Peer Response- Managing Chronic Kidney Disease (CKD)
Hello,
Great work with your post regarding managing chronic kidney disease (CKD). It provides an excellent background to treat this complex condition, covering diagnostic tests, medications, nonpharmacologic therapies, and referrals. Serum creatinine and eGFR are essential in CKD management because they set the basis for the disease’s stage and the required treatment. Also, the efficiency of the haemoglobin A1c testing is equally crucial because the progression of diabetes and CKD is linked, the latter of which is critical to avoid additional damage to the kidneys.
Following this, other than changes in diet, as you’ve stated, another critical behavior change for patients is smoking cessation, as recommended by the CDC (2024). Tobacco has a direct influence on endothelial function, which further worsens cardiovascular risk factors in patients with CKD. However, supervised exercise training should be incorporated to ensure the patient can exercise and benefit. Subsequently, recent innovations in treatment procedures like MRAs have evidenced the potential to curtail proteinuria and hinder the progression of CKD, as postulated by Baran et al. (2021). These newer therapies, when added to the escalating dose of ACE inhibitors or ARBs, could offer added benefits when it comes to CKD management in patients at higher risk for accelerating disease course.
Besides, the issue of patient education has been considered one of the most critical questions in the treatment process. Schrauben et al. (2022) also note that patients should be educated to adopt appropriate lifestyle changes, adhere strictly to medications, and have frequent follow-ups to reduce CKD progression and improve their quality of life. Therefore, the discussion provides a good background for managing CKD, and these factors can assist in enhancing the patients’ outcomes besides managing CKD.
References
Baran, W., Krzemińska, J., Szlagor, M., Wronka, M., Młynarska, E., Franczyk, B., & Rysz, J. (2021). Mineralocorticoid Receptor Antagonists—Use in Chronic Kidney Disease. International Journal of Molecular Sciences, 22(18), 9995. https://doi.org/10.3390/ijms22189995
CDC. (2024, May 14). Benefits of Quitting Smoking. Smoking and Tobacco Use. https://www.cdc.gov/tobacco/about/benefits-of-quitting.html
Schrauben, S. J., Apple, B. J., & Chang, A. R. (2022). Modifiable Lifestyle Behaviors and Chronic Kidney Disease Progression: A Narrative Review. Kidney360, 3(4), 10.34067/KID.0003122021. https://doi.org/10.34067/kid.0003122021
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
PLEASE WRITE PEER REVIEW ON THE POST BELOW
Diagnosis: Chronic Kidney Disease (CKD)
Peer Response- Managing Chronic Kidney Disease (CKD)
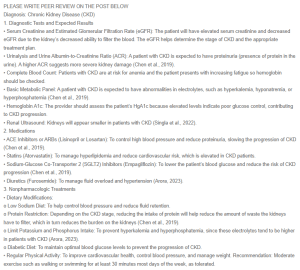
1. Diagnostic Tests and Expected Results
• Serum Creatinine and Estimated Glomerular Filtration Rate (eGFR): The patient will have elevated serum creatinine and decreased eGFR due to the kidney’s decreased ability to filter the blood. The eGFR helps determine the stage of CKD and the appropriate treatment plan.
• Urinalysis and Urine Albumin-to-Creatinine Ratio (ACR): A patient with CKD is expected to have proteinuria (presence of protein in the urine). A higher ACR suggests more severe kidney damage (Chen et al., 2019).
• Complete Blood Count: Patients with CKD are at risk for anemia and the patient presents with increasing fatigue so hemoglobin should be checked.
• Basic Metabolic Panel: A patient with CKD is expected to have abnormalities in electrolytes, such as hyperkalemia, hyponatremia, or hyperphosphatemia (Chen et al., 2019).
• Hemoglobin A1c: The provider should assess the patient’s HgA1c because elevated levels indicate poor glucose control, contributing to CKD progression.
• Renal Ultrasound: Kidneys will appear smaller in patients with CKD (Singla et al., 2022).
