Evidence-Based Project, Part 3 – Critical Appraisal of Research
Part 3A: Critical Appraisal of Research
| Full APA formatted citation of the selected article. | Article #1 | Article #2 | Article #3 | Article #4 |
| Aoun, L., Almardini, S., Saliba, F., Haddadin, F., Mourad, O., Jdaidani, J., Morcos, Z., Saidi, I. A., Sanayeh, E. B., Saliba, S., Almardini, M., & Zaidan, J. (2024). GLP-1 receptor agonists: A novel pharmacotherapy for binge eating (Binge eating disorder and bulimia nervosa)? A systematic review. Journal of Clinical & Translational Endocrinology, 35, 100333. https://doi.org/10.1016/j.jcte.2024.100333
|
Bhattacharya, S., Goicoechea, C., Heshmati, S., Carpenter, J. K., & Hofmann, S. G. (2022). Efficacy of cognitive behavioral therapy for anxiety-related disorders: A meta-analysis of recent literature. Current Psychiatry Reports, 25(1), 19–30. https://doi.org/10.1007/s11920-022-01402-8 | Monteleone, A. M., Pellegrino, F., Croatto, G., Carfagno, M., Hilbert, A., Treasure, J., Wade, T., Bulik, C. M., Zipfel, S., Hay, P., Schmidt, U., Castellini, G., Favaro, A., Fernandez-Aranda, F., Shin, J. I., Voderholzer, U., Ricca, V., Moretti, D., Busatta, D., . . . Solmi, M. (2022). Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neuroscience & Biobehavioral Reviews, 142, 104857. https://doi.org/10.1016/j.neubiorev.2022.104857 | Reas, D. L., & Grilo, C. M. (2020). Psychotherapy and medications for eating disorders: Better together? Clinical Therapeutics, 43(1). https://doi.org/10.1016/j.clinthera.2020.10.006 | |
| Evidence Level *
(I, II, or III)
|
I | I | I | III |
| Conceptual Framework
Describe the theoretical basis for the study (If no one is mentioned in the article, say that here).**
|
While not based on a named theoretical model, the study is grounded in neurobiological principles and metabolic mechanisms of GLP-1 receptor agonists, such as their role in satiety and appetite regulation, which aligns with the pathophysiology of binge-type eating disorders.
|
The study does not explicitly mention a theoretical framework but is grounded in the established principles of Cognitive Behavioral Therapy (CBT) as an evidence-based treatment for anxiety-related disorders. | The authors do not identify a singular theoretical framework but reference evidence-based psychiatric treatment principles. The meta-review integrates psychological and pharmacological models for treating EDs and emphasizes mechanisms such as emotional dysregulation, neurobiological dysconnectivity, and behavioral reinforcement. | This article does not articulate a specific conceptual framework but implicitly supports a biopsychosocial treatment model. It integrates psychotherapy (CBT, IPT, DBT) and pharmacology as complementary approaches, recognizing the multifactorial nature of eating disorders. |
| Design/Method
Describe the design and how the study was carried out (In detail, including inclusion/exclusion criteria). |
A systematic review using PRISMA guidelines, examining preclinical and clinical studies evaluating the effects of GLP-1 agonists (like liraglutide and semaglutide) on binge-type EDs. Inclusion criteria: studies in humans with BED or BN, use of GLP-1 agonists, English language, and published in peer-reviewed journals. Exclusion: animal studies, case reports. The authors critically examined 12 studies, including small RCTs and pilot trials, to synthesize available evidence on pharmacotherapy outcomes. | Meta-analysis adhering to PRISMA guidelines. The authors systematically searched for randomized placebo-controlled trials (RCTs) published between 2017 and 2022 that evaluated the efficacy of CBT in treating anxiety-related disorders in adults. Inclusion criteria: RCTs focusing on adult populations with anxiety-related disorders, employing CBT interventions compared to placebo. Exclusion criteria: Non-randomized studies, studies without placebo controls, and those focusing on non-adult populations. | Systematic meta-review design that synthesizes findings from 13 meta-analyses and network meta-analyses covering interventions for anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED). Inclusion criteria: meta-analyses published in peer-reviewed journals from 2000–2021, English language, with precise statistical data. Exclusion: narrative reviews or single-study syntheses. PRISMA methodology was used to extract and appraise data (Monteleone et al., 2022). | This is a narrative review that critically evaluates studies and clinical trials assessing the effects of combined psychotherapy and pharmacological treatments for EDs. Methodologically, the paper synthesizes findings from prior RCTs, systematic reviews, and real-world observational studies. It compares the efficacy of integrated approaches against standalone modalities across various ED populations. No formal meta-analytical statistical method was used (Reas & Grilo, 2020). |
| Sample/Setting
The number and characteristics of patients, attrition rate, etc. |
A total of 12 clinical studies with sample sizes ranging from 8 to 95 participants each. All subjects were adults diagnosed with BED or BN, recruited from outpatient or specialty eating disorder clinics. Some trials included participants with comorbid obesity or metabolic syndrome. Attrition rates varied across studies, generally between 10–30%. Settings included endocrinology and psychiatric clinics (Aoun et al., 2024).
