Psychiatric Patient Evaluation
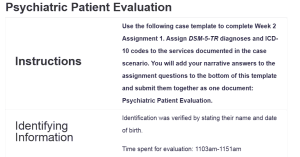
Instructions |
Use the following case template to complete Week 2 Assignment 1. Assign DSM-5-TR diagnoses and ICD-10 codes to the services documented in the case scenario. You will add your narrative answers to the assignment questions to the bottom of this template and submit them together as one document: Psychiatric Patient Evaluation. | |||||||||||||||||||||||||||||||||||||||||
Identifying Information |
Identification was verified by stating their name and date of birth.
Time spent for evaluation: 1103am-1151am |
|||||||||||||||||||||||||||||||||||||||||
Chief Complaint |
“My primary doctor thinks I need more help than she can give me now.” | |||||||||||||||||||||||||||||||||||||||||
HPI |
42 young female was evaluated for psychiatric evaluation and referred by her primary care provider for worsening depression and panic symptoms. She is currently prescribed escitalopram 5mg po daily for depression, alprazolam 1mg po daily for anxiety.
Today, the client reported symptoms of worsening in past month for depression with anergia, anhedonia, motivation, reports anxiety, frequent worry, reports feeling restlessness, palpitations “feels like everything is closing in on me, can’t focus, hard time breathing,” no reported obsessive/compulsive behaviors. Client reported feelings like want to sleep and never wake up.. There is no evidence of psychosis or delusional thinking. Client denied past episodes of hypomania, hyperactivity, erratic/excessive spending, involvement in dangerous activities, self-inflated ego, grandiosity, or promiscuity. Client reports increased irritability and easily frustrated. Has low frustration tolerance, sleeping 10-12 hrs/24hrs, appetite decreased. She has somatic concerns with GI upset and headaches. Client denied any current binging/purging behaviors, denied withholding food from self or engaging in anorexic behaviors. No self-mutilation behaviors. |
|||||||||||||||||||||||||||||||||||||||||
Diagnostic Screening Results |
Screen of symptoms in the past week: Severity Measure for Panic Disorder = Total Score 38 |
|||||||||||||||||||||||||||||||||||||||||
Past Psychiatric and Substance Use Treatment |
· Entered mental health system when she was age 29 after a family suicide.
· Previous Psychiatric Hospitalizations: · Previous Detox/Residential treatments: · Previous psychotropic medication trials: sertraline (became suicidal), trazodone (worsened nightmares), bupropion (became suicidal) · Previous mental health diagnosis per client/medical record: |
|||||||||||||||||||||||||||||||||||||||||
Substance Use History |
Have you used/abused any of the following (include frequency/amt/last use):
Any history of substance related: · Blackouts: – · Tremors: – · DUI: – · D/T’s: – · Seizures: – Longest sobriety |
|||||||||||||||||||||||||||||||||||||||||
Psychosocial History |
Client was raised by single mother. She is married; has 2 children.
Employed at local day care as administrative assistant. Education: High School Diploma Denied current legal issues. |
|||||||||||||||||||||||||||||||||||||||||
Suicide / Homicide Risk Assessment |
Suicide Inquiry: Denies active suicidal ideations, intentions, or plans. | |||||||||||||||||||||||||||||||||||||||||
Mental Status Examination |
She is a 42-year-old Hispanic female who looks her stated age. She is cooperative with examiner. She is disheveled, dressed appropriately. There is psychomotor restlessness. Her mood is anxious and mildly irritable. She denies any auditory or visual hallucinations. There is no evidence of any delusional thinking. She denies any current suicidal or homicidal ideation. |
|||||||||||||||||||||||||||||||||||||||||
Clinical Impression |
The client is a 42 yo Hispanic female who presents with a history of treatment for depression and panic symptoms.
