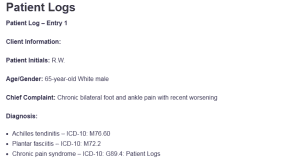
Patient Logs
Patient Log – Entry 1
Client Information:
Patient Initials: R.W.
Age/Gender: 65-year-old White male
Chief Complaint: Chronic bilateral foot and ankle pain with recent worsening
Diagnosis:
- Achilles tendinitis – ICD-10: M76.60
- Plantar fasciitis – ICD-10: M72.2
- Chronic pain syndrome – ICD-10: G89.4: Patient Logs
Procedure:
- Comprehensive foot and ankle musculoskeletal exam
- Palpation of Achilles tendon and plantar fascia
- Gait evaluation and orthotic assessment
- Pain severity scale (1–10)
- Medication reconciliation
Treatment Plan and Notes:
R.W. presented with persistent bilateral foot pain attributed to chronic Achilles tendinitis and plantar fasciitis, flaring up to 9/10 intensity twice weekly. He reported moderate daily pain (3–4/10) and described it as stabbing and achy. The pain is exacerbated by standing or walking and is minimally relieved by the current use of Vicodin. He wears custom orthotics and receives quarterly cortisone injections.
On examination, there was localized tenderness on the medial heel and posterior calcaneus, with tight gastrocnemius and reduced dorsiflexion. Gait was antalgic but stable. Patient education focused on modifying activities and reducing reliance on opioid analgesics. A structured foot stretch program, including wall calf stretches and towel scrunches, was recommended.
NSAIDs were advised post-meal for pain relief, considering GI protection protocols (Ghlichloo & Gerriets, 2023). He was also referred to podiatry for follow-up imaging and a possible orthotic adjustment. The use of cold compresses post-activity and elevation were reinforced for inflammation control (Buchanan & Kushner, 2024). R.W. expressed interest in a PT consult and agreed to begin a home stretching regimen before his next podiatric visit in three weeks.
Patient Log – Entry 2
Client Information:
Patient Initials: R.D.
Age/Gender: 65-year-old White male
Chief Complaint: Right ankle and foot pain; chronic tendinitis and plantar fasciitis
Diagnosis:
- Achilles tendinitis, right lower leg – ICD-10: M76.61
- Plantar fasciitis, right foot – ICD-10: M72.2
- Hematuria (asymptomatic, under urology follow-up) – ICD-10: R31.9
Procedure:
- Focused musculoskeletal exam: palpation of Achilles tendon and plantar fascia
- Pain scale evaluation (current and flare-up ranges)
- Gait and foot alignment assessment
- Review of previous cortisone injection records and urology notes
Treatment Plan and Notes:
R.D. presented with a chronic right Achilles tendinitis and plantar fasciitis, reporting daily pain (3/10) that flares to 8–9/10 twice weekly when walking or standing. The pain is described as stabbing and persistent in the plantar arch and Achilles region. He has been managing with custom orthotics and receives cortisone injections every three months. He takes Vicodin daily, which offers partial relief.
Examination revealed tenderness at the posterior heel and medial plantar fascia, tight gastrocnemius muscles, and limited dorsiflexion. There were no signs of acute swelling. He continues to follow up with urology annually for incidentally discovered kidney and bladder cysts with stable hematuria, first noted in 2022. The patient was counseled on the benefits of physical therapy and instructed to engage in a targeted heel cord stretch regimen, including towel stretches and ankle dorsiflexion exercises (Ahn et al., 2023).
The use of NSAIDs post-meal and daily ice massage for 15–20 minutes post-activity was advised. Opioid use was discussed, and a taper plan may be considered pending response to conservative measures. A follow-up appointment was scheduled in four weeks to assess progress and consider imaging if pain persists.
Patient Log – Entry 3
Client Information:
Patient Initials: S.G.
