NUR 4590 – Deliverable 3 – Quality Improvement Process
In today’s hospital world, when there is an employee survey, nurses can say that they will not do it because nothing will change, and it is a waste of time. At the management level, they can change a lot unless they know what to change. There are many healthcare systems, and they are very competitive.
Do you need help with your assignment? Get in touch with us.
Quality improvement is not only looking at patient safety and satisfaction, but it also looks at a budget and how this budget needs to be controlled. When patients are falling and getting injuries, then a patient needs to stay longer in the hospital. The insurance company will not pay for the stay because it is the healthcare agency’s fault that the patient was not watched correctly during the stay. Staff members do not want to report near misses, such as patient complaints that a floor is slippery or no safety rails in the bathroom. Nevertheless, on the other hand, nothing happened, so why inconvenience? Should we take the time to create a safety event and report it as a near-miss?
Many government agencies, such as the Joint Commission, established sentinel events alerts. One of them is an alert to prevent falls and fall-related injuries in healthcare facilities. The near misses or something that the nurse may notice and not report may create falls and fall-related injuries. Many organizations have created a system for employees to report near misses or falls without or with injuries. The risk management analyzes those reports. Data are created, and consequences are drowned. It creates a model to teach and prevent future occurrences (Achanta, 2017). Quality improvement ensures that data is correctly collected and kept in the registration database and meets the required quality standards, which are usually specified based on the intended uses. For example, the fall prevention data collection goal was to provide hospitals with valuable, practical information about the falls themselves and the situation and reduce their occurrence.
NUR 4590 – Deliverable 3 – Quality Improvement Process
Patient safety is the most important. The outcome of the fall can ruin a patient’s life or even be fatal to the patient. According to the research done by the Joint Commission, a common cause of patient falls is a preliminary assessment, communication failures, lack of adherence to protocols and safety practices, inadequate staff orientation, supervision, employment levels, and lack of leadership. There are multiple types of research done in order to prevent falls from occurring. However, one of the reliable research and essays done by the Joint Commission can be a great source to prevent patients from falling. They are as follows: Lead an effort to raise awareness of the need to prevent falls resulting in injury. Establish an interdisciplinary falls injury prevention team or evaluate the membership of the team in place to ensure organizational infrastructure and capacity to reduce injury risk from falls (Rajagopalan et al., 2017).
In all of the model’s categories, such as structure, procedure, and outcome, some indications that apply to healthcare safety may be measured. For example, a structured hospital must have a policy or mechanism for reporting falls or events related to falls. Reporting is an important indicator that affects the hospital environment or structure. If such events or situations are unreported, they have several negative consequences for the facility. An assessment cannot determine the causes of the fall and how it can be addressed if it is not disclosed.
Numerous medical safety indicators are part of the hospital care delivery process. During an admission, patient and family members’ interviews are crucial to determine fall risk. All the medications need to be checked if they can cause dizziness. Rooms and hallways need to be without the clatter and with enough light. The patient needs to be altered and informed not to get up from the bed without help if he feels comfortable getting up alone. The hospital can have a virtual sister service, which is also programmed with multiple languages, so there is no need for a translator for simple comments. It prevents multiple calls in order to get a translator or call one and use a translator service. (Shekelle et al., 2019). The staff is highly satisfied because when the bed alarm was on, the patient was already on the floor with a Virtual sitter service; this can be prevented; it is an extra set of eyes. Virtual Sitter Service also reduces falls and falls-related injuries per a pilot study done by Mission Hospital in Asheville, North Carolina, a 23% reduction in falls and a 12% reduction in fall-related injuries over a 1-year (Cuttler et al.,2017). The immediate impact on the community is enormous patient satisfaction, especially family members who know that their loved ones are in great hands and understand that, for example, the sitter is not sleeping on the job by the patient site because technology is watching this patient.
NUR 4590 – Deliverable 3 – Quality Improvement Process
The outcome can be measured when there are fewer fall reports. This metric measures the frequency of fall events and injuries related to them. Quality health services deliver the proper care at the proper time. It is essential to explain to staff that reporting the events is not a complaint. It is making sure patient safety is number one and quality of care is improved.
