Healthcare-Legal Aspects and Ethics
The healthcare sector is regulated by various national and state laws to ensure that patients are not negatively affected by ethical dilemmas in healthcare practice. This paper draws the connection between law and ethics in the healthcare setting by focusing on a case scenario where a patient’s right to confidentiality has been breached due to a nurse’s actions and ethical dilemmas. The paper also reviews the present status of patient rights under the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA) and how the rights in these two acts relate to the case scenario. The paper also reviews how a healthcare provider can use the Affordable Care Act (ACA) mandates to resolve ethical dilemmas in healthcare and some relevant healthcare laws enacted in the last two decades that could be applied in the case scenario. The final part of the paper provides recommendations on what could be done to prevent ethical violations from taking place. Our assignment help will hone your writing prowess for papers that will awe your professors.
Patient rights under the Health Insurance Portability and Accountability Act (HIPAA)
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that focuses on creating national standards for protecting sensitive patient health data from being shared without the knowledge or consent of the patient (Collins, 2020). The present status of the Act includes the security and privacy rule. The privacy rule focuses on the disclosure and use of a person’s health information by covered entities. The government also has standards for people’s rights to control and understand how their health data is used.
The main goal of the rule is to ensure that people’s health data is adequately protected while allowing the flow of required health data to promote and provide high-quality health care and protect the public’s well-being and health. The rule also provides a balance that allows important use of health information while preserving a patient’s privacy. The security rule protects all personally identifiable health data created, received, maintained, or transmitted by a covered entity.
In this case, these rights were violated when Nurse Andrea shared Grandma Lucy’s medical records with Philip and other people. Although Nurse Andrea’s actions were aimed at preventing Grandpa Peter from meeting his own needs at the expense of Phillip and Grandma Lucy, the steps were not right. This is because healthcare providers are only required to disclose information relevant to a patient’s treatment and welfare to individuals directly involved with the patient’s care, which were, in this case, Grandpa Peter and other physicians attending to Granma Lucy.
Patients’ rights under the Affordable Care Act (ACA)
The Affordable Care Act regulates the relationship between a patient and health insurers, health plans, and the healthcare system (Gorin et al., 2014). One of the rights in the Act is the right to information about healthcare quality. This right provides that individuals should receive accurate, understandable information about healthcare professionals, health plans, clinics, and hospitals to choose their care wisely. This includes receiving details of their health plan provided precisely and clearly, quickly learning about the experience, education, licensure, and bad records on the professional papers of healthcare providers, and quickly acquiring various statistics on clinics and hospitals. Statistics may include how often specific procedures have been performed, comparisons between procedures’ performance, and how to make complaints against clinics and hospitals.
The second right is the right to choose a healthcare provider. The Act requires health plans to give patients information on different coverage options so that they do not have to wait for the services they need. The third right is the right to emergency service. Health plans are required to inform patients where they can access emergency services near them and the fees they may be required to pay. The fourth right is the right to make decisions, whereby healthcare providers are required to give patients all the information they need to decide on their healthcare. The fifth right is the right to respect. Patients have a right to be treated with good manners and respect and should not be discriminated against. The sixth right is the right to confidentiality. Healthcare professionals, suppliers, and insurers are prohibited from discussing a patient’s health history with employers or anyone else unless the patient gives permission or when the exchange of information is necessary for the patient’s care. The seventh right is the right to complain. Patients have a right to report and demand quick resolution to any problems they may have with their healthcare, such as denied treatment, billing issues, poor treatment, long waiting times, and lack of services.
The right to respect, the right to confidentiality, and the right to complain protect Grandma Lucy and Grandpa Peter. The right to privacy protects Grandma Lucy by prohibiting healthcare providers from sharing her health information. The right to privacy also protects Grandpa Peter because it prohibits healthcare providers from sharing any information from the discussions he holds with them relating to Grandma Lucy’s health. The right to respect protects Grandma Lucy because it requires healthcare providers to treat her with respect by respecting her directive not to renew and give her the best care. The right to respect also protects Grandpa Peter by guaranteeing that he is treated with respect by being listened to and consulted on Grandma Lucy’s healthcare decisions. Grandpa Peter and Grandma Lucy are protected by the right to complain because Grandpa Peter can complain if Grandma Lucy does not receive the best care, such as the poor quality of care that has made Grandma Lucy develop bedsores.
