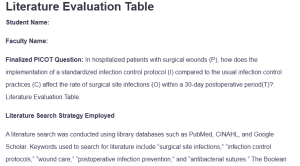
Literature Evaluation Table
Student Name:
Faculty Name:
Finalized PICOT Question: In hospitalized patients with surgical wounds (P), how does the implementation of a standardized infection control protocol (I) compared to the usual infection control practices (C) affect the rate of surgical site infections (O) within a 30-day postoperative period(T)?: Literature Evaluation Table.
Literature Search Strategy Employed
A literature search was conducted using library databases such as PubMed, CINAHL, and Google Scholar. Keywords used to search for literature include “surgical site infections,” “infection control protocols,” “wound care,” “postoperative infection prevention,” and “antibacterial sutures.” The Boolean operator was used to combine the search terms in order to limit or expand the search results.
Also, filters were applied to select peer-reviewed articles within the last five years to ensure the research was current and relevant. Finally, “randomized controlled trial” and “meta-analysis” were included to find only the highest-quality studies.
| Criteria | Article 1 | Article 2 | Article 3 | Article 4 |
| APA Reference
All peer-reviewed journal articles should be current (published within the last 5 years) and closely related to the PICOT question developed earlier in this course. Include the GCU permalink, or working link used to access the article. |
Anderson, D. J., Ilieş, I., Foy, K., Nehls, N., Benneyan, J. C., Lokhnygina, Y., & Baker, A. W. (2020). Early recognition and response to increases in surgical site infections using optimized statistical process control charts—the early 2RIS Trial: A multicenter cluster randomized controlled trial with stepped wedge design. Trials, 21(1). https://doi.org/10.1186/s13063-020-04802-4 | De Simone, B., Sartelli, M., Coccolini, F., Ball, C. G., Brambillasca, P., Chiarugi, M., Campanile, F. C., Nita, G., Corbella, D., Leppaniemi, A., Boschini, E., Moore, E. E., Biffl, W., Peitzmann, A., Kluger, Y., Sugrue, M., Fraga, G., Di Saverio, S., Weber, D., . . . Catena, F. (2020). Intraoperative surgical site infection control and prevention: a position paper and future addendum to WSES intra-abdominal infections guidelines. World Journal of Emergency Surgery, 15(1). https://doi.org/10.1186/s13017-020-0288-4 | Li, X., Lin, H., Zhu, L., Chen, J., Lei, S., Li, B., & Su, S. (2022). The clinical effectiveness of wound edge protectors in reducing surgical site infection after abdominal surgery: Meta-analysis. BJS Open, 6(3). https://doi.org/10.1093/bjsopen/zrac065 | Matz, D., Engelhardt, S., Wiencierz, A., Soysal, S. D., Misteli, H., Kirchhoff, P., & Heizmann, O. (2024). Do antibacterial skin sutures reduce surgical site infections after elective open abdominal surgery?—A prospective, randomized controlled single-center trial. Journal of Clinical Medicine, 13(22), 6803. https://doi.org/10.3390/jcm13226803 |
| Purpose/Aim of Study | This study was designed to assess the effectiveness of SPC charts in detecting trends in SSIs and thus enabling timely interventions. Anderson et al. (2020) hypothesized that using SPC charts would provide surgical teams with dynamic monitoring of infection rates and prompt them to respond quickly to deviations, hence reducing SSI rates. | This study updates recommendations for intraoperative SSI strategies in abdominal surgery and strives to provide evidence-based practice guidelines where current gaps have been identified. The goal is to reduce SSI rates to improve surgical outcomes. | This study aimed to assess the efficiency of wound-edge protectors in preventing SSIs after abdominal surgeries. It also sought to determine the part physical barriers played in the prevention of infection in the post-surgical period, particularly in high-risk surgery. | This study sought to establish the extent of the use of antibiotic-bonded skin sutures in the prevention of SSIs in patients operated through elective open abdomen surgery. The objective was to find out if an opportunity exists for antimicrobial sutures to reduce postoperative infection incidence that regular sutures present (Matz et al., 2024). |
