First Steps on Becoming a Grassroots Lobbyist or Advocate for Health Care Policy
Part 1A: Leave Behind
- The COVID-19 vaccine is available on a priority basis
- The first in line are persons aged 65 and above
- Healthcare workers are also in the first priority line
- However, what about home caregivers?
- Home caregivers are not considered a potential risk
- Ignoring the family/kin/friends of patients and the elderly staying at home is very risky
- When a 65+-year-old gets vaccinated and goes back home to be taken care of by 50-year-old kin, it makes little sense
- Home caregivers should be included in the first priority list of vaccination
- Failure to do so may result in a worse outbreak of the coronavirus.
- A second outbreak will negate any efforts made to control the current pandemic.
- The state government will incur more losses from a second outbreak
- More lives will be lost
- Crating another vaccine may take even longer
- More lives will be lost as a second vaccine awaits disbursement
- The state economy will plummet even further than it has already
- The healthcare system will be strained more than it currently is experiencing.
Part 1B: Rationale
In the US today, many older adults are taken care of by their middle-aged children at home. Not all persons aged 65 and above live in nursing homes or are hospital-bound either. These middle-aged caregivers are not old enough to meet the vaccination age limit. However, these caregivers live in constant fear of infecting their elderly loved ones who, though vaccinated, are exposed to their caregivers. Caregivers who interact with others outside of the elderly can contract COVID-19 and infect those they care for despite the latter getting vaccinated in phase one.
Caregivers do similar tasks as other workers and aides in nursing homes. These caregivers do the house chores, help with ADLs, administer medication, and feed their loved ones. The difference is that these caregivers carry out the responsibilities in houses and apartments, not in long-term care institutions, with no pay. The only thing that these caregivers lack is the title; otherwise, they are, in every way, essential healthcare workers who take care of patients who are very sick yet are exempt from the priority list of vaccination.
Healthcare workers have been listed as priority recipients of the COVID-19 vaccine, and hence, vulnerable older adults in assisted living facilities and nursing homes. However, family members taking care of vulnerable relatives in the community are categorized alongside the general populace and will not get access to the vaccine for months to come. This discrimination began well before the vaccination program began. Restrictive hospital policies prohibited caregivers from visiting their loved ones during the pandemic. Now, government policy restricts the same people from accessing the vaccine. When caregivers of frequently hospitalized persons are vaccinated, this will protect other hospitalized patients and the care providers as well.
Additionally, informal caregivers form an important healthcare system’s extension when patients stay at home. During the pandemic, caregivers may be the only close contact with the patient and, hence, the main source of COVID-19 infection risk. When some patients with certain medical conditions are vaccinated directly, such as those with severe allergies, compromised immune systems, or children below 16 years, they may not be in the recommendations for a long while because safety data on their medical conditions is lacking. When caregivers for these categories of persons are prioritized in the vaccination program, these patients will benefit from the protection the vaccine offers to those caregivers, even as it is indirectly extended to the patients themselves.
Lastly, vaccination could be a great stress reliever for caregivers who have endured much stress during the pandemic. Even before the pandemic, studies had shown that caregivers were and continue to be at high risk of poor health and psychosocial outcomes (Swinkels et al., 2019; Mello et al., 2017). Czeisler et al. (2020) have pointed out that 30% of caregivers have suicidal ideations compared to 11% of the rest of the populace during the COVID-19 pandemic. This raises the urgency to vaccinate caregivers, hoping they will find it easier to cope with their elderly and sick ones during this pandemic.
Scenario Surrounding the Legislative Visit
When I visited the legislative member of Congress, he was somewhat taken aback by my proposal to have caregivers taking care of patients outside of nursing homes, given top-tier vaccination priority. Although he read through my arguments, he still wasn’t convinced that these caregivers should be listed alongside the top-tier persons. More specifically, the Congress leader argued that more than one person attended to persons who received home care, and based on my argument, then it would mean that every person who cares for one patient at home would need to be vaccinated. For example, a 65+-year-old woman has two home caregivers, the first being her middle-aged son and the second being her young adult granddaughter. If the living arrangement is un-adjustable and allows the two to care for one person, then it would mean that both caregivers get vaccinated alongside the older adult. The legislator concluded that there were just not enough vaccines to cater to everyone on the first-tier priority list.
