Peer Responses – Case of an Asthma Patient
Peer Response 1: Hamid
Hello,
This is a great post. The differential diagnosis for Timothy is thorough, covering the most plausible conditions associated with his symptoms. Assuming asthma exacerbation as the primary issue is reasonable because of Timothy’s history of asthma and more utilization of albuterol, including upper respiratory infection (URI) and allergic rhinitis as the causes of his symptoms show a more specific differential diagnosis, which also shows an understanding of how these conditions may occur in tandem, especially in children with a history of atopy.
An area for further exploration is the consideration of environmental or seasonal factors that exacerbate Timothy’s asthma. Cold air or changes in weather will cause asthma to worsen (Chabra & Gupta, 2023). Also, asking questions about changes in Timothy’s environment that include exposure to smoke, allergens, or stress can help identify any contributing factors.
Further, the devised therapy regimen is compatible with contemporary treatment standards, especially the two-step strategy with albuterol for symptom control and fluticasone for sustained therapy. This approach aligns with the Global Initiative for Asthma (GINA) frameworks, particularly regarding the use of inhaled corticosteroids for persistent asthma (Papi et al., 2020). Patient education is still paramount in enhancing compliance with long-term management strategies. Engaging Timothy’s mother in these talks is essential so as to explain why certain medications are essential for the child and remind her of the implications of missing doses.
Concerning antibiotic therapy in managing acute otitis media (AOM), the choice of high-dose amoxicillin is relevant, especially with regard to the presence of antibiotic resistance. An example of a possible substitute is amoxicillin-clavulanate if, for example, Timothy has had multiple cumulative AOM or if there are a large number of resistant organisms in the population (Gavrilovici et al., 2022). It is also important to follow up, particularly in pediatric patients, for assessment of resolution and to rule out any compounding complications.
References
Chabra, R., & Gupta, M. (2023). Allergic and environmental-induced asthma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526018/
Gavrilovici, C., Spoială, E.-L., Miron, I.-C., Stârcea, I. M., Haliţchi, C. O. I., Zetu, I. N., Lupu, V. V., & Pânzaru, C. (2022). Acute otitis media in children—Challenges of antibiotic resistance in the post-vaccination era. Microorganisms, 10(8), 1598. https://doi.org/10.3390/microorganisms10081598
Papi, A., Blasi, F., Canonica, G. W., Morandi, L., Richeldi, L., & Rossi, A. (2020). Treatment strategies for asthma: Reshaping the concept of asthma management. Allergy, Asthma & Clinical Immunology, 16(1). https://doi.org/10.1186/s13223-020-00472-8
Peer Response 2: Devon
Hello,
Great work with your post. The assessment of Timothy’s case is commendable, particularly in how the differential diagnoses for his presenting symptoms are navigated. To focus on asthma exacerbation as the most probable diagnosis is justified and stems from the absence of any recent inhaler use or Timothy’s previous history. This depicts the importance of patients taking their medicine when they have asthmatic symptoms, which is well supported by Hashmi et al.’s (2023) report. Hashmi et al. (2023) emphasize the need to ensure that the patients and their families have adequate information sessions to ensure they understand that they need to manage the conditions continuously and not wait until serious signs and symptoms appear.
An addition to the current study could include an exploration of the relationship of inhaler technique to the management of asthma. Improper usage of inhalation devices skews the effectiveness of medicines and can worsen asthma (Alotaibi et al., 2023). Timothy and his mother may benefit from an actual example of a demonstration of the proper inhaler technique during their clinic visit, accompanied by the discussion of possible challenges such as cost or medication availability.
The differential diagnosis of ear pain covers all the possible and unlikely causes of the condition. Even though acute otitis media is a common reason for ear pain in children, especially after upper respiratory infections, it is also important to consider eustachian tube dysfunction depending on the perspective of Timothy having asthma and allergic rhinitis (Danishyar & Ashurst, 2023). Notably, the main causes of eustachian tube dysfunction include inflammation of the upper respiratory tract, and therefore, children with asthma are at a higher risk.
