JS is a 42-year-old man who lives in the Midwest and is Highly Allergic to Dust and Pollen, and has a History of Mild Asthma
J.S. is a 42-year-old man who lives in the Midwest with a known medical history of mild asthma. J.S. is admitted to the emergency by his wife, who reports that J.S. has wheezing and is unresponsive to a fluticasone/salmeterol inhaler. J.S. is allergic to pollen and dust. His wife highlights that J.S. is anxious with shortness of breath and is unable to breathe while down and is. Therefore, breathing uses accessory muscles. At the emergency room, J.S. is administered 4L of oxygen through a nasal cannula and intravenous dextrose five at a rate of 75 ml per hour. Arterial blood gas revealed that J.S. has a partial oxygen pressure of 55, a partial carbon dioxide pressure of 48, a pH of 7.31, and a bicarbonate level of 26. J.S.’s vital signs reveal a heart rate of 124 bpm, a temperature of 100.40F, blood pressure of 152/84mmHg, and a respiratory rate of 42 breaths per minute.
Asthma is a chronic respiratory disease that occurs through inflammation of the airway, obstruction of intermittent airflow, and bronchial hyperresponsiveness (Hashmi et al., 2022). Causes of asthma include drugs, stress, irritants, environmental pollutants, environmental allergens, exercise, rhinitis, obesity, occupational hazards, viral respiratory tract infections, chronic sinusitis, gastroesophageal reflux disease, and perinatal factors such as maternal smoking and prematurity. Drugs that induce asthma include beta blockers and non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin. NSAIDs decrease the production of prostaglandins and thromboxanes, leading to increased production of leukotrienes. Leukotrienes induce bronchospasm, leading to asthma exacerbation. Obesity in early infancy increases the risk of asthma in children. Exercise causes heat loss from the airway, an increase in airway reactivity, and water loss from the airway, leading to bronchoconstriction. Occupations such as painting, farming, and manufacturing increase the risk of asthma. J.S. is a known asthmatic with allergic asthma exacerbated by dust and pollen.
The asthma symptoms include wheezing, cough, shortness of breath, chest tightness, and chest pain. Patients diagnosed with asthma mostly present with wheezing. In mild asthma, wheezing is expiratory; in severe asthma, wheezing is expiratory and inspiratory. Wheezing does not necessarily mean that a patient has asthma since it can occur due to other causes of airway obstruction, such as heart failure (Hashmi et al., 2022). J.S. presents to the emergency room with wheezing that is unresponsive to a fluticasone/salmeterol inhaler and shortness of breath. Patients with a history of asthma experience symptoms based on seasonal changes, exercise intensity and duration, temperature, humidity, upper respiratory tract infections, allergens, and pollutants such as nitrous oxide. J.S.’s current asthma attack is exacerbated by dust and pollen. Some asthma patients experience nocturnal symptoms such as shortness of breath when lying down caused by increased airway resistance and exaggerated response to the variation in the normal circadian airflow (Hashmi et al., 2022). J.S. reported an inability to breathe while lying down, forcing him to breathe using accessory muscles.
A patient’s medical history is essential in evaluating if the symptoms are related to asthma, the severity of asthma, and identifying the exacerbating factors. J.S.’s medical history shows he is a known asthmatic with mild asthma. He presents with shortness of breath, wheezing, and orthopnea, which are manifestations of asthma. The exacerbating factors for J.S.’s asthma are identified as pollen and dust. The patient’s vital signs showed a blood pressure of 152/84 mmHg, signifying stage 1 hypertension. The average heart rate is 60 to 100 beats per minute; therefore, J.S. has a higher heart rate of 124 beats per minute. The average respiratory rate is 12 to 16; therefore, J.S. has a higher respiratory rate of 42. The average body temperature is between 97F and 99F; therefore, J.S. has a slightly high temperature of 100.40F. A severe asthmatic episode presents with a heart rate greater than 120 bpm, respiratory rate greater than 30 bpm, and loud wheezing. J.S.’s vital signs signify a severe asthmatic episode.
