Ethical Dilemma – End-of-Life Care
Hello. Welcome to today’s presentation on ethical dilemmas.
This presentation aims to explore ethical dilemmas in advanced nursing practice, a critical aspect of healthcare delivery. We will examine the role of advanced practice nurses in addressing ethical issues, describe a specific ethical dilemma scenario, and analyze relevant ethical principles and the ANA Code of Ethics. The presentation will provide recommendations for resolving such dilemmas, aiming to enhance ethical decision-making skills and promote patient-centered, ethical care delivery. By addressing these topics, we can better understand the complexities of ethical challenges in healthcare and develop strategies to navigate them effectively (Rushton, 2023).
Advanced practice nurses play a crucial role in addressing ethical dilemmas in healthcare. They advocate for patient rights and autonomy, ensuring that patient preferences are respected and protected (American Nurses Association [ANA], 2015). These nurses facilitate ethical decision-making processes within healthcare teams, bringing their expertise to complex situations. They also educate staff on ethical principles and guidelines, enhancing the overall ethical awareness in healthcare settings. Additionally, advanced practice nurses contribute to developing and implementing ethical policies and procedures, participate in ethics committees and consultations, and conduct research on ethical issues in healthcare. Their multifaceted involvement helps create a more ethically conscious healthcare environment (Caro-Alonso et al., 2023).
Classic examples of ethical dilemmas can be exemplified in end-of-life care. For instance, a terminally ill cancer patient decides to refuse further treatment while their family insists on continuing aggressive interventions. The patient’s advance directive is unclear, leaving healthcare providers uncertain about the best course of action. Nurses are caught between respecting the patient’s wishes and addressing the family’s concerns. The attending physician considers the family’s request over the patient’s expressed desires, and hospital administration worries about potential legal implications. This scenario highlights the complex interplay of patient autonomy, family dynamics, healthcare provider responsibilities, and institutional concerns in end-of-life care decisions (National Comprehensive Cancer Network [NCCN], n.d.).
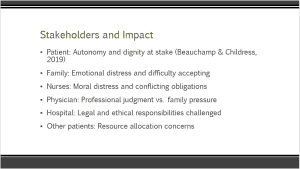
This ethical dilemma impacts various stakeholders. The patient’s autonomy and dignity are at stake, as their right to make decisions about their own care is being challenged (Beauchamp & Childress, 2019). The family experiences emotional distress and difficulty accepting the situation, which can lead to conflicts with the healthcare team. Nurses face moral distress and conflicting obligations between respecting the patient’s wishes and addressing family concerns. Further, the physician must balance professional judgment with family pressure, potentially compromising their ethical obligations. Additionally, the hospital faces challenges to its legal and ethical responsibilities, particularly in terms of respecting patient autonomy and managing potential legal risks. Other patients may be affected by resource allocation concerns, especially if aggressive treatments are continued against the patient’s wishes (Rushton, 2023).
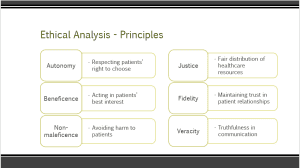
This ethical dilemma involves several conflicting ethical principles. Autonomy emphasizes respecting the patient’s right to choose their care, which is being challenged in this scenario. Beneficence calls for acting in the patient’s best interest, which may be interpreted differently by various stakeholders. Non-maleficence requires avoiding harm to the patient, which could be violated by either continuing or withdrawing treatment. Justice considers fair distribution of healthcare resources, which is particularly relevant if aggressive treatments are continued. Fidelity involves maintaining trust in patient relationships, which could be compromised if the patient’s wishes are not respected. Lastly, veracity emphasizes truthfulness in communication with all parties involved, which is essential for informed decision-making (Beauchamp & Childress, 2019).
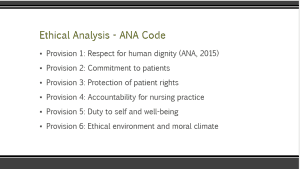
Several provisions of the ANA Code of Ethics apply to this dilemma. Provision 1 emphasizes respect for human dignity, which is central to the patient’s right to make decisions about their care (American Nurses Association [ANA], 2015). Provision 2 focuses on commitment to patients, requiring nurses to prioritize the patient’s interests. Provision 3 addresses the protection of patient rights, including the right to refuse treatment. Provision 4 highlights accountability for nursing practice, which is relevant when nurses face conflicting obligations. Provision 5 considers the nurse’s duty to self and well-being particularly important in situations causing moral distress. Provision 6 emphasizes the importance of maintaining an ethical environment and moral climate, which is crucial for addressing complex ethical dilemmas effectively (ANA, 2015).
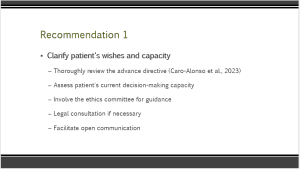
The first recommendation is to clarify the patient’s wishes and decision-making capacity. This involves thoroughly reviewing the advance directive, assessing the patient’s current capacity to make decisions, and clearly documenting their expressed preferences (Caro-Alonso et al., 2023). Involving the ethics committee for guidance can provide valuable insights and support in navigating this complex situation. Additionally, legal consultation may be necessary to ensure compliance with relevant laws and regulations. Further, facilitating open communication among all parties is crucial to ensure everyone’s perspectives are heard and understood. This approach helps to respect the patient’s autonomy while also addressing the concerns of family members and healthcare providers (NCCN, n.d.).
