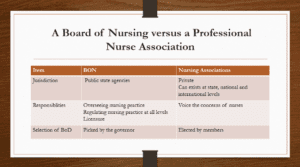
Nursing boards and nursing associations are integral to the practice of nursing. They, however, differ on several fronts. A Board of Nursing (BON) is a state agency that oversees nursing practice in various jurisdictions. Boards of Nursing (BONs) serve to protect and promote public health by ensuring that nurses are competent enough and that nursing practice is per the stated standards. Further, BONs provide licensures for each level of nursing practice. They are also responsible for implementing laws and policies prescribed by the state. BONs are governed by an elected Board of Directors. Nursing associations, on the other hand, are private professional membership organizations. They often require their members to pay subscription fees. They play a role in voicing nursing concerns. Nursing associations are non-jurisdictional and can exist at the state level, nationwide, and even internationally. Nursing associations are led by a Board of Directors (BoD) elected by members.
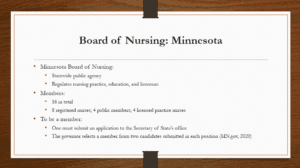
The Minnesota Board of Nursing is a statewide public agency that protects the health of Minnesota’s residents by regulating nursing practice, nursing education, and licensure. The board is constituted of nurses and non-nurse members. Per the Minnesota statutes, eight registered nurses, four licensed practice nurses, and four public members constitute the Minnesota Board of Nursing. These members serve for four years and must be residents of the state. Board members are appointed by the governor of the state. Appointments are made from applications received at the secretary of state’s office. To be a board member, one must meet the criteria of being a resident of Minnesota. The secretary of state’s office and governor’s staff often conduct background searches on all applicants and forward two names for each position. The governor then selects a name from the two (MN.gov, 2020).
BON in Minnesota defines nursing practice in the state and provides legal parameters to the scope of nursing practice. Nurses in the state are expected to be accountable for the quality of care they provide, recognize the limits of their knowledge and expertise, and maintain competency in their nursing roles. Per Minnesota’s statutes, The practice of practical nursing (LPNs), the practice of professional nursing (RNs), and the practice of advanced nurse practitioners are clearly defined. Their roles differ in scope and practice authority. As a full practice authority (FPA) state, Minnesota gives APRNs the authority to dispense and prescribe several medications. Notwithstanding, the board provides a strong quality statement and requires all nurses licensed to practice in the state to provide quality nursing care and abide by its statutes (MN.gov, 2020).
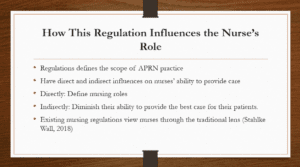
Nursing regulations on the APRN’s practice define the scope of practice of APRNs. They directly and indirectly influence their ability to provide care. Directly, APRN regulations define what is expected of them and their roles in healthcare. In Minnesota, nursing roles are defined by the Nurse Practice Act (NPA) under the Minnesota statute section 148. While these regulations are targeted at protecting the public, they may sometimes impede nursing advancements and indirectly affect their ability to provide the best care for their patients. Stahlke Wall (2018) notes that the existing nursing regulations view nurses through the traditional lens and don’t recognize innovations in nursing practice that nurses may apply to better the health of their patients. Stringent licensing and the expectations of nurses to abide by nurses’ roles defined by the regulators often prevent stymies ambitious nurses’ efforts to attempt innovative nursing knowledge in their practice.
The Minnesota statute clearly defines what is expected of nurses as far as quality healthcare is concerned. Per these statutes, nurses are expected to maintain accountability in providing quality nursing care, provide safe and effective care, and maintain competency in providing nursing care. This will improve the delivery of health care, as nurses are obligated to provide the best care to the patients. The provision of safe, effective, and quality healthcare will also have a bearing on the cost and access to healthcare. Providing safe, effective, and quality healthcare often guarantees better clinical outcomes (Connor et al., 2023). This is translated into reduced hospital stay days, lowered hospital readmission rates and clinical visitations, and reduced need for healthcare interventions. This will lower the cost of healthcare in the state. Restrictive regulation usually decreases access to healthcare. This is, however, not the case in Minnesota. Its FPA status has considerably expanded access to healthcare in the state.
Under Minnesota’s regulations, nurses are expected to promote a safe therapeutic environment for their patients and maintain accountability in providing safe, effective, and quality nursing care. This will have an impact when they are managing cross-cultural patients. Mihdawi et al. (2020) note that cultural competence nursing is based on the ability of nurses to provide a safe therapeutic environment for their patients, maintain cultural awareness, and build trust and good rapport with their patients. By abiding by the provisions of fostering a safe environment for their patients, nurses in Minnesota are expected to understand their environment, demonstrate cultural awareness, and provide care indiscriminately to all patients. This will be translated into effective care for cross-cultural patients.
