Functional Health Pattern
Profile and Developmental History
The case is of a 75-year-old cisgender Caucasian male presenting to the clinic for a routine prostate examination. He reports complaints of headaches with varying intensity for the past two weeks. The patient is responsive and cooperates with caregivers in the care provision processes. He understands several aspects of his health, including the need and significance of various healthcare procedures in health management. The patient is currently in the eighth stage of Erickson’s developmental stages. Aspects such as acceptance, a sense of wholeness, and a feeling of peace evident in the patient’s case are consistent with the integrity postulates of the eighth stage (Gross, 2020). Through his responses, he is at peace with his current life. He also retorted that coming to the clinic regularly rejuvenates his sense of success and acceptance in his old age.
Health Assessment of the Major Systems
A review of the respiratory systems revealed that the patient had nonlabored breathing. The breathing was also rhythmic. Palpation of the posterior and anterior chest revealed no masses, tenderness, or crepitus. He had clear lung sounds. Next, cardiovascular systems assessment revealed rhythmic heart rates. The patient had a blood pressure of 140/86mmHg and a pulse rate of 98 beats per minute. There was a visible jugular venous pulse at rest. Further, the assessment of the musculoskeletal system revealed that the patient had a good balance and normal gait. He demonstrated an active range of motion in all of his joints. There was no evidence of swelling, tenderness, or nodules in his joints. His skin was dry and warm to touch.
Health Perception and Health Management Pattern
The patient defined his pain as a diffuse type, normally appearing in the morning and alleviated by rest. He further noted that the pain was of varying intensity, with an average pain score of 5. He noted that five years ago, he was healthier and had minimal reasons to seek any medical intervention. He is hopeful and happy with his current life and noted that he hopes to be happier as he ages. Five years into the future, he sees himself as a healthy adult who will have accomplished most of the things he hoped to achieve. He further reiterated that he would have no regrets about his life and that he would be at peace with whatever came after.
The patient has no known allergies. His past medical history was negative for any accidents, head injuries, or head surgeries. He is a known diabetic, having been diagnosed with the disease ten years ago. He has since been taking his anti-diabetic medications. Further, the patient demonstrated excellent knowledge of his medications. He noted that he has been taking metformin and gliclazide for the management of his diabetes. He has also been taking Tylenol to manage his headaches. He added that he has been taking his anti-diabetic medications religiously since his diagnosis and had no recall of any missed doses.
The patient has excellent health-seeking behaviour. He is compliant with his medication regimen, frequents healthcare setups for medical checkups, and utilizes various community resources available for preventive healthcare, such as the CDC website. He is a known smoker, taking two cigarettes per day. He is also a binge alcohol drinker but has a negative history of illicit substance use. In addition, the patient has a normal posture and gait. He seems responsive, alert, and attentive and has no signs of swelling on the face. His skin colour is consistent and uniform. The patient had a body temperature of 98 degrees, a blood pressure of 140/89mmH, a pulse rate of 98 beats per minute, and a respiratory rate of 17 breaths per minute. He has an oxygen saturation of 96%.
Nutritional Metabolic Pattern
The patient takes a balanced diet and drinks at least five glasses of water daily. He has a negative recall of any nausea and vomiting. Assessment of the skin revealed that the patient’s skin was warm to the touch and consistent in colour. There were no signs of rash, swelling, tenderness, or any other skin lesions. His hair was fine on touch, with visible even distribution. There was no sign of hirsutism or baldness. The nails were smooth with normal curvature. There was no sign of clubbing. His capillary was refilled within two seconds. He had a listed weight of 239 pounds, a height of 5 feet 11 inches, and a calculated BMI of 33.3. The patient reported not having any feeding precautions. He eats the most available foods at will and doesn’t watch over his caloric intake. He occasionally takes food supplements.
Elimination Pattern
The patient reported to be passing stool twice daily. His last bowel movement was in the morning, just before he presented for care. He noted that he suffered from constipation two weeks ago and has since been taking a lot of fluids. In his last bowel movement, he reported having passed a normal stool with no unusual colour or smell. He denied taking any medication to aid his bowel movements. He has a negative history of any GI surgery or procedure. His urinary habits are consistent and mostly follow his fluid intake. He passed pale yellow and odourless urine. He denied having experienced any recent changes in his urinary habits. The patient denied having any urinary frequency, urgency, inconsistency, dysuria, and nocturia. He has a negative history of bladder surgeries. Abdominal assessment revealed no distension, tenderness, or abnormal bowel sounds.
Activity Exercise Pattern
The patient is a retired military personnel. He is currently working as a counsellor for ex-marines. On a normal day, he wakes up, attends to his animals and crops, and then proceeds to his counselling office. Currently, he can execute most activities of daily living without aid. He likes swimming and hiking. The patient rarely exercises. He noted that his schedule is too tight and does not allow him more time to exercise.
Sexuality Reproduction Pattern
The patient is a 75-year-old cisgender male. He denies having any erectile dysfunction. He reported having symmetrical testicles with no swelling, colour changes, or tenderness. He also denied having any prostatic problems, as all his prostate examinations have been negative for swelling. He reports being sexually active and indulges in sexual activities occasionally. He has a negative history of any STDs or sexual abuse.
Sleep-Rest Pattern
The patient reported having a definite sleeping habit. He sleeps before 10 in the evening and wakes up at 5 in the morning. He does not take any medication to induce or maintain sleep. He reports having good quality sleep as he never experiences unnecessary awakenings. He rarely experiences difficulties falling or maintaining sleep or changes in the pattern of his sleep. He has never received any reports of snoring. He often feels rested after a night’s sleep. He rarely naps during the day because of his busy day schedule.