Moods are anxious and irritable. She has reported symptoms related to her depression and panic. no evident mania/hypomania, no psychosis, denied current cravings for drugs/alcohol, exhibits no withdrawal symptoms, has somatic concerns of GI upset and headaches. At the time of disposition, the client adamantly denies SI/HI ideations, plans, or intent and has the ability to determine right from wrong and can anticipate the potential consequences of behaviors and actions. |
|||||||||||||||||||||||||||||||||||||||||
Diagnostic Impression |
The client is a 42-year-old Hispanic female who has a history of depression/panic symptoms, which have become more severe in the past month. The signs include anergia, anhedonia, reduced motivation, anxiety, focusing on numerous concerns, restlessness, palpitations, increased sensitivity to stress, impatience, oversleeping (up to 12 hours per day), and reduced appetite. Psychosis, hypomania, and delusional thinking are also absent in the client’s current condition.
Panic Disorder Severity Measure score is 38. The diagnostic considerations include the diagnosis of Major Depressive Disorder according to the ICD-10 code, which is F33.1, and Panic Disorder, whose ICD-10 code is F41.0. Based on the reported symptoms and screening results, these diagnoses are considered in the clinical impression. |
|||||||||||||||||||||||||||||||||||||||||
Treatment Plan |
1) Medication:
· Increase escitalopram 10mg po daily · Continue with alprazolam 2) Order labs 3) Patient has emergency numbers: Emergency Services 911, the national Crisis Line 800-273-TALK, the MHC Crisis Clinic. Patient was instructed to go to nearest ER or call 911 if they become actively suicidal and/or homicidal. 4) Time allowed for questions and answers provided. Provided supportive listening. 5) RTC in 30 days 6) Follow up with PCP for GI upset and headaches |
|||||||||||||||||||||||||||||||||||||||||
Narrative Answers
| Reimbursement Billing Code
For this session, I would use the reimbursement billing code 99204, an Evaluation and Management (E/M) code for a new patient needing a thorough medical history, assessment, and moderately difficult medical decision-making (Weida & Weida, 2022). The justification for this billing code includes the following: the evaluation lasted 48 minutes (11:03 AM to 11:51 AM), which aligns with the time-based criteria for 99204. The session involved assessing multiple complex psychiatric conditions, including depression and panic disorder, requiring detailed documentation and treatment planning. Medical decision-making included medication adjustments (increasing escitalopram dosage), continued prescription for alprazolam, and the need for follow-up care and safety planning. Required Documentation to Support DSM-5-TR Diagnoses, ICD-10 Coding, and Billing Code The following documentation is relevant in order to support the selected DSM-5-TR diagnoses, ICD-10 coding, and billing code: comprehensive patient history, including medical, psychiatric, and social history; detailed description of current symptoms, severity, and impact on daily functioning; results from standardized diagnostic screening tools (e.g., Severity Measure for Panic Disorder score of 38); a clear clinical impression explicitly tying symptoms to diagnostic criteria; thorough documentation of decision-making processes for diagnosis and treatment, including rationale for medication adjustments and follow-up planning; time spent on the evaluation and detailed account of services rendered during the session; and clear delineation of differential diagnoses and ruling out other potential conditions. Missing Pertinent Documentation The case scenario lacks the following pertinent components of documentation (at least 12 points): detailed family psychiatric history, full past psychiatric history, including previous diagnoses and treatment outcomes, medical history beyond somatic concerns of GI upset and headaches, further elaboration on current social support systems, documentation of current stressors contributing to symptom exacerbation, detailed risk assessment including previous suicidal or self-harming behaviors, documentation of the patient’s adherence to current medications, full neurological examination results to rule out organic causes, assessment of functional impairment in occupational and social settings, evidence of discussion regarding potential side effects of the prescribed medications, explicit rationale for the chosen DSM-5-TR diagnoses, and follow-up plan details, including specific goals and metrics for assessing progress. Legal and Ethical Dilemmas Related to Billing Practices Overbilling, upcoding, and fraudulent practices pose significant legal and ethical dilemmas in clinical settings. Overbilling refers to charging for services not rendered or overstating the complexity of the services. Upcoding involves using codes for higher reimbursement levels than justified by the care provided. Both