| Research questions (Qualitative)/Hypothesis (Quantitative) | The hypothesis with regard to SPC charts was that these would augment the ability to identify a rising pattern of SSIs much more promptly than the present means of monitoring, allowing intervention linked with cuts identifiable in infection rates. | The important question for the study stated, “Which intraoperative interventions will best prevent SSIs in abdominal surgery?” The hypothesis was that intraoperative adherence to antiseptic policies and sterility would greatly reduce infection rates (De Simone et al., 2020). | The research question was: “Do wound-edge protectors reduce the incidence of surgical site infections after abdominal surgeries?” It was hypothesized that wound-edge protectors would significantly reduce SSIs by preventing bacterial contamination at the surgical site (Li et al., 2022). | The research question was: “Do antibacterial sutures significantly reduce the risk of SSIs after elective open abdominal surgery?” The hypothesis tested was that fewer SSIs would develop in patients receiving antibacterial sutures than those receiving conventional sutures. |
| Design
Type of quantitative or type of qualitative study design |
This is a quantitative, multicenter cluster randomized controlled trial. A stepped-wedge design allows for sequential implementation across sites to evaluate the effect of the intervention. | This was qualitative position research aimed at synthesizing findings from existing literature and expert consensus. The study’s design included a comprehensive review and thematic analysis of previous research and clinical guidelines. | Quantitative study; meta-analysis of RCTs | Quantitative study; prospective randomized controlled trial |
| Setting
Where did the study take place? What type of setting – inpatient, outpatient, etc.? |
The trial was conducted in several inpatient surgical units in various healthcare institutions to ensure patient population diversity and clinical practices. | The recommendations apply broadly to inpatient and outpatient surgical settings, emphasizing intra-abdominal procedures. | The sample consisted of a mix of surgical settings, mostly inpatient hospitals performing abdominal surgeries. | It was performed in a single inpatient surgical center specialized for elective abdominal surgery. |
| Sample
Number and characteristics of participants |
The sample population for this study included patients who had undergone surgery in participating centers. While specific demographics for participants were not identified, this multihospital approach allowed a wide range of patients and surgical cases. | The study did not include primary data collection but reviewed literature and guidelines that included diverse patient populations and surgical settings. | The pooled data analyzed 20 RCTs of several thousand patients undergoing scheduled abdominal surgeries; the series of patients consisted of a varied age group with different comorbidities to ensure heterogeneity (Li et al., 2022). | The study randomized 200 patients undergoing elective open abdominal surgeries. The participants included male and female patients, ranging in age from 18 to 75 years, with varying degrees of health risk (Matz et al., 2024). |
| Methods
Interventions/Instruments |
SPC charts were introduced to monitor and analyze SSI trends in real time. Surgical teams were alerted to institute targeted infection control measures when infection rates exceeded predefined thresholds. Continuous data collection was done through pre- and post-intervention phases. | Data from multiple trials, which investigated antiseptic wound irrigation, double gloving, intraoperative glove changes, and disposable material use, were pooled. Recommendations were given based on evidence ranking regarding intervention effectiveness (De Simone et al., 2020). | Infection rates were compared with and without the use of wound-edge protectors. The meta-analysis combined data from multiple studies to assess the overall effectiveness of the intervention. | Patients were randomly assigned to either antibacterial sutures for skin closure or a standard suture for the same. Infection rates were followed up after the surgery for up to 30 days. |
| Analysis
How was the data collected and analyzed? |
The analysis employed statistical modeling to estimate the SSI rates before and after the intervention periods while comparing trends across several participating centers. It evaluated the timeliness and overall effect of the SSI reduction intervention. | Thematic synthesis and comparative analysis of the reviewed studies identified the most effective intraoperative measures. De Simone et al. (2020) then critiqued gaps in adherence to sterility protocols and emphasized strategies for improvement. | Statistical analysis included calculating pooled risk ratios using information with an assessment of heterogeneity and using standard meta-analytical techniques to determine if this wound-edge protector had a statistically significant association with SSI reduction (Li et al., 2022). | A statistical analysis was performed to compare the infection rates between the two groups. The primary outcome measure was the development of SSIs, while secondary outcome measures included additional interventions or extended hospitalization. |