Cognitive Pattern
The patient is conscious and oriented to place, time, and event. He is responsive and answers questions asked appropriately. He is also able to communicate and recall information. His decision-making ability is excellent. He also has a good attention span. He has a good memory, sound judgment and reasoning, and excellent verbal and mathematical abilities.
Role-Relationship Pattern
The patient is married to one wife and has five children. Their communication is excellent as they communicate frequently and stay together. He is the provider of the family. His wife is also an accomplished doctor who aids in providing for the family. His family is concerned with his illness, and two of his sons accompanied him to the clinic. He is a former military man, having served in missions around the globe. The most important people in his life are his wife and children. He actively participates in community activities and is currently the chairperson of three social groups where he lives. His family members cared a lot for him, and some accompanied him to the clinic.
Perception/Neurological Assessment
The patient has good vision and hearing and does not require assistive hearing or visual devices. His perception of taste and smell is also intact. He denied having any difficulties in any sense or using assistive devices. A neurological exam revealed that the patient is conscious, has a good memory, and has normal speech.
Coping-Stress Tolerance Pattern
The patient noted that the most stressful event in his life was when his father died. He noted that his illness has had little impact on his stress level as he has a supportive family. He is currently under the Medicaid program but can still afford out-of-pocket payments for his medical bills. He has not had any significant life changes in the past year. His family often helps him cope with difficult moments in his life. He denies using substances of abuse to help him cope.
Value Belief Pattern
The most important thing for the client is his family. He hopes to maintain health and happiness. His major sources of hope and strength are his children and wife. He is a Catholic. He prays frequently and always asks God’s favor during his health-seeking durations. The patient currently serves as a chairperson on the Church’s board.
Summary
The presented case is of a 75-year-old old presenting for a routine prostate exam. Assessment findings revealed the presence of elevated blood pressure. Kario et al. (2022) described hypertension as a sustained elevation of blood pressure with a value exceeding 129/80mmHg. Comorbidity of hypertension and diabetes mellitus is common among the elderly groups (Abdelbagi et al., 2021). Assessment of the patient’s perception of life revealed that he is at peace with his current life. He also retorted that coming to the clinic regularly rejuvenates his sense of success and acceptance in his old age. These findings are a manifestation of the eight stages postulated by Erickson’s theory of psychological development (Gross, 2020). This may help design the care approach for the patient.
References
Abdelbagi, O., Musa, I. R., Musa, S. M., ALtigani, S. A., & Adam, I. (2021). Prevalence and associated factors of hypertension among adults with diabetes mellitus in northern Sudan: A cross-sectional study. BMC Cardiovascular Disorders, 21(1). https://doi.org/10.1186/s12872-021-01983-x
Gross, Y. (2020). Erikson’s stages of psychosocial development. The Wiley Encyclopedia of Personality and Individual Differences, 179–184. https://doi.org/10.1002/9781118970843.ch31
Kario, K., Mogi, M., & Hoshide, S. (2022). Latest hypertension research to inform clinical practice in Asia. Hypertension Research, 45(4), 555–572. https://doi.org/10.1038/s41440-022-00874-8
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
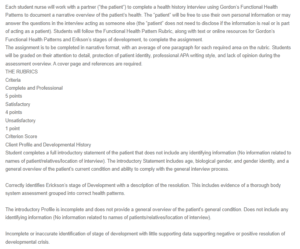
Functional Health Pattern
Each student nurse will work with a partner (“the patient”) to complete a health history interview using Gordon’s Functional Health Patterns to document a narrative overview of the patient’s health. The “patient” will be free to use their own personal information or may answer the questions in the interview acting as someone else (the “patient” does not need to disclose if the information is real or is part of acting as a patient). Students will follow the Functional Health Pattern Rubric, along with text or online resources for Gordon’s Functional Health Patterns and Erikson’s stages of development, to complete the assignment.
The assignment is to be completed in narrative format, with an average of one paragraph for each required area on the rubric. Students will be graded on their attention to detail, protection of patient identity, professional APA writing style, and lack of opinion during the assessment overview. A cover page and references are required.
Client Profile and Developmental History
Student completes a full introductory statement of the patient that does not include any identifying information (No information related to names of patient/relatives/location of interview). The introductory Statement includes age, biological gender, and gender identity, and a general overview of the patient’s current condition and ability to comply with the general interview process.
Correctly identifies Erickson’s stage of Development with a description of the resolution. This includes evidence of a thorough body system assessment grouped into correct health patterns.
The introductory Profile is incomplete and does not provide a general overview of the patient’s general condition. Does not include any identifying information (No information related to names of patients/relatives/location of interview).
Incomplete or inaccurate identification of stage of development with little supporting data supporting negative or positive resolution of developmental crisis.
Student includes identifying information that compromises the protection of the patient’s identity.
Omission of developmental history or omission of supporting evidence.
score of Client Profile and Developmental History,/ 5
Health Assessment of Major Systems
Student completes a full assessment of major health systems and is able to support any findings by documenting any concerns that the patient has regarding health in these areas:
1. Respiratory assessment
2. Cardiovascular assessment
3. Musculoskeletal assessment
The student has a full assessment of each area, however, does not support assessment with patient comments.
Omission of assessment data in any of the three areas.