practices can lead to legal penalties, loss of licensure, and damage to professional reputation (Burks et al., 2022). Strategies for Promoting Legal and Ethical Billing Practices Strategies include education and training, such as regular training on proper coding, billing procedures, and updates to regulatory requirements to ensure compliance, and implementing audits, such as routine internal audits to monitor billing practices and address discrepancies promptly (Bhati et al., 2023). Improving Documentation for Maximum Reimbursement According to Seligson et al. (2021), improving documentation can involve utilizing structured templates to ensure all relevant documentation elements are consistently captured, including specific details like precise symptom descriptions, functional impairments, and diagnostic test results to substantiate coding and billing decisions, comprehensive risk assessments to justify the complexity of medical decision-making, and timely updates to maintain accurate and up-to-date records of follow-up plans, patient progress, and changes in treatment strategies. |
References
Bhati, D., Deogade, M. S., & Kanyal, D. (2023). Improving patient outcomes through effective hospital administration: A comprehensive review. Cureus, 15(10), 1–12. https://doi.org/10.7759/cureus.47731
Burks, K., Shields, J., Evans, J., Plumley, J., Gerlach, J., & Flesher, S. (2022). A systematic review of outpatient billing practices. SAGE Open Medicine, 10(10), 205031212210990. https://doi.org/10.1177/20503121221099021
Seligson, M. T., Lyden, S. P., Caputo, F. J., Kirksey, L., Rowse, J. W., & Smolock, C. J. (2021). Improving Clinical Documentation of Evaluation and Management Care and Patient Acuity Improves Reimbursement as well as Quality Metrics. Journal of Vascular Surgery, 74(6). https://doi.org/10.1016/j.jvs.2021.06.027
Weida, T., & Weida, J. (2022). Outpatient E/M Coding Simplified. Family Practice Management, 29(1), 26–31. https://www.aafp.org/pubs/fpm/issues/2022/0100/p26.html
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Psychiatric Patient Evaluation
Instructions |
Use the following case template to complete Week 2 Assignment 1. Assign DSM-5-TR diagnoses and ICD-10 codes to the services documented in the case scenario. You will add your narrative answers to the assignment questions to the bottom of this template and submit them together as one document. | |||||||||||||||||||||||||||||||||||||||||
Identifying Information |
Identification was verified by stating their name and date of birth.
Time spent for evaluation: 1103am-1151am |
|||||||||||||||||||||||||||||||||||||||||
Chief Complaint |
“My primary doctor thinks I need more help than she can give me now.” | |||||||||||||||||||||||||||||||||||||||||
HPI |
42 young female was evaluated for psychiatric evaluation and referred by her primary care provider for worsening depression and panic symptoms. She is currently prescribed escitalopram 5mg po daily for depression, alprazolam 1mg po daily for anxiety.
Today, the client reported symptoms of worsening in past month for depression with anergia, anhedonia, motivation, reports anxiety, frequent worry, reports feeling restlessness, palpitations “feels like everything is closing in on me, can’t focus, hard time breathing,” no reported obsessive/compulsive behaviors. Client reported feelings like want to sleep and never wake up.. There is no evidence of psychosis or delusional thinking. Client denied past episodes of hypomania, hyperactivity, erratic/excessive spending, involvement in dangerous activities, self-inflated ego, grandiosity, or promiscuity. Client reports increased irritability and easily frustrated. Has low frustration tolerance, sleeping 10-12 hrs/24hrs, appetite decreased. She has somatic concerns with GI upset and headaches. Client denied any current binging/purging behaviors, denied withholding food from self or engaging in anorexic behaviors. No self-mutilation behaviors. |
|||||||||||||||||||||||||||||||||||||||||
Diagnostic Screening Results |
Screen of symptoms in the past week: Severity Measure for Panic Disorder = Total Score 38 |
|||||||||||||||||||||||||||||||||||||||||
Past Psychiatric and Substance Use Treatment |
· Entered mental health system when she was age 29 after a family suicide.
· Previous Psychiatric Hospitalizations: · Previous Detox/Residential treatments: · Previous psychotropic medication trials: sertraline (became suicidal), trazodone (worsened nightmares), bupropion (became suicidal) · Previous mental health diagnosis per client/medical record: |
|||||||||||||||||||||||||||||||||||||||||
Substance Use History |
Have you used/abused any of the following (include frequency/amt/last use):
Any history of substance related: · Blackouts: – · Tremors: – · DUI: – · D/T’s: – · Seizures: – Longest sobriety |
|||||||||||||||||||||||||||||||||||||||||
Psychosocial History |
Client was raised by single mother. She is married; has 2 children.