| Outcomes/key findings of the study and implications for nursing practice (Summary of study results) | The SPC charts helped in the early identification of pattern changes within infection rates much better than before to allow timely interventions by the healthcare teams. This aggressive strategy significantly decreased the overall SSI incidence in all the centers engaged in the study (Anderson et al., 2020). | Concerning the findings, antiseptic irrigation was underlined as critical to reducing SSIs, frequent glove changes, and the application of disposable drapes. Notably, differences in compliance with these measures between surgical centers threaten the regular occurrence of such results. | The review revealed that the prevention of SSIs was achieved by 50% using wound-edge protectors, mainly in high-risk abdominal operations. Also, the intervention was inexpensive and easy to incorporate into the basic teaching-learning procedures (Li et al., 2022). | The data agree with the hypothesis that antibacterial sutures are safer than conventional sutures in the prevention of postoperative infections since they reduce the incidences of SSIS. |
| Recommendations of the Researcher | Anderson et al. (2020) advised improving the existing infection surveillance systems in a hospital to support employing SPC tools to prevent increased SSI occurrences and improve patient care. | De Simone et al. (2020) recommended the universal use of standardized antiseptic protocols in all abdominal surgeries to reduce the incidence of SSIs. They also urged more to fill gaps in evidence. | Li et al. (2022) recommend using wound-edge protectors in abdominal surgery as a standard procedure, especially in cases involving patients at higher risk for infection. | The authors recommend that the use of an antibacterial-coated suture be a routine practice in elective abdominal surgery to reduce the incidence of SSIs (Matz et al., 2024). |
| Explain how this article supports your proposed PICO(T) question and Capstone Change Project. | This study supports the PICOT question by evidencing that standardized monitoring protocols reduce SSIs in surgical patients. The intervention is appropriate in the context of evidence-based practices for infection control. | The findings address the PICOT question by providing direct evidence of effective intraoperative measures for the prevention of SSIs among surgical patients. | This article provides strong evidence for including wound-edge protectors in the standard infection control armamentarium to reduce SSIs in surgical patients and thus directly supports the intervention in the PICOT question. | This research supports the PICOT question that antibacterial suture use can prevent the occurrence of SSIs among hospitalized surgical patients for a particular 30-day postoperative period. |
| Criteria | Article 5 | Article 6 | Article 7 | Article 8 |
| APA Reference
(include the GCU permalink or working link used to access the article) |
Mueller, T., Kehl, V., Egert-Schwender, S., Friess, H., Novotny, A., & Reim, D. (2022). Peritoneal antiseptic irrigation to prevent surgical site infection after laparotomy for hepatobiliary or gastrointestinal surgery (PAISI)—Protocol for a randomized controlled study. Trials, 23(1). https://doi.org/10.1186/s13063-022-06975-6 | Scrimshire, A. B., Booth, A., Fairhurst, C., Reed, M., Tadd, W., Laverty, A., Corbacho, B., Torgerson, D., & McDaid, C. (2020). Scaling up quality improvement for surgical teams (QIST) – avoiding surgical site infection and anaemia at the time of surgery: Protocol for a cluster randomized controlled trial. Trials, 21(1). https://doi.org/10.1186/s13063-020-4152-3 | Seidelman, J. L., Mantyh, C. R., & Anderson, D. J. (2023). Surgical site infection prevention. JAMA, 329(3), 244–252. https://doi.org/10.1001/jama.2022.24075
|
Wolfhagen, N., Boldingh, Q. J. J., Boermeester, M. A., & de Jonge, S. W. (2022). Perioperative care bundles for the prevention of surgical-site infections: Meta-analysis. British Journal of Surgery, 109(10). https://doi.org/10.1093/bjs/znac196 |
