PICO(T) Questions and an Evidence-Based Approach – Diabetic Complications
Evidence-based approaches in chronic care have been lauded for their effectiveness in optimizing clinical outcomes and improving patient experiences. These approaches utilize the best available evidence to inform clinical decision-making and best practices in managing these conditions. The PICOT framework maintains significance in implementing these approaches in practice. This framework helps identify a health issue in management and guides the search for evidence that addresses the issue. It forms the groundwork for exploring scientific resources that form part of best practices in comprehensive care for chronic disorders. Long-term complications of diabetes remain an area in chronic care that can be explored using this framework. This paper analyses long-term complications of diabetes as a healthcare issue through the PICOT framework and identifies and analyzes sources that relate to diabetic complications.
Definition of a Practice Issue to be Explored Using the PICOT Framework
Diabetic complications remain a global concern, having been implicated in significant morbidity and mortality. Long-term complications of diabetes present a particular challenge to diabetic management due to their high potential to cause deterioration in the quality of life of individuals and even death. Microvascular complications are the most common causes of diabetic blindness, chronic kidney disease, and diabetic foot. These presentation causes significant functional deficits among people with diabetes and fetche considerable healthcare costs. Macrovascular complications such as stroke are more severe and have been implicated in significant mortalities (Albarakat & Guzu, 2019). The severity and consequence of these complications warrant their address.
The PICOT framework identifies specific issues within management that can be addressed effectively using best practices found in the literature. This framework will guide internet searches for evidence as it outlines care areas that need addressed. Specific concerns in the comprehensive care of long-term complications are fragmented approaches in care or poor care coordination. In this case, a PICOT formatted question will be: In diabetic patients with long-term complications of the disease presenting to the clinic (P), do care coordination and collaborative paradigms (I) confer any therapeutic benefit compared to fragmented approaches (C) in minimizing long term complications of diabetes (O) within 12 months (T) of home-based management. This PICOT question will give insight into best management practices in diabetic care that reduce the likelihood of developing diabetic complications. The interventions proposed in the questions may considerably improve the outcomes of patients with diabetes.
Sources of Evidence that Could be Potentially Effective in Answering a PICO(T) Question
Sources of evidence that can effectively answer this question include journal articles that detail the effectiveness of collaborative paradigms and care coordination approaches in patients with chronic disorders under home-based care. Journal articles on the coordination and continuum of care for diabetic patients transitioning to home-based approaches and those on the effectiveness of care coordination approaches in managing long-term complications of diabetes may as well be useful.
The article “Team-Based Care to Improve Diabetes Management: A Community Guide Meta-analysis” by Levengood et al. (2019) outlines team approaches in diabetic management. This article is potentially effective in answering the PICOT question outlined above as it details an intervention that can help reduce diabetic complications. It assesses the effectiveness of team-based care in chronicity and concludes that it lays the groundwork for comprehensive diabetes management and is vital in reducing the likelihood of long-term diabetic complications (Levengood et al., 2019). This article could thus potentially be used to address the PICOT question.
Another article that could potentially be used to answer the PICOT question is “Interprofessional Collaboration and Diabetes Management in Primary Care: A Systematic Review and Meta-Analysis of Patient-Reported Outcomes” by Nurchis et al. (2022). This article evaluates the impacts of interprofessional collaborations in comprehensive diabetes management through patient-reported outcomes. This article addresses the interventions and outcomes sections of the PICOT questions. Findings from the article reveal that inter-professional collaboration interventions positively impacted several aspects of diabetic care, including lowering the likelihood of diabetic complications and enhancing patient satisfaction with the care process (Nurchis et al., 2022). This article thus maintains utility in answering the PICOT question outlined.
The potential of the articles outlined above to answer the PICOT question was determined using the Ask, Access, Appraise, Apply, Audit (5As) model. In this criteria, a source or an article that addresses a component of the PICOT question is accessed via various web search tools and databases before being critiqued or appraised for its ability to answer the question effectively. The information in these sources is then applied to answer the question. Articles or sources that meet this criterion are chosen.