Using emollients together with topical corticosteroids to manage Timothy’s atopic dermatitis is relevant, as endorsed by (Ridd et al., 2023). It would also be valuable to investigate possible psychosocial consequences of atopic dermatitis, especially if it is severe and long-standing. This shows that chronic skin disorders in children are psychosocial stressors that worsen symptoms based on the study. Meeting these concerns comprehensively will likely enhance the overall performance of the treatments being offered.
References
Alotaibi, M. M., Hughes, L., & Ford, W. R. (2023). Assessing inhaler techniques of asthma patients using aerosol inhalation monitors (AIM): A cross-sectional study. Healthcare, 11(8), 1125. https://doi.org/10.3390/healthcare11081125
Danishyar, A., & Ashurst, J. V. (2023). Acute otitis media. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470332/
Hashmi, M. F., Tariq, M., & Cataletto, M. E. (2023, May 3). Asthma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430901/
Ridd, M. J., Wells, S., MacNeill, S. J., Sanderson, E., Webb, D., Banks, J., Sutton, E., Shaw, A. R., Wilkins, Z., Clayton, J., Roberts, A., Garfield, K., Liddiard, L., Barrett, T. J., Lane, J. A., Baxter, H., Howells, L., Taylor, J., Hay, A. D., & Williams, H. C. (2023). Comparison of lotions, creams, gels and ointments for the treatment of childhood eczema: The BEE RCT. Health Technology Assessment (Winchester, England), 27(19), 1–120. https://doi.org/10.3310/GZQW6681
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
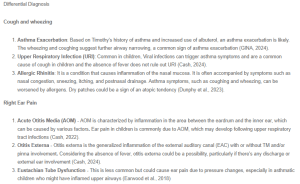
Differential Diagnosis
Cough and wheezing
- Asthma Exacerbation: Based on Timothy’s history of asthma and increased use of albuterol, an asthma exacerbation is likely. The wheezing and coughing suggest further airway narrowing, a common sign of asthma exacerbation (GINA, 2024).
- Upper Respiratory Infection (URI): Common in children, Viral infections can trigger asthma symptoms and are a common cause of cough in children and the absence of fever does not rule out URI (Cash, 2024).
- Allergic Rhinitis: It is a condition that causes inflammation of the nasal mucosa. It is often accompanied by symptoms such as nasal congestion, sneezing, itching, and postnasal drainage. Asthma symptoms, such as coughing and wheezing, can be worsened by allergens. Dry patches could be a sign of an atopic tendency (Dunphy et al., 2023).
Peer Responses – Case of an Asthma Patient
Right Ear Pain
- Acute Otitis Media (AOM) – AOM is characterized by inflammation in the area between the eardrum and the inner ear, which can be caused by various factors. Ear pain in children is commonly due to AOM, which may develop following upper respiratory tract infections (Cash, 2022).
- Otitis Externa – Otitis externa is the generalized inflammation of the external auditory canal (EAC) with or without TM and/or pinna involvement. Considering the absence of fever, otitis externa could be a possibility, particularly if there’s any discharge or external ear involvement (Cash, 2024).
- Eustachian Tube Dysfunction – This is less common but could cause ear pain due to pressure changes, especially in asthmatic children who might have inflamed upper airways (Earwood et al., 2018)
Dry, Scaly Patches
- Atopic Dermatitis – Common in children with asthma, characterized by dry, itchy, scaly patches on elbows and knees (Chu et al., 2024).
- Psoriasis – While less common in young children, psoriasis can also present with dry, scaly patches but typically has more defined borders compared to atopic dermatitis (Cash, 2024).
- Contact Dermatitis – Possible allergic reaction to an irritant or allergen; however, the chronicity and location of the patches favor a more systemic cause like atopic dermatitis (Cash, 2024).