Age/Gender: 70-year-old White male
Chief Complaint: Follow-up for chronic maxillary sinusitis and post-kidney transplant care
Diagnosis:
- Chronic maxillary sinusitis – ICD-10: J32.0
- Chronic kidney disease stage 4 – ICD-10: N18.4
- Kidney transplant status – ICD-10: Z94.0
- Recurrent urinary tract infections – ICD-10: N39.0
- Eczema – ICD-10: L30.9
Procedure:
- Comprehensive ENT assessment: nasal mucosa inspection, sinus palpation
- Medication reconciliation: Tacrolimus, Flonase
- Review of nephrology and dermatology care plans
- Education on post-transplant infection risk
Treatment Plan and Notes:
S.G., a retired veteran (service 1976–1980), presented for chronic sinusitis follow-up. He experiences flare-ups four times per year with symptoms of nasal congestion, frontal headache, facial pressure, and purulent drainage, especially post-shaving. He denied fever, facial swelling, or shortness of breath. A physical exam showed mild tenderness over the maxillary sinuses and mucosal congestion.
Notably, he had a left-sided kidney transplant in March 2022 due to a congenital single kidney and CKD4. His last UTI occurred in November 2024, and he is followed by both a nephrologist and a dermatologist. Immunosuppressive therapy with tacrolimus continues. Given his transplant status, he was counseled on strict infection prevention, including saline nasal irrigation, humidification, and daily Flonase use (Pinchera et al., 2024).
Due to his immunocompromised state, antibiotics were deferred unless purulent drainage worsens or fever develops. Coordination with ENT was initiated for imaging if flare-ups increase. Dermatologic management of eczema continues per prior recommendations.
The patient was educated on signs of serious infection and emphasized the importance of hydration, hygiene, and follow-up. He understood and agreed to all recommendations and will follow up in one month or sooner if symptoms worsen.
Patient Log – Entry 4
Client Information:
Patient Initials: M.K.
Age/Gender: 35-year-old White male
Chief Complaint: Routine follow-up for hypertension
Diagnosis:
- Essential (primary) hypertension – ICD-10: I10
- Hyperlipidemia, unspecified – ICD-10: E78.5
Procedure:
- Blood pressure measurement (sitting and standing)
- Cardiovascular risk assessment (ROS, family history, medication adherence)
- Lipid profile review and medication reconciliation (losartan, atorvastatin)
- Lifestyle evaluation: diet, physical activity, stress
Treatment Plan and Notes:
M.K. presented for a scheduled follow-up to monitor well-controlled hypertension. He is currently on losartan and atorvastatin, with no reported side effects or changes in adherence. No family history of cardiovascular disease was noted, and he has remained asymptomatic. Vital signs were stable, with a blood pressure of 122/78 mmHg.
The patient denied chest pain, dizziness, headaches, or visual changes. The physical exam was unremarkable. Lab work from the previous visit showed stable lipid levels and normal renal function. He was encouraged to continue a DASH-style diet, maintain regular aerobic exercise (at least 150 minutes weekly), and reduce sodium intake (Mulla & Siddiqui, 2022).
Education was provided on recognizing early signs of elevated blood pressure and the importance of medication compliance. A follow-up lipid panel was ordered for 6 months, and a routine physical exam was scheduled annually. The patient verbalized understanding and showed good insight into long-term cardiovascular risk prevention strategies.
Patient Log – Entry 5
Client Information:
Patient Initials: L.J.
Age/Gender: 40-year-old White male
Chief Complaint: Bilateral knee pain—left since 2003, right since 2014
Diagnosis:
- Chronic pain of bilateral knees – ICD-10: M25.561
- Patellofemoral pain syndrome – ICD-10: M22.40
- Joint pain, unspecified – ICD-10: M25.50
Procedure:
- Bilateral knee exam: palpation, ROM, joint line tenderness
- Gait analysis
- Pain scale and flare frequency assessment
- Medication review (Tylenol, ibuprofen)
Treatment Plan and Notes:
L.J. reported long-standing bilateral knee pain, initially affecting the left knee (2003) and later the right (2014). Pain is described as daily (5/10) with sharp, popping sensations and flares to 8/10 twice weekly during flexion or prolonged activity. He denied trauma or recent exacerbation. A physical exam revealed crepitus and mild patellar tenderness bilaterally, with no joint effusion.