2. Medications
• ACE Inhibitors or ARBs (Lisinopril or Losartan): To control high blood pressure and reduce proteinuria, slowing the progression of CKD (Chen et al., 2019).
• Statins (Atorvastatin): To manage hyperlipidemia and reduce cardiovascular risk, which is elevated in CKD patients.
• Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors (Empagliflozin): To lower the patient’s blood glucose and reduce the risk of CKD progression (Chen et al., 2019).
• Diuretics (Furosemide): To manage fluid overload and hypertension (Arora, 2023).
3. Nonpharmacologic Treatments
• Dietary Modifications:
o Low Sodium Diet: To help control blood pressure and reduce fluid retention.
o Protein Restriction: Depending on the CKD stage, reducing the intake of protein will help reduce the amount of waste the kidneys have to filter, which in turn reduces the burden on the kidneys (Chen et al., 2019).
o Limit Potassium and Phosphorus Intake: To prevent hyperkalemia and hyperphosphatemia, since these electrolytes tend to be higher in patients with CKD (Arora, 2023).
o Diabetic Diet: To maintain optimal blood glucose levels to prevent the progression of CKD.
• Regular Physical Activity: To improve cardiovascular health, control blood pressure, and manage weight. Recommendation: Moderate exercise such as walking or swimming for at least 30 minutes most days of the week, as tolerated.
4. Suggested Consults/Referrals
• Nephrologist: To provide specialized care, especially if CKD is stage 3 or higher or if the patient needs to start hemodialysis (Chen et al., 2019).
• Dietitian: To provide guidance on renal-specific dietary modifications, especially in managing protein, potassium, and phosphorus intake. The dietician can also help educate the patient on a diabetic diet to help control blood sugar levels and salt restriction for hypertension.
• Cardiologist: A referral to cardiology may be helpful for this patient who states his blood pressure is uncontrolled SBP 170-180s at home. Effectively controlling hypertension can lower cardiovascular risks and reduce the burden on the kidneys (Arora, 2023).
• Endocrinologist: If the patient’s hemoglobin A1c comes back elevated, a referral to endocrine may be necessary to assist in managing blood glucose levels and reducing the risk of further kidney damage.
5. Client Education
• Educate the patient on CKD, its progression, and the importance of managing underlying conditions like hypertension and diabetes.
• Emphasize the importance of taking medications as prescribed, monitoring for side effects, and attending follow-up appointments with the primary care provider and consults.
• Teach the patient about the importance of dietary modifications, such as reducing sodium, potassium, and phosphorus intake, and adhering to a diabetic diet if applicable (Arora, 2023).
• Monitor for signs of worsening kidney function, such as increased fatigue, swelling, changes in urine output, or shortness of breath, and report these promptly (Arora, 2023).
6. Follow-Up
• Follow-up in 4-6 weeks if eGFR is greater than 30 and albuminuria is less than 300mg/g to reassess kidney function with serum creatinine and eGFR, blood pressure, and symptom progression (Chen et al., 2019).
• Continue regular monitoring of kidney function every 3-6 months, depending on CKD stage, and more frequently if there are concerns about rapid progression or complications.
• Modify medications, reinforce dietary recommendations, and make referrals based on follow-up findings and the patient’s response to treatment. Consider referral to nephrology if eGFR is less than 30 or albuminuria is greater than 300 mg/g (Chen et al., 2019).
References
Arora, P. (2023). Chronic kidney disease. https://emedicine.medscape.com/article/238798-overview
Chen, T. K., Knicely, D. H., & Grams, M. E. (2019). Chronic Kidney Disease Diagnosis and Management: A Review. JAMA : The Journal of the American Medical Association, 322(13), 1294–1304. https://doi.org/10.1001/jama.2019.14745
Singla, R. K., Kadatz, M., Rohling, R., & Nguan, C. (2022). Kidney ultrasound for nephrologists: A review. U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9098467/