|
The meta-analysis included 10 studies with a combined total of 1,250 participants. Of these, seven studies focused on Post-Traumatic Stress Disorder (PTSD). The settings varied across studies but primarily involved clinical environments where CBT interventions were administered. | Aggregated data from over 150,000 participants derived from previous large-scale meta-analyses, including adolescent and adult patients with various EDs. Settings included outpatient, inpatient, and specialized treatment centers globally. Demographics were balanced across sexes in some analyses, though women were predominant in most studies. Attrition was variable and accounted for in individual meta-analyses. | The narrative review incorporated data from clinical trials and observational studies, including several thousand patients with AN, BN, or BED. Participants were diverse in age and clinical background. Trials spanned inpatient and outpatient settings. Due to the nature of the review, the exact number of patients reviewed was not consolidated. Studies often focused on adult females, with fewer data for adolescents or males. |
| Major Variables Studied
List and define dependent and independent variables |
Independent variables: Type and dosage of GLP-1 receptor agonist (liraglutide, semaglutide). Dependent variables: Frequency of binge-eating episodes, weight change, glycemic control, psychiatric symptoms. | Independent Variable: Implementation of CBT interventions.
Dependent Variables: Severity of target disorder symptoms (e.g., PTSD, generalized anxiety), levels of depression, and other related psychological outcomes. |
Independent variables: Treatment modality (CBT, IPT, DBT, pharmacotherapy, combined therapies). Dependent variables: ED symptom remission, weight restoration (for AN), relapse rates, psychiatric symptom reduction. | Independent variable: Treatment approach (psychotherapy, medication, or combined). Dependent variables: Symptom reduction, relapse prevention, weight stabilization, and treatment engagement (Reas & Grilo, 2020). |
| Measurement
Identify primary statistics used to answer clinical questions (You need to list the actual tests done). |
Clinical outcomes were measured using standardized psychiatric scales such as EDE-Q and physical health metrics like BMI, fasting glucose, and HbA1c. Tools varied by study but consistently included validated ED symptom inventories. | Various standardized assessment tools were utilized across the included studies to measure anxiety and depression symptoms. Statistical analyses included calculating Hedges’ g to determine effect sizes, assessments of heterogeneity, and evaluations for publication bias (Kim et al., 2023). | Utilized outcome data from each meta-analysis, including remission percentages, effect sizes (Cohen’s d, OR), and clinical scales (EDE, YBC-EDS). Data included diagnostic criteria adherence and structured interview results. | Measurement tools included standardized psychiatric rating scales like EDE-Q, CGI-I, and BDI-II. Medication efficacy was often gauged through symptom frequency reduction, dropout rates, and patient-reported outcome measures (PROMs). |
| Data Analysis Statistical or
Qualitative findings
(You must enter the actual numbers determined by the statistical tests or qualitative data). |
Although no pooled statistical analysis was conducted, individual studies reported reductions in binge frequency (25–60%), moderate weight loss (5–8 kg), and improvement in metabolic markers. Psychiatric symptom improvement was reported inconsistently. | The meta-analysis revealed CBT’s small but statistically significant effect on target disorder symptoms (Hedges’ g = 0.24, p < 0.05). The impact on depression symptoms was more minor and not statistically significant (Hedges’ g = 0.15, p = n.s.). When isolating studies on PTSD, the effect size was further reduced (Hedges’ g = 0.14, p < 0.05). Low heterogeneity was observed in most analyses, and no evidence of publication bias was detected (Bhattacharya et al., 2022). | The meta-review found that CBT had the most consistent and robust outcomes across all Eds. | The review found that combined therapy outperformed standalone approaches for BED and BN. Medications (especially SSRIs and topiramate) were less effective alone. AN treatment favored psychotherapy, as pharmacologic interventions showed negligible benefits. Quantitative estimates varied by disorder. |