Ligament stability tests were negative. Gait was guarded with mild valgus alignment. Current OTC management includes Tylenol and ibuprofen. He was counseled on the benefits of low-impact exercises like swimming and cycling and referred to physical therapy for quadriceps strengthening and patellar tracking correction (Hsu & Siwiec, 2023).
The use of ice packs after exertion and joint offloading through weight management was emphasized. The patient was advised to avoid deep squats and high-impact sports. Referral to orthopedics for imaging was offered, but the patient opted to try PT first. A recheck in six weeks was scheduled to evaluate symptom progression.
Patient Log – Entry 6
Client Information:
Patient Initials: C.F.
Age/Gender: 76-year-old White male
Chief Complaint: Chronic pain in back and bilateral knees; follow-up after prior ACL repair
Diagnosis:
- Chronic back pain – ICD-10: M54.5
- Chronic bilateral knee pain – ICD-10: M25.561
- History of left ACL repair – ICD-10: Z98.890
- Chronic pain syndrome – ICD-10: G89.4
Procedure:
- Full musculoskeletal evaluation of back and knees
- Pain scale documentation (baseline and flare-ups)
- Functional mobility assessment (sitting, standing, climbing)
- Education on conservative pain management strategies
Treatment Plan and Notes:
C.F., a retired marine and former nurse, presented with chronic dull and sharp pain in the back and both knees. The pain, which began around 2010 due to physical labor, is daily and rated 5/10, flaring to 9–10/10 during activity or prolonged standing. He has a history of ACL repair in 1997 but denies any recent injury, use of braces, injections, or physical therapy. On examination, he exhibited reduced lumbar flexion, bilateral knee joint line tenderness, and stiffness. No swelling, radiculopathy, or neurological deficits were noted.
He denied bowel/bladder issues and showed no signs of instability. Given his reluctance to use medications or therapy in the past, he was counseled on initiating a structured home exercise program focused on stretching and joint preservation (Farley et al., 2024). Recommendations included hot packs for morning stiffness, ice after activity, and lateral sleep positioning.
The patient was advised to avoid ladders and hiking due to increased fall risk. Referral to PT and pain management was offered. He agreed to attempt a trial of home-based interventions and monitor progress. A reassessment in four weeks was scheduled.
Patient Log – Entry 7
Client Information:
Patient Initials: K.A.
Age/Gender: 24-year-old Black female
Chief Complaint: Follow-up after hospitalization for chest pain; discharged AMA
Diagnosis:
- Reactive airway disease – ICD-10: J45.998
- History of chest pain, unspecified – ICD-10: R07.9
- Allergic rhinitis – ICD-10: J30.9
Procedure:
- Respiratory system examination: auscultation for wheezing, respiratory rate
- Medication reconciliation: Flonase, Montelukast, nebulizer, inhaler
- Hospital discharge AMA documentation review
- Echocardiogram results interpretation
Treatment Plan and Notes:
K.A. presented for outpatient follow-up after a recent hospital admission for chest pain. She had left against medical advice (AMA) on May 28 and was scheduled to see a cardiologist at the end of June. The patient denied current chest pain or shortness of breath but reported mild congestion and expiratory wheezing. Vital signs were stable; a lung exam revealed scattered wheezes without crackles.
A review of her hospital echocardiogram showed no structural abnormalities. The current regimen includes daily Flonase and Montelukast, along with an as-needed nebulizer and inhaler. Education focused on asthma trigger avoidance, medication adherence, and early use of bronchodilators during symptom onset (Reuter et al., 2024).
She was encouraged to keep her cardiology appointment and avoid strenuous activity until cardiac clearance. Emphasis was placed on the importance of completing all patient procedures and the problems that could occur if these were cut short. The patient noted that she understood and decided to stick with the recommended treatment and additional check-ups.