Findings from Articles or other Sources of Evidence as it Relates to the Identified Health Care Issue
The PICOT question outlined aims to establish the effectiveness of care coordination and collaborative paradigms in lessening the severity of risk for long-term complications of diabetes among diabetics under home-based care. Care coordination and collaborative approaches are best practices identified in the literature that maintain significance in the comprehensive management of diabetes. These approaches are based on teamwork, communications, role interdependence, and information sharing (Levengood et al., 2019). Care coordination synchronizes care approaches offered by diverse healthcare professionals available in healthcare toward optimizing care outcomes and enhancing patient experiences.
Care coordination approaches have been associated with reduced risk for diabetic complications. Care coordination also provides the groundwork for patient-centred care to prevent diabetic complications. This approach tailors care provision toward the beliefs and values of individual patients. It provides a platform for identifying factors contributing to patients’ diseases and may unearth factors leading to disease exacerbation and subsequent complications (Levengood et al., 2019). This highlights their utility in preventing long-term complications of the disease. The source used met the credibility criteria of timeliness, relevancy, purpose, authority, and accuracy.
Relevance of the Findings from Chosen Sources of Evidence to Making Decisions Related to a PICO(T) Question
Findings from the chosen sources maintain relevance in answering the PICOT question outlined. The finding affirms collaborative paradigms and care-coordination approaches as best practices in comprehensive diabetes management that considerably lower the incidence of diabetic complications. This addresses the outcome and intervention portions of the PICOT framework. Abdulrhim et al. (2021) assert that collaborative care models optimize diabetic management and may help reduce long-term complications of diabetes. This reinforces the significance of this approach and explains the need for its preferential utility of fragmented approaches. Findings from this source demonstrate its relevance to diabetic care. It informs best practices that can be used in preventing long-term complications of the disease.
Findings from the literature also point to the downside of fragmented care approaches that answer the comparison part of the PICOT question outlined. Kailasam et al. (2019) report that a fragmented care approach in diabetic care is associated with quality compromises in care provision, which in turn puts the patients at a higher risk for developing diabetic complications. This reinforces the need for a paradigm shift from fragmented care approaches to care coordination utilizing collaborative paradigms to prevent diabetic complications. Findings from this source are also valuable in informing best practices in diabetes management.
Conclusion
Long-term complications of diabetes remain a health concern. These complications have been implicated in the deterioration of the quality of life and mortalities. The PICOT framework provides a tool for identifying issues with diabetes management and guides searches for evidence to address these issues. Journal articles and organizational websites are vital sources from which evidence-based best practices can be obtained. These pieces of evidence detail effective and best practices in preventing long-term complications of the disease and answer the PICOT question outlined.
References
Abdulrhim, S., Sankaralingam, S., Ibrahim, M. I., Diab, M. I., Hussain, M. A., Al Raey, H., Ismail, M. T., & Awaisu, A. (2021). Collaborative Care Model for diabetes in primary care settings in Qatar: A qualitative exploration among healthcare professionals and patients who experienced the service. BMC Health Services Research, 21(1). https://doi.org/10.1186/s12913-021-06183-z
Albarakat, M., & Guzu, A. (2019). Prevalence of type 2 diabetes and its complications among home health care patients at Al-Kharj Military Industries Corporation Hospital. Journal of Family Medicine and Primary Care, 8(10), 3303. https://doi.org/10.4103/jfmpc.jfmpc_634_19
Kailasam, M., Guo, W., Hsann, Y. M., & Yang, K. S. (2019). Prevalence of care fragmentation among outpatients attending specialist clinics in a Regional Hospital in Singapore: A cross-sectional study. BMJ Open, 9(3). https://doi.org/10.1136/bmjopen-2018-022965
Levengood, T. W., Peng, Y., Xiong, K. Z., Song, Z., Elder, R., Ali, M. K., Chin, M. H., Allweiss, P., Hunter, C. M., & Becenti, A. (2019). Team-based care to improve diabetes management: A Community Guide meta-analysis. American Journal of Preventive Medicine, 57(1). https://doi.org/10.1016/j.amepre.2019.02.005
Nurchis, M. C., Sessa, G., Pascucci, D., Sassano, M., Lombi, L., & Damiani, G. (2022). Interprofessional collaboration and Diabetes Management in Primary Care: A systematic review and meta-analysis of patient-reported outcomes. Journal of Personalized Medicine, 12(4), 643. https://doi.org/10.3390/jpm12040643
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Create a 3-5 page submission in which you develop a PICO(T) question for a specific care issue and evaluate the evidence you locate, which could help to answer the question.