Minnesota is a full practice authority state. APRNs in the state prescribe and dispense various medications independently. The scope of APRNs in Minnesota includes but is not limited to prescribing, diagnosing, performing advanced assessments, dispensing and administering therapeutic devices, drugs, and controlled substances. As advanced practitioners, APRNs are healthcare leaders who are also expected to be researchers, health educators, and primary care providers. Additionally, they can accept referrals, interpret diagnostic results, and supervise other nursing activities. The Minnesota statutes define the clinical roles of APRNs and persons who may practice as APRNS. Per these statutes, an individual licensed as an APRN and certified to practice as either a Certified Nurse Practitioner (CNP), Certified Registered Nurse Anesthetist (CRNA), Clinical Nurse Specialist (CNS), or Certified Nurse Midwife (CNM) is allowed to practice in the state as an APRN.
The nursing regulatory landscape in Minnesota has seen significant changes, with each change targeted at improving the quality of nursing care. Currently, there is a bipartisan bill to keep nurses from leaving the provision. This legislative proposal is geared toward addressing nursing shortages in the state. In the wake of the COVID-19 pandemic, several regulatory changes were made to improve access to nursing care. The board of nursing was authorized to temporarily extend or renew expired permits to address nurse shortages. Additionally, practice restrictions were waivered for APRNs to further ensure that more patients receive nursing care (Leslie et al., 2023). Far from that, there has also been an amendment to include mandatory continuous education for all nurses. These legislative changes have played a role in elevating the quality of nursing care in the state.
Cassiani, S. H., Lecorps, K., Rojas Cañaveral, L. K., da Silva, F. A., & Fitzgerald, J. (2020). Regulation of Nursing Practice in the Region of the Americas. Revista Panamericana de Salud Pública, 44, 1. https://doi.org/10.26633/rpsp.2020.93
Connor, L., Dean, J., McNett, M., Tydings, D. M., Shrout, A., Gorsuch, P. F., Hole, A., Moore, L., Brown, R., Melnyk, B. M., & Gallagher‐Ford, L. (2023). Evidence‐based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews on Evidence-Based Nursing, 20(1), 6–15. https://doi.org/10.1111/wvn.12621
Leslie, K., Myles, S., Stahlke, S., Schiller, C. J., Shelley, J. J., Cook, K., Stephens, J., & Nelson, S. (2023). Regulating during crisis: A qualitative comparative case study of nursing regulatory responses to the COVID-19 pandemic. Journal of Nursing Regulation, 14(1), 30–41. https://doi.org/10.1016/s2155-8256(23)00066-2
Mihdawi, M., Al-Amer, R., Darwish, R., Randall, S., & Afaneh, T. (2020). The influence of nursing work environment on patient safety. Workplace Health & Safety, 68(8), 384–390. https://doi.org/10.1177/2165079920901533
MN.gov. (2020). Minnesota Board of Nursing – Minnesota’s State Portal. https://mn.gov/boards/assets/Newsltr_Summer_2019_tcm21-392338.pdf
Stahlke Wall, S. (2018). The impact of regulatory perspectives and practices on professional innovation in nursing. Nursing Inquiry, 25(1). https://doi.org/10.1111/nin.12212
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Nursing is a very highly regulated profession. There are over 100 boards of nursing and national nursing associations throughout the United States and its territories. Their existence helps regulate, inform, and promote the nursing profession. With such numbers, it can be difficult to distinguish between BONs and nursing associations and overwhelming to consider the various benefits and options offered by each.
Regulation for Nursing Practice Staff Development Meeting
Both boards of nursing and national nursing associations have significant impacts on the nurse practitioner profession and scope of practice. Understanding these differences helps lend credence to your expertise as a professional. In this Assignment, you will practice the application of such expertise by communicating a comparison of boards of nursing and professional nurse associations. You will also share an analysis of your state board of nursing.
To Prepare:
- Assume that you are leading a staff development meeting on regulation for nursing practice at your healthcare organization or agency.
- Review the NCSBN and ANA websites to prepare for your presentation.
The Assignment: (8- to 9-slide PowerPoint presentation)
Develop an 8- to 9-slide PowerPoint Presentation that addresses the following:
- Describe the differences between a board of nursing and a professional nurse association.
- Describe the board for your specific region/area.
- Who is on the board?
- How does one become a member of the board?
- Describe at least one state regulation related to the general nurse’s scope of practice.
- How does this regulation influence the nurse’s role?
- How does this regulation influence delivery, cost, and access to healthcare?
- If a patient is from another culture, how would this regulation impact the nurse’s care/education?
- Describe at least one state regulation related to Advanced Practice Registered Nurses (APRNs).
- How does this regulation influence the nurse’s role?
- How does this regulation influence delivery, cost, and access to healthcare?
- Has there been any change to the regulation within the past 5 years? Explain.
- Include Speaker Notes on Each Slide (except on the title page and reference page)