Patient Log – Entry 8
Client Information:
Patient Initials: F.B.
Age/Gender: 75-year-old White male
Chief Complaint: Evaluation for chronic foot pain related to flatfoot and lower extremity edema
Diagnosis:
- Acquired flatfoot deformity – ICD-10: M21.42
- Bilateral lower extremity edema – ICD-10: R60.0
- Gait abnormality – ICD-10: R26.9
Procedure:
- Musculoskeletal foot exam: arch integrity, pain localization, gait assessment
- Evaluation of edema grade and response to compression therapy
- Functional mobility test (ambulation, stairs)
- Review of past podiatry history and orthotic device usage
Treatment Plan and Notes:
F.B. presented with chronic foot pain attributed to flatfoot and significant bilateral lower extremity edema. He uses a scooter and walker for ambulation and wears compression socks daily. He reported 5/10 baseline foot pain, described as aching, with flares up to 7/10 during prolonged sitting or walking. Physical exam showed 3+ BLE edema and collapsed medial longitudinal arches.
He reported that he had not undergone any foot surgery, and there was no recent trauma. More than a decade had gone by since F.B. had last visited a podiatrist, and he was unsure about the best methods for dealing with his foot pain now. Special arch-supportive orthotics were recommended for his flatfoot condition, and it was advised to reduce shoes worn for long periods. Edema was managed through compression therapy, and treatments also included raising the legs and avoiding a high intake of salt (Jacob et al., 2023).
The decision was made to create custom orthotics and repeat radiograph examinations. The patient was advised about the possibility of skin breakdown due to inactivity and edema. He planned to start with gentle therapies and return after 4–6 weeks to determine if any further treatment was necessary.
References
Ahn, J., Yeo, J., Lee, S., Lee, Y. J., Park, Y., Goo, B., & Ha, I. (2023). Healthcare usage and cost for plantar fasciitis: A retrospective observational analysis of the 2010–2018 health insurance review and assessment service national patient sample data. BMC Health Services Research, 23(1). https://doi.org/10.1186/s12913-023-09443-2
Buchanan, B. K., & Kushner, D. (2024). Plantar fasciitis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431073/
Farley, T., Stokke, J., Goyal, K., & DeMicco, R. (2024). Chronic low back pain: History, symptoms, pain mechanisms, and treatment. Life, 14(7), 812. https://doi.org/10.3390/life14070812
Ghlichloo, I., & Gerriets, V. (2023, May 1). Nonsteroidal anti-inflammatory drugs (NSAIDs). PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547742/
Hsu, H., & Siwiec, R. M. (2023, June 26). Knee osteoarthritis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507884/
Jacob, J., Liow, Y., & Teo, D. B. (2023). Approach to bilateral lower limb oedema. Singapore Medical Journal, 64(7), 444. https://doi.org/10.4103/singaporemedj.smj-2021-142
Mulla, S., & Siddiqui, W. J. (2022). Losartan. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526065/
Pinchera, B., Trucillo, E., D’Agostino, A., & Gentile, I. (2024). Urinary tract infections in kidney transplant patients: An open challenge—Update on epidemiology, risk factors and management. Microorganisms, 12(11), 2217. https://doi.org/10.3390/microorganisms12112217
Reuter, Q., Lesh, N., Reyes, M., Gothard, D., Pallaci, M., & Weinstock, M. (2024). Rapid outpatient evaluation for emergency department patients with intermediate risk chest pain safely reduces admissions. Journal of the American College of Emergency Physicians Open, 5(5). https://doi.org/10.1002/emp2.13280
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Patient Log
Throughout this course, you will also keep a log of patient encounters using Meditrek. AGPCNP students must record at least 100 encounters with GYN patients; FNP students must record at least 125 encounters with patients (100 GYN and 25 OB patients) by the end of this practicum.