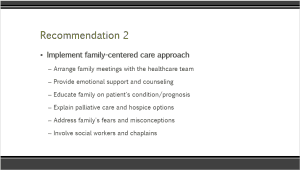
The second suggestion would be to promote family-centered care through well-planned family conferences with the health team. This extremely difficult situation for the family can be facilitated with emotional support and counseling. Preparing the family by educating them about the patient’s illness and prognosis will help in decision-making. Describing how palliative care and hospice work during the end of life might enlighten the family to realize alternative ways of approaching end-of-life care. Addressing the family’s fears and misconceptions can help to allay some of their concerns, which may, in turn, decrease conflict. Offering social workers and chaplains the opportunity to become involved with the family might provide a team approach to care, thus giving them even more support and resources during this difficult time (NCCN, n.d.).
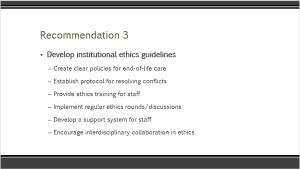
The third recommendation is the need to develop comprehensive institutional ethics guidelines. This involves making clear policies for end-of-life care that will provide a framework for decision-making in complicated cases. Essentially, there will be the need to set up a protocol for conflict resolution, which can go a long way in solving disagreements in this respect. Providing ethics training for all staff enhances overall ethical awareness and decision-making skills. Also, implementing regular ethics rounds or discussions can foster ongoing dialogue about ethical issues. Further, developing a support system for staff experiencing moral distress is crucial for maintaining their well-being and job satisfaction. Lastly, encouraging interdisciplinary collaboration in ethics can lead to more comprehensive and balanced approaches to ethical dilemmas (Rushton, 2023).
In conclusion, advanced practice nurses play a crucial role in resolving ethical dilemmas in healthcare, particularly in end-of-life care decisions, which often present challenging ethical situations. These dilemmas impact multiple stakeholders, including patients, families, healthcare providers, and institutions. Ethical principles and the ANA Code of Ethics provide essential guidance for nursing practice in navigating these complex situations. Key recommendations include clarifying patient wishes, supporting families through a family-centered care approach, and developing comprehensive institutional ethics guidelines and support systems. By implementing these strategies, healthcare organizations can enhance their ability to address ethical dilemmas effectively, ultimately improving patient care and supporting healthcare providers in their ethical decision-making processes (Rushton, 2023; ANA, 2015).
American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. American Nurses Association. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/coe-view-only/
Beauchamp, T., & Childress, J. (2019). Principles of biomedical ethics: Marking its fortieth anniversary. The American Journal of Bioethics, 19(11), 9–12. https://doi.org/10.1080/15265161.2019.1665402
Caro-Alonso, P. Á., Rodríguez-Martín, B., Rodríguez-Almagro, J., Chimpén-López, C., Romero-Blanco, C., Casado Naranjo, I., Hernández-Martínez, A., & López-Espuela, F. (2023). Nurses’ perceptions of ethical conflicts when caring for patients with COVID-19. International Journal of Environmental Research and Public Health, 20(6), 4763. https://doi.org/10.3390/ijerph20064763
National Comprehensive Cancer Network. (n.d.). Treatment by cancer type. NCCN. https://www.nccn.org/guidelines/category_1
Rushton, C. H. (2023). Transforming moral suffering by cultivating moral resilience and ethical practice. American Journal of Critical Care, 32(4), 238–248. https://doi.org/10.4037/ajcc2023207
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Ethical Dilemma – End-of-Life Care
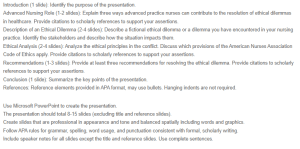
Introduction (1 slide): Identify the purpose of the presentation.
Advanced Nursing Role (1-2 slides): Explain three ways advanced practice nurses can contribute to the resolution of ethical dilemmas in healthcare. Provide citations to scholarly references to support your assertions.
Description of an Ethical Dilemma (2-4 slides): Describe a fictional ethical dilemma or a dilemma you have encountered in your nursing practice. Identify the stakeholders and describe how the situation impacts them.
Ethical Analysis (2-4 slides): Analyze the ethical principles in the conflict. Discuss which provisions of the American Nurses Association Code of Ethics apply. Provide citations to scholarly references to support your assertions.
Recommendations (1-3 slides): Provide at least three recommendations for resolving the ethical dilemma. Provide citations to scholarly references to support your assertions.
Conclusion (1 slide): Summarize the key points of the presentation.
References: Reference elements provided in APA format, may use bullets. Hanging indents are not required.
Use Microsoft PowerPoint to create the presentation.
The presentation should total 8-15 slides (excluding title and reference slides).
Create slides that are professional in appearance and tone and balanced spatially including words and graphics.
Follow APA rules for grammar, spelling, word usage, and punctuation consistent with formal, scholarly writing.
Include speaker notes for all slides except the title and reference slides. Use complete sentences.