The three points I would state to oppose this reason that the legislature asserts are, first, it is a generalization; secondly, the assertion is unethical; and thirdly, the assertion will prove costly. In the first point, not all persons have multiple caregivers; in cases where this is so, the caregivers should be given the option of designating one person to care for the patient or move the patient to an assisted living facility. If caregivers refuse to take either of these options, then they forfeit their chances to be vaccinated in the first-tier priority group. The assertion is also unethical because it does not comply with the ethical principles of non-maleficence, utilitarianism, and justice. Thirdly, by not vaccinating the caregivers, the patients at home are at risk of infection, which will significantly cause a financial strain in the healthcare system and subsequently negatively impact the economy. The entire community is bound to feel the negative impacts of the surge in infection of those being taken care of at home and by their caregivers as well.
As a nurse working during this pandemic period, I have witnessed people coming to the hospital with symptoms of COVID-19. In most cases, the elderly patients brought in are either from nursing homes or staying in their own homes. Those brought in by their relatives face challenges different from those in the other category. The former category often finds that they can no longer visit their loved ones because of the strict hospital policies. On more occasions than one, I have witnessed the family of the patient who never gets to see their loved one until such a time the person has passed on. Some caregivers have had to struggle with the thought that they may have infected their loved ones. When such kin are presented with the opportunity to get vaccinated, that is, if they are placed as the top priority, they will be in a better position, especially psychologically, to care for their loved ones.
As mentioned earlier, most caregivers have to deal with their personal mental anguish from having to take care of their loved ones. COVID-19 has made it even harder for some to cope with the new normal. In the event that such caregivers die from either disease, psychological anguish, or become sick, it means that those they care for will have to get alternative places or care arrangements. If the elderly are taken to nursing homes, the homes will become overcrowded and risk patients to coronavirus infection. That said, the caregiver’s health should be prioritized along with those whom they care for because, by so doing, the pandemic will be better contained.
References
Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., … & Rajaratnam, S. M. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049.
Mello, J. D. A., Macq, J., Van Durme, T., Cès, S., Spruytte, N., Van Audenhove, C., & Declercq, A. (2017). The determinants of informal caregivers’ burden in the care of frail older persons: a dynamic and role-related perspective. Aging & mental health, 21(8), 838-843.
Swinkels, J. C., Broese van Groenou, M. I., de Boer, A., & Tilburg, T. G. V. (2019). Male and female partner-caregivers’ burden: Does it get worse over time?. The Gerontologist, 59(6), 1103-1111.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
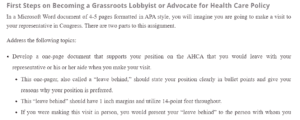
First Steps on Becoming a Grassroots Lobbyist or Advocate for Health Care Policy
In a Microsoft Word document of 4-5 pages formatted in APA style, you will imagine you are going to make a visit to your representative in Congress. There are two parts to this assignment.
Address the following topics:
- Develop a one-page document that supports your position on the AHCA that you would leave with your representative or his or her aide when you make your visit.
- This one-pager, also called a “leave behind,” should state your position clearly in bullet points and give your reasons why your position is preferred.
- This “leave behind” should have 1-inch margins and utilize 14-point font throughout.
- If you were making this visit in person, you would present your “leave behind” to the person with whom you speak during your visit.
First Steps on Becoming a Grassroots Lobbyist or Advocate for Health Care Policy
- Include a second page that describes your rationale for the position in your “leave behind” page, supported by at least two journal articles.
- Write a two-page brief to describe the scenario surrounding your legislative visit. Understanding the political affiliation of your representative, include answers to the following:
- Was your member in support or in opposition to the AHCA?
- State three points that you would cover in support or opposition to your representative’s position.
- How does your nursing experience influence the advocacy position that you take on the AHCA?
You may find it necessary to search for answers to the questions outside of the assigned reading.
On a separate references page, cite all sources using APA format. Helpful APA guides and resources are available in the South University Online Library. Below are guides that are located in the library and can be accessed and downloaded via the South University Online Citation Resources: APA Style page. The American Psychological Association website also provides detailed guidance on formatting, citations, and references in APA Style.
- APA Citation Helper
- APA Citations Quick Shee
- APA-Style Formatting Guidelines for a Written Essay
- Basic Essay Template
Please note that the title and reference pages should not be included in the total page count of your paper.