Pharmacological Treatments for Arthritis
| MEDICATION
generic and trade name drug classification |
Medication Mechanism of
Action |
Common
Side Effects |
Pertinent
Nursing Implications & Patient Teaching |
| Ibuprofen
Classification: Non-steroidal anti-inflammatory drugs (NSAIDs)
|
Non-selective cyclooxygenase (COX) inhibitor: Inhibits cyclooxygenase 1 and cyclooxygenase two isoenzymes, leading to decreased prostaglandin synthesis. COX enzyme in the arachidonic pathway converts arachidonic acid to prostaglandin H2 and prostaglandins. Inhibition of COX enzymes, therefore, blocks the arachidonic pathway, inhibiting prostaglandin synthesis (Ngo & Bajaj, 2022). | – Epigastric pain
– Tinnitus – Heartburn – Dizziness – Rash – Nausea – Vomiting – Constipation – Edema – Headache – Agranulocytosis – Acute renal failure |
– Use with caution in patients with cardiovascular diseases such as myocardial infarction.
– Advise the patient to take oral ibuprofen with food to prevent gastrointestinal adverse effects such as heartburn and epigastric pain. – Advise the patient to take ibuprofen as prescribed. |
| Methotrexate
Classification: Antineoplastics, Antimetabolite
|
Dihydrofolic acid reductase inhibitor: purine and pyrimidine are required for DNA synthesis. Methotrexate inhibits dihydrofolic acid reductase required for DNA synthesis and, therefore, inhibits DNA synthesis, cellular replication, and DNA repair (Hannoodee & Mittal, 2022). | – Hyperuricemia
– Nausea and vomiting – Arachnoiditis when administered through the intrathecal route – Glossitis – Reddening of the skin – Leukopenia – Renal failure – Azotemia – Ulcerative stomatitis – Anorexia – Mucositis depending on the dose of methotrexate – Thrombocytopenia – Leukopenia – Nephropathy
|
– Monitor the patient for signs of infection and bone marrow suppression.
– Monitor the patient for signs of tumor lysis syndrome, renal toxicity, and hepatotoxicity. – Methotrexate is not administered in pregnancy and lactation. – Patients who have difficulty swallowing are given oral methotrexate solution. – Advise the patient to measure the dose of oral methotrexate solution using an oral syringe provided by the pharmacist since household items such as a spoon can lead to an overdose or underdose. – Advise the patient to take oral methotrexate as prescribed. – Advise the patient to take the recommended dose weekly and not daily. – Advise the patient to take methotrexate with or without food. – Advise the patient on the importance of folic acid supplementation (Hannoodee & Mittal, 2022). |
| Leflunomide
Classification: Disease-modifying antirheumatic drugs (DMARDs)
|
Inhibits pyrimidine synthesis: Inhibits the activity of dihydroorotate dehydrogenase enzyme required for the synthesis of pyrimidine ribonucleotide uridine monophosphate in the de novo synthesis (Padda & Goyal, 2022). | – Respiratory infections
– Diarrhea – Hypertension – Alopecia – Nausea – Ras – Bronchitis – Abdominal pain – Urinary tract infections – Dyspepsia – Headache – Back pain |
– Monitor the liver function monthly in the first six months of taking leflunomide, then monitor after every eight weeks.
– Interrupt leflunomide therapy if the alanine transaminase enzyme is more than thrice the upper limit value and initiate cholestyramine until the alanine transaminase value is back within the normal range (Padda & Goyal, 2022). – Advise the patient to take leflunomide as prescribed. – Leflunomide is not administered in pregnancy and lactation. – Advise women of childbearing age to use contraception. |
| Hydroxychloroquine
Classification: Aminoquinoline, Disease-modifying antirheumatic drugs (DMARDs) |
Anti-inflammatory and immunomodulatory. | – Blood and lymphatic disorders include aplastic anemia, bone marrow failure, thrombocytopenia, hemolysis, and bone marrow failure.
– Ear disorders such as deafness, tinnitus, and nerve deafness. – Gastrointestinal disorders such as abdominal pain, diarrhea, nausea, and vomiting – Hepatobiliary disorders such as acute hepatic failure – Nutrition disorders such as weight loss, loss of appetite, and porphyria – Psychiatric disorders such as irritability, psychosis, and suicidal ideation – Cardiac disorders such as ventricular arrhythmias and QT prolongation |
– Monitor the patient for renal and cardiac function (Singh et al., 2022).
