Primary Care Medication Management
Question One: First-Line Treatment Recommendations
The JNC 8 and the ACA/AHA guidelines for hypertension (HTN) treatment vary in the definition of HTN and proposals for the treatment regimens. However, both guidelines suggest the use of ACE inhibitor (ACEi), Angiotensin receptor blocker (ARB), and Calcium channel blocker (CCB) as standalone or combined doses for non-African African American patients. They also recommend the prescription of Thiazide diuretics and CCBs for African-American patients (tufts.edu). The differences in the medicine are because ACEi/ARBs tend to have a reduction in drug efficacy in lowering blood pressure in African American patients (Marti et al., 2019).
Do you need help with your assignment ? Contact us.
Question Two: Recommended Medications To Start With
Under JNC8 and the AHA/ACC guidelines, BP 146/92 is above elevated BP and is defined as HTN stage 1 and HTN stage 2 (tufts.edu). Further, an analysis of today’s results based on a 10-year risk of heart disease or stroke shows that Mrs Lyons has a low risk of cardiovascular disease. However, her blood pressure is poorly controlled. In this case, the initiation of medication is required. Therefore, recommendations include lifestyle interventions and using thiazide diuretics combined with calcium channel blockers. For thiazide diuretics class, I recommend hydrochlorothiazide, sold as Aquazide H/Hydrocotat with an initial dosage of 25 mg taken orally once daily. I recommend amlodipine for the channel blockers class, sold as Norvasc at 5 mg once daily. To decrease her LDL and triglycerides and allow HDL to increase, I recommend using statins, specifically Atorvastatin (Lipitor®), at a dosage of 40 mg daily.
Question Three: Mechanism of Action of the Listed Drugs
The mechanism of action of hydrochlorothiazide (Aquazide H/Hydrocotat) as a thiazide-type diuretic is not fully known. However, thiazides generally work by regulating and controlling how often the body passes water and salt is reabsorbed into the body (Khalil & Zeltser, 2022). After ingestion, thiazides increase the urination rate and inhibit salt reabsorption within the kidneys. By activating calcium-activated potassium channels in vascular smooth muscles and inhibiting various carbonic anhydrases in vascular tissue, thiazides cause blood vessels to dilate, lowering the blood pressure in return.
On the other hand, Norvasc, as a CCB medication, works by initiating a block on the transportation of calcium in the coronary arteries. As calcium plays a role in muscle contraction, blocking the transport and action of calcium relaxes arterial muscles, causing coronary arteries and other body arteries to dilate. The dilated arteries improve the blood flow to and from the heart. Amlodipine reduces blood pressure in the heart and the entire body. In turn, this reduces the risks of coronary and related vascular disease development (Khalil & Zeltser, 2022).
The atorvastatin (Lipitor®) action mechanism is similar to other statins. Atorvastatin works by competitively inhibiting the action of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase (McIver & Siddique, 2021). The inhibition of HMG-CoA reductase slows the liver’s cholesterol and other sterols synthesis. Lipitor also improves the action and number of hepatic LDL receptors on the cell surface, increasing catabolism and uptake of LDL and triglycerides in the liver and lowering plasma cholesterol and lipoprotein levels (McIver & Siddique, 2021).
Question Four: Side Effect Profile of the Listed Medication
After taking hydrochlorothiazide, there are fluctuations in glucose levels in the blood. Most patients may feel nausea, stomach upset, or dizziness as side effects directly related to the diuretic dose (Khalil & Zeltser, 2022). On the other hand, Norvasc’s side effects may include dizziness, drowsiness, tiredness, nausea, flushing, and swelling in the lower leg. In some rare cases, patients, after taking Norvasc, may experience deep pains, severe drowsiness, the feeling of passing out, and a pounding headache. Such cases require an emergency visit to the doctor. The significant side effects of atorvastatin include joint pain, a sore throat, cases of diarrhea, and sometimes muscle pains around the arms and legs (McIver & Siddique, 2021). In rare cases, patients may experience pain in the upper stomach, jaundice, total body weakness, difficulty breathing, and swelling of the face or throat. All rare cases need to be reported to the doctor immediately.
Question Five: Interactions between the Prescribed Medications
Hydrochlorothiazide displays severe to moderate interactions with other diuretics. It has also shown serious interactions with photosensitizers and other blood pressure medications. Hydrochlorothiazide interacts with bile acid-binding resins such as cholestyramine and colestipol. Similarly, Norvasc interacts with nitroglycerin, simvastatin (especially Zocor, Simcor, and Vytorin), and other heart or blood pressure medications. Atorvastatin use may increase plasma concentrations with a risk of myopathies. Drugs that induce the Cytochrome P450 3A4 may cause a decrease in atorvastatin concentrations in the plasma. Atorvastatin also increases the plasm concentrations of digoxin and the bioavailability of norethindrone and Ethinyl estradiol (McIver & Siddique, 2021).