| Purpose/Aim of Study | This study proposes to assess the effectiveness of peritoneal antiseptic irrigation in the prevention of SSI following laparotomy for hepatobiliary or gastrointestinal surgery. It evaluates whether the use of antiseptic irrigation during surgical operation can help reduce infection rate after operation (Mueller et al., 2022). | The purpose of this study was to assess the impact of a quality improvement program called the QIST program on the rates of STSs and the management of surgical anemia. The purpose was to know whether the structure of care protocols could lower infection and enhance health outcomes (Scrimshire et al., 2020). | The aim of this study was to describe contemporary evidence-based practices regarding the prevention of SSIs. In line with the available information and analysis of the theorists’ recommendations, the authors endeavored to identify the most effective processes and activities related to diverse SSI prevention in a surgical environment (Seidelman et al., 2023). | Perioperative care bundles designed for this study were aimed at examining the impact of the measures put in place to prevent SSIs. The study was therefore conducted to determine if, overall, the implementation of the enhanced perioperative care bundles can reasonably address surgical infection in patients (Wolfhagen et al., 2022). |
| Research questions (Qualitative)/Hypothesis (Quantitative) | The research question was: “Does peritoneal antiseptic irrigation reduce the incidence of SSIs following laparotomy for GI or hepatobiliary surgeries?” The hypothesis was that antiseptic irrigation would decrease SSIs compared to saline irrigation or no irrigation. | The research question was whether quality improvement protocols could help reduce SSIs and improve anemia management in surgical patients. It was hypothesized that more structured care bundles would minimize SSI and improve the patient outcome of surgical concerns. | The research question was: “What are the best practices for preventing SSIs among surgical patients?” It was hypothesized that standardized infection prevention protocols would include all care bundles and timely antibiotic administration, thus significantly decreasing SSIs. | The question was: “Do perioperative care bundles reduce the incidence of SSIs in surgical patients?” The hypothesis was that the use of structured care bundles encompassing infection prevention measures decreases SSIs compared to non-bundle care. |
| Design
Type of quantitative or type of qualitative study design |
Quantitative; randomized controlled trial | Quantitative study; cluster randomized controlled trial | Qualitative study; comprehensive literature review and synthesis of evidence-based practices | Quantitative study; systematic review and meta-analysis of randomized controlled trials (RCTs) for the efficacy of perioperative care bundles |
| Setting
Where did the study take place? What type of setting – inpatient, outpatient, etc.? |
The study was performed in an inpatient surgical setting, where hepatobiliary and gastrointestinal surgeries were commonly performed. | The study was conducted across numerous surgical units, ensuring broad clinical settings. | The review included a range of inpatient and outpatient surgical settings and focused on those surgeries that are most common or at the highest risk for SSIs. | Data for this study were obtained from various inpatient and outpatient surgical units. The meta-analysis pooled data from multiple studies across several types of surgeries. |
| Sample
Number and characteristics of participants |
The study expects to enrol 300 patients undergoing laparotomy due to hepatobiliary and gastrointestinal tract conditions. Patients are randomly allocated for antiseptic or saline irrigation (Mueller et al., 2022). | In this cluster trial, the participants were surgical teams and their patients. The sample size was large, with many participating hospitals and surgical teams. | The study did not collect primary data; instead, the data was synthesized from various clinical studies with a wide variety of patients and types of surgeries. | The meta-analysis included more than 10,000 surgical patients from multiple studies, permitting a robust analysis of effectiveness in perioperative care bundle interventions. |
| Methods
Interventions/Instruments |