– Advise the patient to take hydroxychloroquine as prescribed. – Advise the patient to take hydroxychloroquine with food or a glass of milk. – Advise the patient not to split or crush tablets.
|
| Infliximab
Classification: Tumour necrosis factor-alpha (TNF-alpha) inhibitors |
TNFα inhibitor. Infliximab has a high affinity for transmembrane and soluble TNFα. Binding to TNFα prevents TNFα from binding to receptors, preventing intestinal and synovial inflammation (Fatima et al., 2022). | – Infection
– Infusion-related reactions – Upper respiratory infections – Headache – Development of antinuclear bodies – Abdominal pain – Development of antibodies to double-stranded DNA – Diarrhea – Bronchitis – Fatigue – Rhinitis |
– Monitor the patient for signs of infection
– Monitor the patient for infusion-related reactions – Monitor the patient for elevated alanine transaminase – Discontinue in case of infusion-related reactions, infection, or sepsis. – After administration, discard unused portions since infliximab lacks antibacterial preservatives (Fatima et al., 2022). – Do not infuse in the same intravenous line with other drugs |
| Anakinra
Classification: Disease-modifying antirheumatic drugs (DMARDs) |
Interleukin 1 receptor antagonist: interleukin 1β and interleukin 1α stimulate the inflammatory cascade by stimulating the production of TNFα and cytokines. Anakinra blocks the activity of interleukin 1β, and interleukin 1α prevents the occurrence of an inflammatory cascade (Bedaiwi et al., 2022). | – Headache
– Injection site reaction – Vomiting – Pyrexia – Arthralgia – Nasopharyngitis – Diarrhea – Nausea – Neutropenia
|
– Monitor the patient for injection site reactions
– Monitor the patient for signs of infection – Monitor the patient for hypersensitivity reactions – Discontinue treatment in severe hypersensitivity reactions – Do not coadminister with live vaccines – Educate the patient on how to identify signs of infection and sepsis |
| Abatacept
Classification: Disease-modifying antirheumatic drugs (DMARDs) |
T lymphocyte activation inhibitor: Antigen-presenting cells (APCs) are required for the complete activation of T cells. Abatacept prevents APCs from delivering costimulatory signals, preventing complete activation of T cells and causing downregulation of T cells (Lauper et al., 2022). | – Headache
– Infections – Nasopharyngitis – Nausea – Hypertension – Urinary tract infection – Dizziness – Back pain – Pain in the extremities – Cough – Dyspepsia – Rash |
– Monitor the patient for signs of anaphylaxis and hypersensitivity reactions.
– Monitor the patient for infusion-related reactions – Monitor for signs of infections
|
| Rituximab
Classification: Disease-modifying antirheumatic drugs (DMARDs), Monoclonal antibodies |
Binds to the CD20 antigen, activating antibody or complement-mediated cytolysis (Hanif & Anwer, 2022). | – Angioedema
– Pruritis – Chills – Asthenia – Fever – Headache – Abdominal pain – Lymphopenia – Night sweats – Cough – Infection – Rhinitis – Infusion reactions – Nausea |
– Monitor the patient for infusion-related reactions.
– Advise women of childbearing age to use contraceptives during treatment and for 12 months after treatment – Premeducate the patient with antihistamine and acetaminophen before administration (Hanif & Anwer, 2022). – Administered as an intravenous infusion |
| MEDICATION
generic and trade name drug classification |
Medication Mechanism of
Action |
Common
Side Effects |
Pertinent
Nursing Implications & Patient Teaching |
| Golimumab
Classification: Tumour necrosis factor-alpha (TNF-alpha) inhibitors |
Binds to bioactive and soluble TNFα, preventing TNFα from binding to its receptors and blocking TNFα biological activity (Padda et al., 2022). | – Upper respiratory tract infection
– Viral infections such as herpes – Injection site reactions such as pain, pruritis, and paresthesia – Hypertension – Paraesthesia |
– Monitor alanine transaminase and aspartate transaminase
– Monitor the patient for signs of infection and sepsis. – Discontinue sepsis and severe infection. – Injection must be colorless to light yellow. A discolored or opaque injection is discarded – Administered in different intravenous lines with other agents |
| Tocilizumab
Classification: Monoclonal antibodies (Interleukin 6 receptor inhibitors) |
Interleukin 6 receptor antagonist inhibits protein synthesis, T cell activation, and immunoglobin secretion (Preuss & Anjum, 2022). | – Subcutaneous injection sites’ reaction
– Upper respiratory tract infection – Constipation – Nasopharyngitis – Hypertension – Headache – Bronchitis – Mouth ulceration – Rash |
– Monitor the patient for injection site reactions.