Employed at local day care as administrative assistant. Education: High School Diploma Denied current legal issues. |
|||||||||||||||||||||||||||||||||||||||||
Suicide / Homicide Risk Assessment |
Suicide Inquiry: Denies active suicidal ideations, intentions, or plans. | |||||||||||||||||||||||||||||||||||||||||
Mental Status Examination |
She is a 42 yo Hispanic female who looks her stated age. She is cooperative with examiner. She is disheveled, dressed appropriately. There is psychomotor restlessness. Her mood is anxious and mildly irritable. She denies any auditory or visual hallucinations. There is no evidence of any delusional thinking. She denies any current suicidal or homicidal ideation. |
|||||||||||||||||||||||||||||||||||||||||
Clinical Impression |
The client is a 42 yo Hispanic female who presents with a history of treatment for depression and panic symptoms.
Moods are anxious and irritable. She has reported symptoms related to her depression and panic. no evident mania/hypomania, no psychosis, denied current cravings for drugs/alcohol, exhibits no withdrawal symptoms, has somatic concerns of GI upset and headaches. At the time of disposition, the client adamantly denies SI/HI ideations, plans, or intent and has the ability to determine right from wrong and can anticipate the potential consequences of behaviors and actions. |
|||||||||||||||||||||||||||||||||||||||||
Diagnostic Impression |
[Student to provide DSM-5-TR diagnoses with ICD-10 coding]Double click inside this text box to add/edit text. Delete placeholder text when you add your answers. |
|||||||||||||||||||||||||||||||||||||||||
Treatment Plan |
1) Medication:
· Increase escitalopram 10mg po daily · Continue with alprazolam 2) Order labs 3) Patient has emergency numbers: Emergency Services 911, the national Crisis Line 800-273-TALK, the MHC Crisis Clinic. Patient was instructed to go to nearest ER or call 911 if they become actively suicidal and/or homicidal. 4) Time allowed for questions and answers provided. Provided supportive listening. 5) RTC in 30 days 6) Follow up with PCP for GI upset and headaches |
|||||||||||||||||||||||||||||||||||||||||
Narrative Answers
| [In 1-2 pages, address the following:
· What reimbursement billing code would you use for this session? Provide your justification for using this billing code. · Explain what pertinent information is required in documentation to support your chosen DSM-5-TR diagnoses, ICD-10 coding, and billing code. · Explain what pertinent documentation is missing from the case scenario and what other information would be helpful to narrow your coding and billing options. (There are at least 12 missing pertinent components of documentation). · Discuss legal and ethical dilemmas related to overbilling, upcoding, and fraudulent practices. Propose 2 strategies for promoting legal and ethical coding and billing practices within your future clinical roles. · Finally, explain how to improve documentation to support coding and billing for maximum reimbursement. Add your answers here. Delete instructions and placeholder text when you add your answers. |
References
Add APA-formatted citations for any sources you referenced
Delete instructions and placeholder text when you add your citations.
Psychiatric Patient Evaluation
READINGS
- DSM-5-TR
- American Psychiatric Association. (2020). Updates to DSM–5 criteria, text and ICD-10 codes.
- American Psychiatric Association. (2013). Insurance implications of DSM
- American Psychiatric Association. (2020). Coding and reimbursement.
- American Psychiatric Association. (2013). Numerical listing of DSM-5 diagnoses and codes (ICD-10-CM). In Diagnostic and statistical manual of mental disorders (5th ed.).
- Buppert, C. (2021). Nurse practitioner’s business practice and legal guide (7th ed.). Jones & Bartlett Learning.
- Chapter 9, “Reimbursement for Nurse Practitioner Services”
- Centers for Medicare & Medicaid Services. (2020). Your billing responsibilities.
- Stewart, J. G., & DeNisco, S. M. (2019). Role development for the nurse practitioner (2nd ed.). Jones & Bartlett Learning.
- Chapter 15, “Reimbursement for Nurse Practitioner Services”
- Understanding health insurance: A guide to billing and reimbursement.