Patients in the open-labeled intervention group underwent peritoneal antiseptic irrigation procedures during surgery; the control group received normal saline. Infection rates were monitored during rehabilitation after the operation, and outcomes were measured 30 days postoperatively. | The care bundle instituted as part of the intervention consisted of care elements related to infection control, anemia, and surgery. To assess the intervention’s impact, infection and anemia rates taken at the end of the intervention were compared to those taken before the intervention (Scrimshire et al., 2020). | The authors systematically analyzed the literature on preventing SSI using antibiotics, proper wound management, and care bundles. They categorized the results according to the merits of each approach from prior research and recommendations for practice. | The authors pooled data from RCTs that focused on implementing perioperative care bundles, which often entailed preoperative antibiotics, operating theatre cleanliness, and postoperative management of the surgical site. They compared the pre- and post-introduction of care bundles regarding infection prevalence (Wolfhagen et al., 2022). |
| Analysis
How was the data collected and analyzed? |
The infection rates were compared between the two groups using statistically standard procedures (Mueller et al., 2022). The main outcome measure was the rate of SSIs, while secondary outcomes included recovery time and further interventions required by the patients. | The rates of infection and anemia of the two surgical teams were calculated and statistically compared before and after the intervention. | The data analysis was performed by categorizing categorization and synthesizing the evidence on SSI prevention strategies. The review has focused on identifying the most widely supported and effective interventions across different surgical disciplines. | It adopted statistical methods in conducting a meta-analysis via pooled odds ratios and estimates of risk reduction to unravel the effects of care bundles on SSI rates. The studies’ heterogeneity was assessed to show that the results were not spurious. |
| Outcomes/key findings of the study and implications for nursing practice (Summary of study results) | Although the full results from this study are pending, preliminary data reflect that SSI rates in GI-hepatobiliary surgery with antiseptic irrigations are reduced. This is consistent with the hypothesis that such antiseptic solutions, relative to saline, are better at preventing infection (Mueller et al., 2022). | The QIST intervention could establish significantly lower SSIs with the added improvement in anemia management. The better the implementation of the intervention, the better the results for patients. This showed the benefits of structured care bundles (Scrimshire et al., 2020). | The study confirmed that preoperative antibiotic prophylaxis combined with perioperative care bundles and postoperative wound management significantly reduce SSI rates. Indeed, it has been determined that proper adherence to these protocols is key to their effectiveness (Seidelman et al., 2023). | The study revealed that using perioperative care bundles significantly reduced SSI rates. More effective bundles included preoperative antibiotic prophylaxis, skin antisepsis, and proper wound management after surgery (Wolfhagen et al., 2022). |
| Recommendations of the Researcher | Pending final results, this trial suggests adding antiseptic irrigation of the peritoneum to the infection control bundle of care for high-risk surgeries. | Scrimshire et al. (2020) recommended further scaling the QIST program with greater numbers of surgical teams to institutions in order to significantly reduce SSIs and improve perioperative care. | The authors propose a universal adoption of evidence-based care bundles with strict adherence to infection prevention guidelines in all surgical settings (Seidelman et al., 2023). | Wolfhagen et al. (2022) recommend that the routine use of perioperative care bundles in all surgical units be accepted as standard practice for reducing SSIs and improving overall surgical outcomes. |
| Explain how this article supports your proposed PICO(T) question and Capstone Change Project. | This study lays a good foundation for the intervention in the PICOT question. Antiseptic irrigation thus can reduce SSIs within 30 days postoperatively from surgical patients. Since this is a traditional usage, antiseptics stand to be easily accepted by all (Mueller et al., 2022). | This supports the PICOT framework by showing that structured infection control and care bundle interventions can decrease SSI outcomes in surgical patients and, therefore, would have a wider application to the proposed change project. | It provides evidence for the PICOT question that standardized infection control practices reduce SSIs in surgical patients, for instance, in a 30-day postoperative period. | This study strongly supports the PICOT question since there is evidence that structured and standardized infection control protocols, such as care bundles, can reduce SSIs in surgical patients within a specified postoperative period. |