ACA mandates honoring patient rights and benefits
The ACA mandates that providers must honor patient rights and benefits. Grandma Lucy and her son Phillip could benefit from the right to respect and right to confidentiality. Grandma Lucy is in no position to speak up and say what she wants but has already expressed her wishes not to be renewed even at the point of her death. Providers need to respect her wishes, and this could benefit Grandma Lucy because she would not have to endure pain. The right to confidentiality could help Phillip because he could discuss his wishes with the healthcare providers without Grandpa Peter knowing. After all, the current scenario shows that Grandpa Peter is hiding information from Phillip so that Phillip does not benefit.
ACA mandates resolving ethical dilemmas in healthcare
I could use these mandates to resolve ethical dilemmas in healthcare in different ways. First and foremost, respecting patients, orders can be used by respecting the autonomy of the patient and their family. Healthcare providers can also balance the benefits a patient gets from the healthcare services provided with the burdens of therapy to determine whether to honor the wishes of the patient and their family or consider renegotiating to come up with a mutually beneficial solution. The mandate to respect patients can also be used to not harm while offering benefit to the patient and seeking justice, thus ensuring that all patients receive the highest quality of care and are not denied healthcare services. The mandate to respect the confidentiality of the patient can be used to maintain honesty and integrity in the relationship between healthcare providers and patients and ensure that a patient’s healthcare information is protected.
Relevant healthcare laws enacted in the last two decades
One of the relevant healthcare laws enacted in the last two decades that could be applied in this case is the Patient Safety and Quality Improvement Act (PSQIA) of 2005. The Act protects healthcare workers reporting unsafe conditions. This Act focuses on encouraging healthcare workers to report medical errors while maintaining the right to patient confidentiality. Healthcare providers found breaching confidentiality are required to pay fines (Riley et al., 2008).
The second law is the Patient Safety Rule, which establishes a framework that healthcare providers and hospitals may use to voluntarily report information to Patient Safety Organizations on a confidential and privileged basis for analyzing and aggregating patient safety events.
How a new chief executive officer (CEO) of St. Michael’s Medical Center can prevent these ethical violations
As the new chief executive officer of St. Michael’s Medical Center, one of the measures I could take to prevent these ethical violations is introducing training programs to educate nurse leaders in the hospitals on how to create and maintain a culture of professional integrity. Nurse leaders need to understand their role in enforcing policies in the healthcare setting and supporting interventions to prevent and end physicians’ wrongdoings (DuBois et al., 2018). The second measure is creating a monitoring team in charge of monitoring the activities of nurses and investigating credible complaints while balancing privacy concerns with the need for transparency.
The third measure is using prescription drug monitoring plans to track drug prescription patterns to identify any odd behavior in a physician’s prescribing practice, hence preventing ethical issues before they arise. The fourth measure is creating a tracking system to track serious disciplinary actions and facilitate rapid response. Tracking misconduct is vital because it provides information informing decisions of committees looking for information about their physicians, disciplinary committees, and researchers intending to understand professional violations (DuBois et al., 2018). Tracking the consequences of wrongdoings also facilitates transparent evaluation by disciplinary boards and state medical boards. The fifth measure outlines the results of ethical misconduct in the employee handbook. This will help in ensuring that employees understand the consequences of their actions, hence preventing them from ethical violations. The results need to be severe, such as the suspension or revocation of medical licenses.