| Findings and Recommendations
General findings and recommendations of the research |
GLP-1 agonists represent a promising new direction for the pharmacologic treatment of BED and BN. Authors recommend larger RCTs with psychiatric monitoring, especially regarding long-term safety and effects on mood, cognition, and ED behaviors. | The findings suggest that the placebo-controlled effects of CBT for anxiety-related disorders, particularly PTSD, are more minor in recent studies compared to earlier meta-analyses. The authors recommend further research to explore the factors contributing to these reduced effect sizes and to assess the efficacy of CBT across a broader range of anxiety-related disorders beyond PTSD. | Strong support for CBT as a first-line intervention across EDs. Combined therapies are recommended for BN and BED, emphasized personalization based on severity and comorbidities, and advocated for global dissemination of best practices (Monteleone et al., 2022). | The combination of psychotherapy and medication enhances treatment outcomes for BED and BN. It is less promising for AN. The authors recommend integrated care models where psychotherapists and prescribers collaborate closely (Reas & Grilo, 2020). |
| Appraisal and Study Quality
Describe the general worth of this research to practice.
What are the strengths and limitations of the study?
What risks are associated with implementing the suggested practices or processes detailed in the research?
What is the feasibility of use in your practice? |
Strengths: Innovative treatment direction, bridges endocrinology, and psychiatry. Limitations: early-phase trials, small samples, lack of long-term follow-up. Implementation risks: unknown psychological side effects.
Feasibility: promising but needs clinical guidelines. |
The meta-analysis is methodologically robust, adhering to PRISMA guidelines and focusing on RCTs with placebo controls, enhancing the findings’ reliability. Strengths include the systematic approach and the focus on recent literature. Limitations involve the predominance of PTSD studies, which may not generalize to all anxiety-related disorders, and the relatively small number of included studies. The reduced effect sizes observed may impact the perceived efficacy of CBT, suggesting a need for ongoing evaluation and potential adaptation of CBT protocols. Implementing CBT remains feasible in clinical practice, but clinicians should be aware of the modest effect sizes reported in recent studies. | Strengths: Comprehensive synthesis informs global clinical practice. Limitations: methodological heterogeneity, underrepresentation of low-income countries. Feasibility: high in structured treatment centers.
Risks: improper generalization without local adaptation. |
Strengths: real-world applicability, supports integrated care.
Limitations: narrative style, lacks systematic meta-analytic structure. Feasibility: moderate to high in collaborative practice settings. Risks: overreliance on medications in AN. |
|
Key findings
|
GLP-1 agonists may reduce binge episodes, promote weight loss, and improve glycemic control in BED and BN. |
Recent placebo-controlled trials indicate that CBT has a small but significant effect on reducing symptoms of anxiety-related disorders, with exceptionally modest effects observed in PTSD populations (Bhattacharya et al., 2022). | CBT remains the gold standard; pharmacotherapy is effective mainly for BED/BN and has a limited role in AN. Personalized treatment is needed (Chand et al., 2023). | Combined treatment shows superior results in BED and BN; pharmacotherapy alone is insufficient. Therapy alone is preferred in AN. |
|
Outcomes
|
Reduced bingeing behavior, improved metabolic markers, and potential for multimodal therapy integration in ED care. | The meta-analysis highlights the need for continued research into the efficacy of CBT for various anxiety-related disorders and suggests potential reconsideration of treatment approaches to enhance therapeutic outcomes. | Enhanced remission, reduced relapse, better adherence to therapy. Supports multi-therapy models in clinical ED treatment. | Better patient engagement, symptom management, and reduced dropout in integrated models for BED/BN. |
| General Notes/Comments |
A novel and potentially transformative pharmacologic option, mental health safety monitoring is crucial.