The patient log must include the following:
- Client Information
- Diagnosis
- Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
- Treatment Plan and Notes
Includes
1). Diagnosis
2). Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
3). Treatment Plan and Notes
Scenario 1
65 years old white meal
- 65 white male
- Marines 71-73
- History of carcinoma to left arm (scar measures 5 cm), left lateral thigh (6 cm scar), and low back (3 cm scar). Removed 2015
- Follows up with provider annually
Scenario 2
65 white male
- Kidney and bladder cysts – incidentally found in 2022 during a ct for another issue
- Hematuria
- Annual urology follow up
- Right ankle Achilles tendinitis since 1981 4/10 daily tender pain
- Flares 2 days a week to 8/10 when staying, walking, or when he rolls it
- Takes daily vicoden for pain
- Right foot plantar fascitis since 2024
- Cortisone shots q 3 months
- Daily 3/10 stabbing pain Flares to 9/10, 2 days a week with standing and walking
- Custom orthotics help
Scenario 3
S.G 70 years old male, retired, service 1976-1980
- f/u Issue with maxillary frontal sinusitis, s.s includes nasal congestion, headache, pressure, discomfort, tighten around sinus, purulent drainage, flare up 4 times a year, flare up after shaving.
- PHM: kidney transplant left side 03/19/2022, born with 1 kidney congenital, CKD4, recurrent UTI, last UTI 11/2024, sinusitis, Eczema
- Follow by Nephrologist, Dermatologist
- Denies dialysis treatment
- Medications: Tacrolimus po BID, Flonase spray daily
Scenario 4
35 white male
- Hypertension
- Takes losartan and atorvastatin
- No family history
- Managed by pop
Patient Logs
Scenario 5
40 white male
- Bilateral knee pain
- Left knee began in 2003
- Right knee in 2014
- From day to day activities
- Daily 5/10 popping, stabbing pain in knee cap
- Flares twice a week lasting 30 to 120 minutes, 8/10 pain increased with flexion
- Takes Tylenol and ibuprofen
Scenario 6
C.F 76 YEARS OLD WHITE MALE
- Follow up with back, bilateral knees pain
- PMH: Chronic pain on bilateral knees, back, neck, bilateral hip, Repaired left ACL ligament 1997
- Issues started from 2010 from daily activities
- Occupation: Nurse, retired marine from 1988-2017
- X-ray done on back 2012
- Denies injuries on back and knee.
- Denies physical therapy, chiropractor, medications
- Daily constant pain back, bilateral knees
- Rated pain 5/10, describes as dull achiness on back pain, pain can go up to 9/10, lasting 12 hrs a day
- Rated pain 5/10, describe as sharp shooting pain bilateral knees, pain can go up to 9-10/10, lasting 12 hrs a day
- Flare up 1-2 times a week, lasting 12 hrs a day related to activity
- Denies numbness/tinglings, incontinent of bladder and bowel movement
- Denies back brace, or knee braces
- Denies cortisone injection on left knee
- Pain aggravated by prolonged standing, supine
- Pain alleviated with rest, stretching, lateral position
- Unable to climb up ladder, can no longer hike anymore
Scenario 7
K.A 24 years old female black
- Follow up visit from hospital chest pain
- s/s congestion, expiratory wheezing
- Denies SOB, chest pain
- Discharged from hospital AMA 5/28
- Upcoming follow up Appointment with Cardiologist the end of this month june
- Had echocardiogram done at hospital, result no abnormal finding
- Continue to use flonase daily, montelukast daily, and nebulizer and inhaler as needed.
Scenario 8
F B 75 years old white male
- Eval for flat foot pain
- No history of surgery or procedure on foot
- 3+ edema BLEs, have compression socks on
- Have orthotic shoe not specially for flat foot, but for BLEs edema
- Rated pain 5/10, describes as achiness, flare up daily, pain can go up to 6-7/10
- Pain aggravated by prolonged sitting and walking
- Pain alleviated by stretching
- Unable to do stair
- Use scooter and walker for ambulation
- Last saw podiatrist 10 years ago
- Not sure what he take for foot pain