To minimize any falls with injuries or without, it is essential to report any suspicious activities. Nurses’ schedules can be made so that they can handle the patient load. The patient needs to be monitored by a virtual sitter if one on one care is not possible. Use a standardized, validated tool to identify fall risk factors (e.g., Morse Fall Scale17-20 or Hendrich II Fall Risk Model21-24), first integrated into the electronic medical record. Progress a customized plan of care based on identified fall and injury risks, and implement interventions specific to a client, population, or setting. Regulate and apply practices and interventions established to be effective, including a consistent hand-off communication process for recognizing patient risk for falls with injury. It is crucial to recognize specific areas of risk and patient-specific interventions to mitigate the risk. One-to-one education of each client at the bedside by trained health professionals using educational materials covering fall risk and causes and preventive strategies. Check post-fall management, which includes a post-fall huddle; a system of honest, transparent reporting; trending and analysis of falls, which can inform improvement efforts; and reassess the patient (Sentinel event alert, 2015).
References
Achanta, G. (2017, March). Optimizing the Use of an Electronic Fall Prevention Toolkit To Prevent Falls in Hospitalized Patients | Agency for Healthcare Research and Quality. Www.ahrq.gov. https://www.ahrq.gov/chain/research-tools/featured-certs/electronic-fall-prevention-toolkit.html
Cuttler, S. J., Barr-Walker, J., & Cuttler, L. (2017). Reducing medical-surgical inpatient falls and injuries with videos, icons and alarms. BMJ Open Quality, 6(2), e000119. https://doi.org/10.1136/bmjoq- 2017-000119
Rajagopalan, R., Litvan, I., & Jung, T.-P. (2017). Fall Prediction and Prevention Systems: Recent Trends, Challenges, and Future Research Directions. Sensors, 17(11), 2509. https://doi.org/10.3390/s17112509
Sentinel event alert. (2015, September 28). Preventing falls and fall-related injuries in health care facilities. The Joint Commission. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_55_falls_4_26_16.pdf
Shekelle, P. G., Greeley, A. M., Tanner, E. P., Mak, S. S., Begashaw, M. M., Miake-Lye, I. M., & Beroes- Severin, J. M. (2019). One-to-One Observation: A Systematic Review. In PubMed. Department of Veterans Affairs (US). https://pubmed.ncbi.nlm.nih.gov/32065739/
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
NUR 4590 – Deliverable 3 – Quality Improvement Process
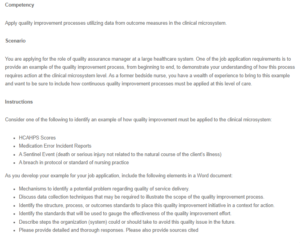
Competency
Apply quality improvement processes utilizing data from outcome measures in the clinical microsystem.
NUR 4590 – Deliverable 3 – Quality Improvement Process
Scenario
You are applying for the role of quality assurance manager at a large healthcare system. One of the job application requirements is to provide an example of the quality improvement process, from beginning to end, to demonstrate your understanding of how this process requires action at the clinical microsystem level. As a former bedside nurse, you have a wealth of experience to bring to this example and want to be sure to include how continuous quality improvement processes must be applied at this level of care.
Instructions
Consider one of the following to identify an example of how quality improvement must be applied to the clinical microsystem:
- HCAHPS Scores
- Medication Error Incident Reports
- A Sentinel Event (death or serious injury not related to the natural course of the client’s illness)
- A breach in protocol or standard of nursing practice
As you develop your example for your job application, include the following elements in a Word document:
- Mechanisms to identify a potential problem regarding quality of service delivery.
- Discuss data collection techniques that may be required to illustrate the scope of the quality improvement process.
- Identify the structure, process, or outcomes standards to place this quality improvement initiative in a context for action.
- Identify the standards that will be used to gauge the effectiveness of the quality improvement effort.
- Describe steps the organization (system) could or should take to avoid this quality issue in the future.
- Please provide detailed and thorough responses. Please also provide sources cited