|
This study provides valuable insights into the current state of CBT efficacy for anxiety-related disorders, emphasizing the importance of ongoing research and adaptation of therapeutic strategies to optimize patient outcomes. | Meta-review serves as a treatment map and highlights the need for global ED care access and evidence-based training. | A practical guide to combining medication and psychotherapy; caution needed in generalizing results across ED types. |
Part 3B: Critical Appraisal of Research
The four high-level studies conducted have revealed that the best practice involves supplementing pharmacologic treatment with CBT, either GLP-1 receptor agonist or SSRI, for individuals with BED or BN. This strategy is useful in providing a complete approach to the patient because it tackles both psychological and physical manifestations of the illness.
General Worth of Research to Practice
This research holds significant clinical value as it informs modern, patient-centered treatment protocols for BED and BN. As a practical matter, this investigation has clinical utility because it advances current and evidence-based approaches to treating BED and BN. Monteleone et al. (2022) present a systematic review of studies that support the recommendation of CBT as the initial treatment modality in psychotherapy. Reas and Grilo (2020) propose using mixed treatment approaches to enhance clients’ compliance, prevent relapse, and improve the outcome. GLP-1 receptor agonists are well discussed by Aoun et al. (2024) as potential novel pharmacological interventions with extra metabolic advantages. These studies provide a practical methodology for developing combined treatment strategies in real-life practices.
Strengths and Limitations of the Studies
A significant strength of the studies is their reliance on high-quality evidence. Three of the four articles are systematic reviews or meta-analyses, providing level-I evidence. Most studies adhere to PRISMA guidelines and use validated outcome measures. They involved large sample sizes, thereby giving more credence to their findings. However, some limitations are noted. For instance, many of the studies by Aoun et al. (2024) had small pilot trials and no long-term data follow-up; thus, the findings cannot be generalized. Preventing adverse outcomes, therefore, requires an ethical prescription and continuous checks.
Risks Associated with Implementation
There are risks some risks associated with the integrated model. GLP-1 receptor agonists and other pharmacologic treatments have the potential to have unknown long-term psychiatric side effects, for instance, mood swings or cognitive impairment (Aoun et al., 2024). One of the potential issues is that of overmedicalizing treatment in patients who can be managed with a lot of psychotherapy. Reas and Grilo (2020) noted that it is best not to rely on medications alone, especially in the management of disorders such as anorexia nervosa, where the outcome is not very impressive. The prescribers must practice ethically and ensure that their patients are monitored constantly to reduce harm.
Feasibility of Use in Practice
This integrated solution is highly conceivable, particularly in an enthused and possibly interdisciplinary environment. CBT is already used in most clinical settings, and GLP-1 receptor agonists are FDA-approved for metabolic disorders; they may be prescribed off-label with a psychiatrist’s supervision (Bhattacharya et al., 2022). This approach is in sync with the recent emphasis on individualized medicine and team practice, thus explaining why this would easily fit both the outpatient and specialty settings.
Conclusion
Considering the data incorporated in these studies, a strong and specific recommendation can be made to use CBT jointly with pharmacotherapy to treat BED and BN. This is because the current best practice model of care is clinically beneficial, feasible, and adaptable in addressing the needs of high-risk patients and other adult patients.