PICO(T) Questions and an Evidence-Based Approach – Diabetic Complications
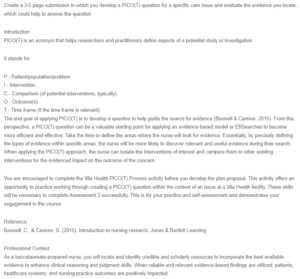
Introduction
PICO(T) is an acronym that helps researchers and practitioners define aspects of a potential study or investigation.
It stands for:
P – Patient/population/problem.
I – Intervention.
C – Comparison (of potential interventions, typically).
O – Outcome(s).
T – Time frame (if the time frame is relevant).
The end goal of applying PICO(T) is to develop a question to help guide the search for evidence (Boswell & Cannon, 2015). From this perspective, a PICO(T) question can be a valuable starting point for applying an evidence-based model or EBSearches to become more efficient and effective. Take the time to define the areas where the nurse will look for evidence. Essentially, by precisely defining the types of evidence within specific areas, the nurse will be more likely to discover relevant and useful evidence during their search. When applying the PICO(T) approach, the nurse can isolate the interventions of interest and compare them to other existing interventions for the evidenced impact on the outcome of the concern.
You are encouraged to complete the Vila Health PICO(T) Process activity before you develop the plan proposal. This activity offers an opportunity to practice working through creating a PICO(T) question within the context of an issue at a Vila Health facility. These skills will be necessary to complete Assessment 3 successfully. This is for your practice and self-assessment and demonstrates your engagement in the course.
Reference
Boswell, C., & Cannon, S. (2015). Introduction to nursing research. Jones & Bartlett Learning.
Professional Context
As a baccalaureate-prepared nurse, you will locate and identify credible and scholarly resources to incorporate the best available evidence to enhance clinical reasoning and judgment skills. When reliable and relevant evidence-based findings are utilized, patients, healthcare systems, and nursing practice outcomes are positively impacted.
PICO(T) is a framework that can help you structure your definition of the issue, a potential approach you will use, and your predictions related to the issue. Word choice is important in the PICO(T) process because different word choices for similar concepts will lead you to different existing evidence and research studies to help develop your initial question. When writing a PICO(T)-formatted research question, you want to focus on the intervention’s impact and compare the outcome you desire.
Scenario
For this assessment, please use a healthcare issue of interest from your current or past nursing practice.
If you do not have an issue of interest in your nursing practice, review the optional Case Studies presented in the resources and select one of those as the basis for your assessment.
Instructions
For this assessment, select a healthcare issue of interest and apply the PICO(T) process to develop and research the research question.
Your initial goal is to define the population, intervention, comparison, and outcome. In some cases, a time frame is relevant, and you should include that when writing a question, you can research related to your issue of interest. After you define your question, research it, and organize your initial findings, select the two sources of evidence that seem the most relevant to your question and analyze them more deeply. Specifically, interpret each source’s specific findings and best practices related to you and explain how the evidence would help you plan and make decisions related to your question.
If you need some structure to organize your initial thoughts and research, the PICOT Question and Research Template document (accessible from the “Create PICO(T) Questions” page in the Capella Library’s Evidence-Based Practice guide) might be helpful.
In your submission, make sure you address the following grading criteria:
Define a practice issue to be explored via a PICO(T) approach. Create a PICO(T)-formatted research question
Identify sources of evidence that could be potentially effective in answering a PICO(T) question (databases, journals, websites, etc.).
Explain the findings from articles or other sources of evidence related to the identified healthcare issue.
Explain the relevance of the findings from chosen sources of evidence to making a decision related to a PICO(T) question.
Communica that is clear, logical, and professional with correct grammar and spelling using the current APA style.