Final Diagnoses
- Asthma Exacerbation
- Acute Otitis Media
- Atopic Dermatitis
Plan
Asthma Exacerbation
- Albuterol HFA inhaler, 90 mcg/actuation, take 2 puffs 4 – 6 hours as needed for wheezing or shortness of breath. Dispense: 1 inhaler (200 puffs). Refill: 2
- Albuterol is a short-acting beta-2 agonist (SABA) that provides quick relief of bronchospasm. It’s the first-line treatment for acute asthma symptoms (GINA, 2024)
- Fluticasone Propionate inhaler, 44 mcg/actuation, take 2 puffs BID. Dispense: 1 inhaler (120 puffs). Refills: 2
- Inhaled corticosteroids (ICS) like fluticasone are the cornerstone of long-term asthma management. They reduce airway inflammation and prevent exacerbations (GINA, 2024).
- This dual approach helps control Timothy’s asthma more effectively by addressing both acute symptoms and long-term inflammation (GINA, 2024).
- Patient Education: Teach Timothy’s mother the proper technique for inhaler use, the importance of regular use of the maintenance inhaler, and when to use the rescue inhaler.
- Follow UP: 2 weeks to assess asthma control.
Acute Otitis Media
When antibiotics are prescribed, the recommended first-line therapy is high-dose amoxicillin. This is usually given at a dosage of 80 to 90 mg per kg per day, divided into two doses. However, if the patient has recently taken amoxicillin for acute otitis media (AOM) or has purulent conjunctivitis, amoxicillin/clavulanate is typically used instead (Gaddey et al., 2019). Assuming Timothy is 21 kg. His calculated dose would be 11.875 ml or 950 mg twice a day
- Amoxicillin 400 mg/5ml suspension. Give 12 mL (960 mg) by mouth twice a day for 10 days. Dispense: 250 ml. Refill: 0
- This dosage adheres to the guideline-recommended 90 mg/kg/day for AOM. The higher dosage is recommended to overcome antibiotic resistance in common AOM pathogens (Gaddey et al., 2019).
- Patient Education
- Educated mother the importance of completing the 10-day course of antibiotics even if symptoms are improved.
- Instructed mother on the use of medication syringe and dosing cup.
- Advised to follow any instructions provided by the pharmacist
- Follow up: Advised Timothy’s mother to return if symptoms worsen or do not improve within 48-72 hours, as this could indicate treatment failure or complications
Atopic Dermatitis
- Hydrocortisone 1% cream. Apply thinly to affected areas twice daily for up to 14 days. Dispense: 1 tube. Refill: 0
- Topical corticosteroids, like hydrocortisone, can effectively alleviate inflammation and itching associated with atopic dermatitis. This treatment is effective in managing symptoms and preventing further complications caused by excessive scratching, which can result in secondary infections (AAP, 2021).
- Patient Education: Discussed moisturizing techniques, identifying triggers, and applying topical steroids properly to manage atopic dermatitis.
- Follow up: As needed if symptoms do not resolve or worsen.
PEER RESPONSE 2:
Devon Brush posted Aug 13, 2024 1:33 PM
When Timothy arrives to the clinic, with the complaints of wheezing, ear pain and dry scaly patches a thorough history and physical exam should be conducted to appropriately diagnose him. Timothy’s history of asthma and recent wheezing suggests that his cough may be due to poorly controlled asthma. The Global Initiative for Asthma (GINA) guidelines emphasize that wheezing in an asthmatic child who has not been adherent to regular follow-up and who lacks proper medication management, such as running out of an albuterol inhaler, is a red flag for poorly controlled asthma (Global Initiative for Asthma, 2022).
Potential Differential Diagnoses (DDx) for Cough and Wheezing:
- Asthma Exacerbation: The most likely cause of Timothy’s cough and wheezing is an asthma exacerbation, given his history and recent lack of inhaler use. Poor medication adherence and lack of routine monitoring could exacerbate his symptoms (Global Initiative for Asthma, 2022).