References
Aoun, L., Almardini, S., Saliba, F., Haddadin, F., Mourad, O., Jdaidani, J., Morcos, Z., Saidi, I. A., Sanayeh, E. B., Saliba, S., Almardini, M., & Zaidan, J. (2024). GLP-1 receptor agonists: A novel pharmacotherapy for binge eating (Binge eating disorder and bulimia nervosa)? A systematic review. Journal of Clinical & Translational Endocrinology, 35, 100333. https://doi.org/10.1016/j.jcte.2024.100333
Bhattacharya, S., Goicoechea, C., Heshmati, S., Carpenter, J. K., & Hofmann, S. G. (2022). Efficacy of cognitive behavioral therapy for anxiety-related disorders: A meta-analysis of recent literature. Current Psychiatry Reports, 25(1), 19–30. https://doi.org/10.1007/s11920-022-01402-8
Chand, S. P., Kuckel, D. P., & Huecker, M. R. (2023, May 23). Cognitive behavior therapy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470241/
Kim, J., Aryee, L. M. D., Bang, H., Prajogo, S., Choi, Y. K., Hoch, J. S., & Prado, E. L. (2023). Effectiveness of digital mental health tools to reduce depressive and anxiety symptoms in Low- and Middle-Income Countries: Systematic review and Meta-analysis. JMIR Mental Health, 10, e43066. https://doi.org/10.2196/43066
Monteleone, A. M., Pellegrino, F., Croatto, G., Carfagno, M., Hilbert, A., Treasure, J., Wade, T., Bulik, C. M., Zipfel, S., Hay, P., Schmidt, U., Castellini, G., Favaro, A., Fernandez-Aranda, F., Shin, J. I., Voderholzer, U., Ricca, V., Moretti, D., Busatta, D., . . . Solmi, M. (2022). Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neuroscience & Biobehavioral Reviews, 142, 104857. https://doi.org/10.1016/j.neubiorev.2022.104857
Reas, D. L., & Grilo, C. M. (2020). Psychotherapy and medications for eating disorders: Better together? Clinical Therapeutics, 43(1). https://doi.org/10.1016/j.clinthera.2020.10.006
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Evidence-Based Project, Part 3 – Critical Appraisal of Research
Use this document to complete the evaluation table requirement of the Module 4 Assessment, Evidence-Based Project, Part 3A: Critical Appraisal of Research
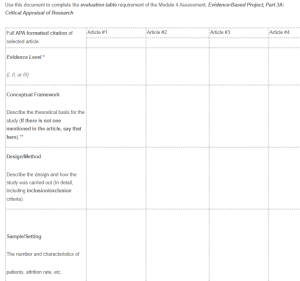
Critical Appraisal of Research
| Full APA formatted citation of selected article. | Article #1 | Article #2 | Article #3 | Article #4 |
| Evidence Level *
(I, II, or III) |
||||
| Conceptual Framework
Describe the theoretical basis for the study (If there is not one mentioned in the article, say that here).** |
||||
| Design/Method
Describe the design and how the study was carried out (In detail, including inclusion/exclusion criteria). |
||||
| Sample/Setting
The number and characteristics of patients, attrition rate, etc. |
|
|||
| Major Variables Studied
List and define dependent and independent variables |
|
|||
| Measurement
Identify primary statistics used to answer clinical questions (You need to list the actual tests done). |
||||
| Data Analysis Statistical or
Qualitative findings (You need to enter the actual numbers determined by the statistical tests or qualitative data). |
||||
| Findings and Recommendations
General findings and recommendations of the research |
||||
| Appraisal and Study Quality
Describe the general worth of this research to practice. What are the strengths and limitations of study? What are the risks associated with implementation of the suggested practices or processes detailed in the research? What is the feasibility of use in your practice? |
||||
| Key findings | ||||
| Outcomes | ||||
| General Notes/Comments |
Refer to the Johns Hopkins Evidence-Based Practice Model for Nursing and HealthcarePprofessionals, Hierarchy of Evidence Guide on the following page
**Note on Conceptual Framework
- The following information is from Walden academic guides which helps explain conceptual frameworks and the reasons they are used in research. Here is the link https://academicguides.waldenu.edu/library/conceptualframework
- Researchers create theoretical and conceptual frameworks that include a philosophical and methodological model to help design their work. A formal theory provides context for the outcome of the events conducted in the research. The data collection and analysis are also based on the theoretical and conceptual framework.
- As stated by Grant and Osanloo (2014), “Without a theoretical framework, the structure and vision for a study is unclear, much like a house that cannot be constructed without a blueprint. By contrast, a research plan that contains a theoretical framework allows the dissertation study to be strong and structured with an organized flow from one chapter to the next.”
- Theoretical and conceptual frameworks provide evidence of academic standards and procedure. They also offer an explanation of why the study is pertinent and how the researcher expects to fill the gap in the literature.
- Literature does not always clearly delineate between a theoretical or conceptual framework. With that being said, there are slight differences between the two.