References
Anderson, D. J., Ilieş, I., Foy, K., Nehls, N., Benneyan, J. C., Lokhnygina, Y., & Baker, A. W. (2020). Early recognition and response to increases in surgical site infections using optimized statistical process control charts—the early 2RIS Trial: A multicenter cluster randomized controlled trial with stepped wedge design. Trials, 21(1). https://doi.org/10.1186/s13063-020-04802-4
De Simone, B., Sartelli, M., Coccolini, F., Ball, C. G., Brambillasca, P., Chiarugi, M., Campanile, F. C., Nita, G., Corbella, D., Leppaniemi, A., Boschini, E., Moore, E. E., Biffl, W., Peitzmann, A., Kluger, Y., Sugrue, M., Fraga, G., Di Saverio, S., Weber, D., . . . Catena, F. (2020). Intraoperative surgical site infection control and prevention: A position paper and future addendum to WSES intra-abdominal infections guidelines. World Journal of Emergency Surgery, 15(1). https://doi.org/10.1186/s13017-020-0288-4
Li, X., Lin, H., Zhu, L., Chen, J., Lei, S., Li, B., & Su, S. (2022). The clinical effectiveness of wound edge protectors in reducing surgical site infection after abdominal surgery: Meta-analysis. BJS Open, 6(3). https://doi.org/10.1093/bjsopen/zrac065
Matz, D., Engelhardt, S., Wiencierz, A., Soysal, S. D., Misteli, H., Kirchhoff, P., & Heizmann, O. (2024). Do antibacterial skin sutures reduce surgical site infections after elective open abdominal surgery?—A prospective, randomized controlled single-center trial. Journal of Clinical Medicine, 13(22), 6803. https://doi.org/10.3390/jcm13226803
Mueller, T., Kehl, V., Egert-Schwender, S., Friess, H., Novotny, A., & Reim, D. (2022). Peritoneal antiseptic irrigation to prevent surgical site infection after laparotomy for hepatobiliary or gastrointestinal surgery (PAISI)—Protocol for a randomized controlled study. Trials, 23(1). https://doi.org/10.1186/s13063-022-06975-6
Scrimshire, A. B., Booth, A., Fairhurst, C., Reed, M., Tadd, W., Laverty, A., Corbacho, B., Torgerson, D., & McDaid, C. (2020). Scaling up quality improvement for surgical teams (QIST) – avoiding surgical site infection and anaemia at the time of surgery: Protocol for a cluster randomised controlled trial. Trials, 21(1). https://doi.org/10.1186/s13063-020-4152-3
Seidelman, J. L., Mantyh, C. R., & Anderson, D. J. (2023). Surgical site infection prevention. JAMA, 329(3), 244–252. https://doi.org/10.1001/jama.2022.24075
Wolfhagen, N., Boldingh, Q. J. J., Boermeester, M. A., & de Jonge, S. W. (2022). Perioperative care bundles for the prevention of surgical-site infections: Meta-analysis. British Journal of Surgery, 109(10). https://doi.org/10.1093/bjs/znac196
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
In nursing practice, accurate identification and application of research is essential to achieving successful outcomes. The ability to articulate research data and summarize relevant content supports the student’s ability to further develop and synthesize the assignments that constitute the components of the capstone project.
This assignment will be used to develop a written implementation plan.
For this assignment, provide a synopsis of the review of the research literature. Using the “Literature Evaluation Table,” determine the level and strength of the evidence for each of the eight research articles you have selected. The articles should be current (published within the past 5 years) and closely relate to the PICOT question developed earlier in this course.
Literature Evaluation Table
The articles may include quantitative research, descriptive analyses, longitudinal studies, or meta-analysis articles. A systematic review may be used to provide background information for the purpose or problem identified in the proposed capstone project.
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
Client’s Note:
- PICOT: In hospitalized patients with surgical wounds (P), how does the implementation of a standardized infection control protocol (I) compared to the usual infection control practices (C) affect the rate of surgical site infections (O) within a 30-day postoperative period(T)?