Question Six: Non-Pharmacological Interventions
The JNC 8 and ACC/AHA guidelines recommend the adoption of lifestyle modifications such as the adoption of a healthy diet, reduction or abstinence from smoking and alcohol intake, and physical exercises as the first-line treatment for patients with elevated BP and HTN with no other significant comorbidities (Al-Ahmad et al., 2021). These non-pharmacological interventions may be adopted as either first-line recommendations or in addition to medical interventions. The non-pharmacological interventions eliminate or reduce the risks associated with medications in managing elevated BP, HTN, and high cholesterol in patients without severe comorbidities.
References
Al-Ahmad, M., Beiram, R., & AbuRuz, S. (2021). Application of the American College of Cardiology (ACC/AHA) 2017 Guideline for the Management of Hypertension in Adults and Comparison with the 2014 Eighth Joint National Committee Guideline. Journal of the Saudi Heart Association, 33(1), 16.
Khalil, H., & Zeltser, R. (2022). Antihypertensive medications. In StatPearls [Internet]. StatPearls Publishing.
Marti, C. N., Fonarow, G. C., Anker, S. D., Yancy, C., Vaduganathan, M., Greene, S. J., & Butler, J. (2019). Medication dosing for heart failure with reduced ejection fraction—opportunities and challenges. European journal of heart failure, 21(3), 286-296.
McIver, L., & Siddique, M. (2021). Atorvastatin. Ncbi.nlm.nih.gov. Retrieved 15 March 2022, from https://www.ncbi.nlm.nih.gov/books/NBK430779/#:~:text=Mechanism%20of%20Action%20Atorvastatin%20competitively%20inhibits%203-hydroxy-3-methylglutaryl-coenzyme%20A,LDL%20receptors%20on%20the%20surface%20of%20hepatic%20cells.
tufts.edu. (n.d.). Document: Hypertension: JNC- 8 (2014) vs Aha/ACC (2017). TUSK. Retrieved 14 March 2022, from https://tusk.tufts.edu/view/content/M3052C/2641554?SIZE=
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Mrs. Lyons is a 57-year-old African-American female who recently developed headaches and had an elevated blood pressure reading at her work health fair. When her blood pressure was taken at the health fair, the reading was 168/99. She has returned to the drugstore thrice to take her blood pressure. The lessons have been 145/90, 150/89, and 140/88. At the health fair, she was told her BMI was elevated. Her cholesterol levels were also measured at the health fair. The results were: total cholesterol level 250, LDL 138, HDL 48, and Triglycerides 170.
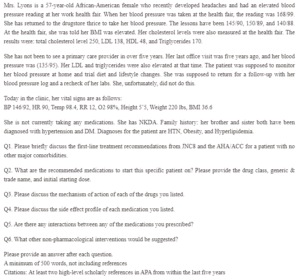
Primary Care Medication Management
She has not been to see a primary care provider in over five years. Her last office visit was five years ago, and her blood pressure was (135/95). Her LDL and triglycerides were also elevated at that time. The patient was supposed to monitor her blood pressure at home and trial diet and lifestyle changes. She was supposed to return for a follow-up with her blood pressure log and a recheck of her labs. She, unfortunately, did not do this.
Today in the clinic, her vital signs are as follows:
BP 146/92, HR 90, Temp 98.4, RR 12, O2 98%, Height 5’5, Weight 220 lbs, BMI 36.6
She is not currently taking any medications. She has NKDA. Family history: her brother and sister both have been diagnosed with hypertension and DM. Diagnoses for the patient are HTN, Obesity, and Hyperlipidemia.
Q1. Please briefly discuss the first-line treatment recommendations from JNC8 and the AHA/ACC for a patient with no other major comorbidities.
Q2. What are the recommended medications to start this specific patient on? Please provide the drug class, generic & trade name, and initial starting dose.
Q3. Please discuss the mechanism of action of each of the drugs you listed.
Q4. Please discuss the side effect profile of each medication you listed.
Q5. Are there any interactions between any of the medications you prescribed?
Q6. What other non-pharmacological interventions would be suggested?
Please provide an answer after each question
A minimum of 500 words, not including references
Citations: At least two high-level scholarly references in APA from within the last five years