Evaluation of an asthmatic patient includes measurement of arterial blood, serum immunoglobin E, pulse oximetry, chest C.T. scan, periostin, chest radiography, nuclear imaging, electrocardiography, magnetic resonance imaging, allergy skin testing, 24-hour pH monitoring, exercise testing, peak flow monitoring, bronchoprovocation, and pulmonary function testing (Hashmi et al., 2022). Arterial blood gas evaluation of J.S.’s respiratory function showed a pH of 7.31, PaCO2 of 48, HCO3 of 26, and PaO2 of 55. The normal partial pressure of oxygen (PaO2) is 75 mmHg to 100 mmHg; therefore, J.S. has a low PaO2 of 55 mmHg. The normal partial pressure of carbon dioxide (PaCO2) is 38 mmHg to 42 mmHg; therefore, J.S. has a high PaCO2 of 48 mmHg. Normal arterial blood pH is 7.38 to 7.42; therefore, J.S. has a low pH of 7.31. The average bicarbonate level (HCO3) is 22 mEq/L to 28 mEq/L; therefore, J.S. has a normal bicarbonate level of 26 mEq/L. Essentially, abnormal results revealed by J. S’s arterial blood gas are low PaO2, high PaCO2, and low pH, showing that he has respiratory acidosis.
Asthma management focuses on preventing symptoms, decreasing morbidity, and preventing acute episodes (Hashmi et al., 2022). J.S. is unresponsive to the fluticasone/salmeterol inhaler. Salmeterol is a long-acting beta-two agonist, while fluticasone is a corticosteroid (Remien & Bowman, 2022). The fluticasone/salmeterol inhaler is efficient for mild asthma; therefore, J.S. is unresponsive because he has severe asthma. Severe asthma is managed using high-dose inhaled corticosteroids and long-acting beta-agonists such as salmeterol. J.S.’s medication should be adjusted to salmeterol and a high dose of fluticasone. In addition, immediate oxygen therapy is administered in severe asthma through high-flow nasal cannulas (McNamara et al., 2022). J.S. is started on 4 L oxygen by nasal cannula and intravenous (IV) D5W at 75 mL/hr, and he and his wife are trained in allergen avoidance. J.S.’s asthma attack is exacerbated by pollen and dust; therefore, J.S. and his wife are taught how to identify allergens that can exacerbate asthma. Patient education on seasonal changes is crucial for J.S. to understand how and when to avoid allergens such as pollen.
References
Hashmi MF, Tariq M, Cataletto ME. (2022). Asthma. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430901/.
McNamara, P. S., Clayton, D., Burchett, C., Compton, V., Peak, M., Clark, J., & Jones, A. P. (2022). Humidified and standard oxygen therapy in acute severe asthma in children (HUMOX): A pilot randomized controlled trial. PloS one, 17(2), e0263044. https://doi.org/10.1371/journal.pone.0263044.
Remien K, Bowman A. (2022). Fluticasone. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542161/.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
J.S. is a 42-year-old man who lives in the Midwest and is highly allergic to dust and pollen, and has a history of mild asthma. J.S.’s wife drove him to the emergency room when his wheezing was unresponsive to his fluticasone/salmeterol (Advair) inhaler. J.S. was unable to lie down and began to use accessory muscles to breathe. J.S. is immediately started on 4 L oxygen by nasal cannula and intravenous (IV) D5W at 75 mL/hr. A set of arterial blood gases is sent to the laboratory. J.S. appears anxious and says that he is short of breath.
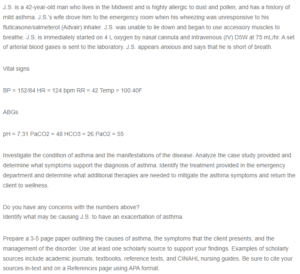
JS is a 42-year-old man who lives in the Midwest and is Highly Allergic to Dust and Pollen, and has a History of Mild Asthma
Vital signs
BP = 152/84 HR = 124 bpm RR = 42 Temp = 100.40F
ABGs
pH = 7.31 PaCO2 = 48 HCO3 = 26 PaO2 = 55
Investigate the condition of asthma and the manifestations of the disease. Analyze the case study provided and determine what symptoms support the diagnosis of asthma. Identify the treatment provided in the emergency department and determine what additional therapies are needed to mitigate the asthma symptoms and return the client to wellness.
Do you have any concerns with the numbers above?
Identify what may be causing J.S. to have an exacerbation of asthma.
Prepare a 3-5 page paper outlining the causes of asthma, the symptoms that the client presents, and the management of the disorder. Use at least one scholarly source to support your findings. Examples of scholarly sources include academic journals, textbooks, reference texts, and CINAHL nursing guides. Be sure to cite your sources in-text and on a References page using APA format.


