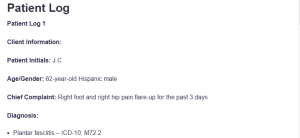
Patient Log
Patient Log 1
Client Information:
Patient Initials: J.C
Age/Gender: 62-year-old Hispanic male
Chief Complaint: Right foot and right hip pain flare-up for the past 3 days
Diagnosis:
- Plantar fasciitis – ICD-10: M72.2
- Right hip osteoarthritis – ICD-10: M16.11
- Chronic bilateral knee pain – ICD-10: M25.561: Patient Log
Procedure:
- Comprehensive musculoskeletal assessment
- Gait observation using a cane
- Pain scale evaluation (1–10)
- Imaging review (hip MRI and foot X-ray)
Treatment Plan and Notes:
J.C. experienced acute-on-chronic musculoskeletal pain that limited his range of motion and affected his daily activities. The pain was stabbing and sharp, worsened by walking, and relieved with meloxicam and ibuprofen. Despite using a cane and orthotic inserts, the patient had an antalgic gait, and there was marked impairment in standing up from sitting.
A complete musculoskeletal exam revealed focal tenderness along the plantar fascia and limited right hip flexion, which was in keeping with progressive osteoarthritis. Although he had previously declined physical therapy, he was once again counseled on its proven benefits of reducing inflammation and improving joint function, in this case, through specific stretching and muscle strengthening (El-Tallawy et al., 2021).
He was requested to initiate treatment in one week, and a written referral was issued. He was also advised to limit excessive standing, use cushioned footwear, and perform daily ankle rolls and seated stretches. A modified plan was made for pain assessment on a 1–10 scale, and guidance was provided on switching NSAIDs with meals to minimize GI risk.
A re-evaluation in four weeks is scheduled to monitor therapy compliance, gait status, and pain relief. According to conservative pain management guidelines, he was also instructed to perform frequent foot elevation and cold compresses to reduce localized inflammation and pain (Buchanan & Kushner, 2024). The patient indicated understanding of all instructions and agreed to implement the recommended modifications.
Patient Log 2
Client Information:
Patient Initials: F.R
Age/Gender: 65-year-old White male
Chief Complaint: Increased fatigue, insomnia, and social withdrawal
Diagnosis:
- Mild cognitive impairment – ICD-10: G31.84
- Major depressive disorder, single episode, moderate – ICD-10: F32.1
Procedure:
- Mini-Mental State Examination (MMSE)
- Depression screening using PHQ-9
- Neurological assessment
- Medication review (Donepezil 10 mg PO daily)
Treatment Plan and Notes:
F.R. is a retired mail worker and veteran with symptoms of low motivation, impaired sleep, and minimal interest in activities that he previously enjoyed. The MMSE score was compatible with mild cognitive impairment, which was consistent with the prior diagnosis of dementia. A PHQ-9 score of 16 confirmed moderate depression.
The patient is continued on donepezil 10 mg PO qd for cognitive function. As emotional distress and functional impairment increased, sertraline 25 mg PO qd was ordered, with plans to titrate in two weeks if tolerable. The patient and caregiver were instructed about the potential side effects of GI upset, drowsiness, and mood alteration. Educational materials were provided to augment medication adherence, regular monitoring, and daily wellness checklists.
By person-centered principles of care, the carer was advised to implement a daily routine, promote gentle exercise, and introduce calming pre-bedtime routines to improve sleep quality. Referral was made to a local cognitive wellness group to promote peer support and reduce social isolation. Bains and Abdijadid (2023) assert that early dual-approach management of depression and dementia improves emotional well-being and reduces further cognitive decline.
In addition, the patient was also instructed in ambulation safety, such as clear pathways on the floor, stairway handrails, and outdoor walking restricted to mornings only. Plans were also made to reassess medication efficacy and mood on a two-week follow-up visit. F.R. appreciated the additional support and was encouraged to maintain a medication and mood diary to report on his next visit.
Other issues covered included long-term care planning and the role of the durable power of attorney in the event of future cognitive decline, with a recommendation for advanced decision-making (Livingston et al., 2020). The caregiver was also invited to attend a forthcoming dementia caregiver education class being presented at the clinic.
References
Bains, N., & Abdijadid, S. (2023). Major depressive disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559078/
Buchanan, B. K., & Kushner, D. (2024). Plantar fasciitis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431073/
El-Tallawy, S. N., Nalamasu, R., Salem, G. I., LeQuang, J. A. K., Pergolizzi, J. V., & Christo, P. J. (2021). Management of musculoskeletal pain: An update with emphasis on chronic musculoskeletal pain. Pain and Therapy, 10(1), 181–209. https://doi.org/10.1007/s40122-021-00235-2
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., & Orgeta, V. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Throughout this course, you will also keep a log of patient encounters using Meditrek. AGPCNP students must record at least 100 encounters with GYN patients; FNP students must record at least 125 encounters with patients (100 GYN and 25 OB patients) by the end of this practicum.
The patient log must include the following:
- Client Information
- Diagnosis
- Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
- Treatment Plan and Notes
SCENERIO 1
J.C Hispanic Latino 62 years old male
- Chief complaint: right foot pain, right hip pain flare up occur 3 days
- From knee condition issues
- Past medical hx: plantar fasciitis, right hip pain, knees pain
- HaS issue over 4-5 years approximately from 2020
- No past medical history of procedure, surgery on right hip, right foot
- Had orthotic shoe & insert for right foot from VA
- X-ray, MRI done on hip
- Pain occur daily, rated 5/10 describes as shooting pain
- Pain can go up to 10/10 lasting 10 mins, alleviated by meloxicam
- Pain aggravated by prolonged sitting and standing
- Pain alleviated by ibuprofen, and meloxicam
- Use cane
- Denies physical therapy
Patient Log
SCENERIO 2
F.R 65 years old white male
- Present with increased fatigue, difficulty getting out of bed, insomnia, stop socializing with friends
- PHM: recently diagnosed with Dementia in 2022, mild cognitive impairment impacted short term and long term memory
- Social: Retired VA served in 1977-1980, Used to work at post office custodial
- Done CT, MRI of brain
- No history of surgery or procedure of the brain
- Donepezil 10mg po daily
- Use cane and walker regularly for ambulation
Includes
1). Diagnosis
2). Procedure (Note: Make sure that, as you perform procedures at your practicum site, you also note those on your printed-out Clinical Skills List.)
3). Treatment Plan and Notes