– Do not administer as a bolus. – Monitor for signs of infections. – Discontinue therapy in case of an infection.
|
References
Bedaiwi, M. K., Almaghlouth, I., & Omair, M. A. (2021). Effectiveness and adverse effects of anakinra in the treatment of rheumatoid arthritis: a systematic review. European review for medical and pharmacological sciences, 25(24), 7833–7839. https://doi.org/10.26355/eurrev_202112_27630.
Fatima, R., Bittar, K., & Aziz, M. (2022). Infliximab. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK500021/.
Hanif, N., & Anwer, F. (2022). Rituximab. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK564374.
Hannoodee, M., & Mittal, M. (2022). Methotrexate. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556114/.
Lauper, K., Iudici, M., Mongin, D., Bergstra, S. A., Choquette, D., Codreanu, C., Cordtz, R., De Cock, D., Dreyer, L., Elkayam, O., Hauge, E. M., Huschek, D., Hyrich, K. L., Iannone, F., Inanc, N., Kearsley-Fleet, L., Kristianslund, E. K., Kvien, T. K., Leeb, B. F., Lukina, G., Finckh, A. (2022). Effectiveness of TNF-inhibitors, abatacept, IL6-inhibitors, and JAK-inhibitors in 31 846 patients with rheumatoid arthritis in 19 registers from the ‘JAK-pot’ collaboration. Annals of the rheumatic diseases, 81(10), 1358–1366. https://doi.org/10.1136/annrheumdis-2022-222586.
Ngo, V. T. H., & Bajaj, T. (2022). Ibuprofen. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542299/.
Padda, I. S., & Goyal, A. (2022). Leflunomide. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557799/.
Padda, I. S., Bhatt, R., & Parmar, M. (2022). Golimumab. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK576392/.
Preuss, C. V, & Anjum, F. (2022). Tocilizumab. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK570644/.
Singh, A., Kotlo, A., Wang, Z., Dissanayaka, T., Das, S., & Antony, B. (2022). Efficacy and safety of hydroxychloroquine in osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. The Korean journal of internal medicine, 37(1), 210–221. https://doi.org/10.3904/kjim.2020.605.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Purpose of the Assignment
Identify the common pharmacologic treatments for inflammatory diseases of the human body.
Review the potential effects medication has on the clients’ basic care and comfort needs.
Identify nursing interventions meeting the basic care and comfort needs of clients receiving these pharmacological agents.
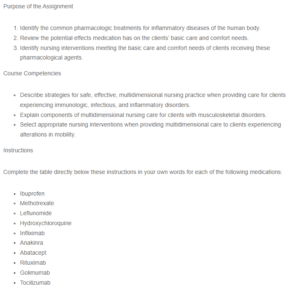
Pharmacological Treatments for Arthritis
Course Competencies
- Describe strategies for safe, effective, multidimensional nursing practice when providing care for clients experiencing immunologic, infectious, and inflammatory disorders.
- Explain components of multidimensional nursing care for clients with musculoskeletal disorders.
- Select appropriate nursing interventions when providing multidimensional care to clients experiencing alterations in mobility.
Instructions
Complete the table directly below these instructions in your own words for each of the following medications:
- Ibuprofen
- Methotrexate
- Leflunomide
- Hydroxychloroquine
- Infliximab
- Anakinra
- Abatacept
- Rituximab
- Golimumab
- Tocilizumab
Use at least two scholarly sources to support your findings. Be sure to cite your sources in-text and on a reference page using APA format.