- Viral Upper Respiratory Infection (URI): A viral URI can trigger asthma symptoms and cause cough and wheezing in children. The absence of fever might suggest a viral etiology rather than bacterial.
- Allergic Rhinitis: Given the chronic nature of asthma, an allergic component could be contributing to Timothy’s symptoms. Allergens might induce both cough and wheezing in susceptible individuals.
Final Diagnosis: The most likely diagnosis for Timothy’s cough and wheezing is an asthma exacerbation (Global Initiative for Asthma, 2022).
Right Ear Pain:
Potential Differential Diagnoses (DDx) for Ear Pain:
- Acute Otitis Media (AOM): This condition is common in children and often presents with ear pain. Timothy’s ear pain without systemic symptoms such as fever might still indicate AOM, particularly if there has been recent inflammation or infection (Danishyar & Ashurst, 2023).
- Otitis Externa: Also known as “swimmer’s ear,” this condition can cause ear pain, especially if there’s a history of water exposure.
- Eustachian Tube Dysfunction: Eustachian tube dysfunction could cause ear pain and pressure due to blockage or improper drainage, potentially associated with Timothy’s asthma or allergic rhinitis.
Final Diagnosis: The most likely diagnosis for Timothy’s ear pain is acute otitis media (Danishyar & Ashurst, 2023).
Dry, Scaly Patches:
Potential Differential Diagnoses (DDx) for Skin Lesions:
- Atopic Dermatitis (Eczema): The presence of dry, scaly patches on the elbows and behind the knees is characteristic of eczema, especially in a child with a history of asthma, as atopic diseases often coexist (National Eczema Association, 2017).
- Psoriasis: Psoriasis can also present with scaly patches, although the distribution in children is less common in the flexural areas.
- Contact Dermatitis: If Timothy has been exposed to an irritant or allergen, this could lead to localized dermatitis with dry, scaly patches.
Final Diagnosis: The most likely diagnosis for Timothy’s skin lesions is atopic dermatitis (National Eczema Association, 2017).
Plan of Care
Asthma Exacerbation:
- Medications:
- Albuterol Inhaler: 90 mcg/actuation, 2 puffs every 4-6 hours as needed for wheezing.
- Inhaled Corticosteroid (ICS): Prescribe a low-dose ICS such as Fluticasone, 44 mcg/puff, 2 puffs twice daily to prevent future exacerbations.
- Spacer Device: Recommend using a spacer with the inhaler to improve medication delivery.
- Patient Education:
- Teach proper inhaler technique, emphasizing the importance of adherence to controller medication (ICS) to prevent exacerbations.
- Advise on the recognition of asthma exacerbation signs and the need to seek prompt medical care if symptoms worsen.
- Follow-Up:
- Schedule a follow-up visit in 2 weeks to reassess asthma control and adjust the treatment plan if needed.
Acute Otitis Media:
- Medications:
- Amoxicillin: 80-90 mg/kg/day divided into two doses for 10 days is recommended for uncomplicated AOM (Danishyar & Ashurst, 2023).
- Patient Education:
- Explain the importance of completing the entire antibiotic course.
- Advise on pain management strategies, such as using acetaminophen or ibuprofen.
- Follow-Up:
- Return in 10-14 days to reassess ear pain and ensure resolution of infection.
Atopic Dermatitis:
- Medications:
- Topical Corticosteroids: Hydrocortisone 2.5% cream applied to affected areas twice daily for flare-ups.
- Emollients: Encourage daily use of emollients like petrolatum-based products to maintain skin hydration.
- Patient Education:
- Educate on the importance of daily moisturizing and avoiding known triggers.
- Discuss the chronic nature of eczema and the importance of long-term management.
- Follow-Up:
- Return in 1 month to evaluate the effectiveness of treatment and make necessary adjustments.
Timothy’s clinical presentation suggests an asthma exacerbation, acute otitis media, and atopic dermatitis as the most likely diagnoses. Comprehensive management, including medication adjustments, patient education, and scheduled follow-ups, is essential to improve Timothy’s health outcomes.