References
DuBois, J. M., Anderson, E. A., Chibnall, J. T., Diakov, L., Doukas, D. J., Holmboe, E. S., Koenig, H. M., Krause, J. H., McMillan, G., Mendelsohn, M., Mozersky, J., Norcross, W. A., & Whelan, A. J. (2018). Preventing egregious ethical violations in medical practice: Evidence-informed recommendations from a multidisciplinary working group. Journal of Medical Regulation, 104(4), 23-31. https://doi.org/10.30770/2572-1852-104.4.23
Gorin, S. H., Darnell, J. S., & Allen, H. L. (2014). Affordable Care Act. Encyclopedia of Social Work. https://doi.org/10.1093/acrefore/9780199975839.013.830
Riley, W., Liang, B. A., Rutherford, W., & Hamman, W. (2008). The Patient Safety and Quality Improvement Act of 2005. Journal of Patient Safety, 4(1), 13-17. https://doi.org/10.1097/pts.0b013e31816154b5
Sollins, H. (2020). Health Insurance Portability and Accountability Act (HIPAA). Encyclopedia of Behavioral Medicine, 1014-1015. https://doi.org/10.1007/978-3-030-39903-0_113
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Healthcare practitioners are ethically bound to respect the patient’s dignity and to make a positive effort to secure a comfortable and considerate atmosphere for the patient in such ways as providing appropriate gowns and drapes, private facilities for undressing, and clear explanations for procedures. There are guidelines to help all healthcare providers stay within the scope of their practices and operate within the law and the policies of any employing healthcare facility. (Judson & Harrison, 2021)
Healthcare-Legal Aspects and Ethics
Consider the following case from the course scenario on St. Michael’s Medical Center.
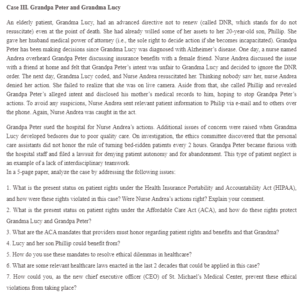
Case III. Grandpa Peter and Grandma Lucy
An elderly patient, Grandma Lucy, had an advanced directive not to renew (called DNR, which stands for do not resuscitate) even at the point of death. She had already willed some of her assets to her 20-year-old son, Phillip. She gave her husband medical power of attorney (i.e., the sole right to decide action if she becomes incapacitated). Grandpa Peter has been making decisions since Grandma Lucy was diagnosed with Alzheimer’s disease. One day, a nurse named Andrea overheard Grandpa Peter discussing insurance benefits with a female friend. Nurse Andrea addressed the issue with a friend at home and felt that Grandpa Peter’s intent was unfair to Grandma Lucy and decided to ignore the DNR order. The next day, Grandma Lucy coded, and Nurse Andrea resuscitated her. Thinking nobody saw her, nurse Andrea denied her action. She failed to realize that she was on live camera. Aside from that, she called Phillip and revealed Grandpa Peter’s alleged intent and disclosed his mother’s medical records to him, hoping to stop Grandpa Peter’s actions. To avoid any suspicions, Nurse Andrea sent relevant patient information to Philip via e-mail and to others over the phone. Again, Nurse Andrea was caught in the act.
Grandpa Peter sued the hospital for Nurse Andrea’s actions. Additional issues of concern were raised when Grandma Lucy developed bedsores due to poor quality care. On investigation, the ethics committee discovered that the personal care assistants did not honor the rule of turning bed-ridden patients every 2 hours. Grandpa Peter became furious with the hospital staff and filed a lawsuit for denying patient autonomy and for abandonment. This type of patient neglect is an example of a lack of interdisciplinary teamwork.
In a 5-page paper, analyze the case by addressing the following issues:
- What is the present status of patient rights under the Health Insurance Portability and Accountability Act (HIPAA), and how were these rights violated in this case? Were Nurse Andrea’s actions right? Explain your comment.
- What is the present status of patient rights under the Affordable Care Act (ACA), and how do these rights protect Grandma Lucy and Grandpa Peter?
- What are the ACA mandates that providers must honor regarding patient rights and benefits and that Grandma?
- Lucy and her son Phillip could benefit from?
- How do you use these mandates to resolve ethical dilemmas in healthcare?
- What are some relevant healthcare laws enacted in the last two decades that could be applied in this case?
- How could you, as the new chief executive officer (CEO) of St. Michael’s Medical Center, prevent these ethical violations from taking place?
Please cite learning resources in APA format.

