Ethical and Legal Implications of Prescribing Drugs
Nurses face various ethical issues in their practice. In this scenario, the patient is admitted to the intensive care unit after a stroke and put on a ventilator. The patient’s wife opines that treatment should be withdrawn to relieve her husband’s suffering. On the other side, the patient’s daughter asserts that evidence-based treatment that would improve his condition should not be withdrawn.
The Ethical and Legal Implications of the Scenario
In this scenario, the healthcare interdisciplinary team involved in the management of the patient comprises physicians, nurses, and pharmacists. Furthermore, the patient’s family is a key stakeholder. Healthcare providers face the ethical and legal implications of withholding or withdrawing treatment from the patient. The ethical principle of beneficence champions practices that benefit and improve the patient’s overall well-being (Akdeniz et al., 2021). Also, non-maleficence champions practices that don’t harm patients. Autonomy acknowledges that patients and their families are important stakeholders in the decision-making process (Akdeniz et al., 2021). However, in this context, the patient’s wife and daughter differ in opinions regarding the patient’s management. To address this ethical issue, the interdisciplinary team should evaluate the severity of the patient’s stroke, explore possible interventions, and establish a prognosis. A poor prognosis justifies treatment withdrawal. Legal provisions direct physicians and the interdisciplinary team to respect patients’ decision to withdraw or withhold treatment when they have a poor prognosis (Akdeniz et al., 2021). In addition, patients should not insist on receiving treatment that is not beneficial or predisposes them to serious health conditions such as brain damage.
Strategies to Address Disclosure and Nondisclosure
In this scenario, the interdisciplinary team members involved in managing the patient should adhere to specific statutes regarding disclosure and non-disclosure. Firstly, the interdisciplinary team members should not disclose personal health information and other details provided by the patient’s family. Chapter 456, Section 57 of the Florida Statutes, directs healthcare practitioners to maintain the privacy and confidentiality of patient information (FloridaSenate.gov, 2022). Written consent should be obtained from the patient (in this context, his family) before the information is disclosed to other healthcare practitioners. Furthermore, this information may be disclosed at a subpoena following legal notice (FloridaSenate.gov, 2022). Secondly, healthcare practitioners should disclose information associated with medical negligence, adverse effects, or medication errors (FloridaSenate.gov, 2022). This requirement facilitates legal proceedings and may necessitate the disclosure of personal health information. Furthermore, this disclosure is key to the success of administrative proceedings. The disclosure policy aims to improve the quality of healthcare services and avert preventable medical errors.
Strategies for Decision-Making
In this context, I would embrace evidence-based practice and the principles of honesty and trust to make decisions. Regarding evidence-based practice, I would collaborate with other members of the interdisciplinary team to determine the severity and prognosis of the patient. I would use these findings to decide on continued intensive care for the patient or withdrawal of treatment as requested by the patient’s wife. I would use open communication to inform the patient’s wife and daughter about the evidence-based findings and seek their approval of the decision. For instance, if the massive stroke is likely to cause significant brain damage and cognitive impairment, increase morbidity, and lower the patient’s quality of life, I will engage the patient’s family and educate them on the merits of treatment withdrawal. The principles of honesty and trustworthiness will enable me to disclose any error committed during patient care. This is harmonious with the provisions of Chapter 456, Section 57 of the Florida Statutes (FloridaSenate.gov, 2022). As such, I would inform the unit manager about the error and file a report detailing the type of error, potential causes, and possible strategies for averting the error in my future practice.
Process of Writing Prescriptions
Six sequential steps are used to write a prescription. The first step entails patient assessment to determine individualized needs or problems (Wyles et al., 2020). The second step entails determining the objective or goal of treatment. The next step entails selecting the best evidence-based medicine. The selection should be rational and relevant to the patient’s needs (Wyles et al., 2020). Furthermore, the treatment plan should be cost-effective. The fourth step entails the implementation of the treatment plan (Wyles et al., 2020). Both pharmacological and non-pharmaceutical approaches should be implemented. The fifth step entails patient education regarding medication adherence and potential adverse effects (Wyles et al., 2020). Finally, the sixth step entails evaluation to establish the effectiveness of the treatment plan.
Strategies to Minimize Medication Errors
Nurses and other interdisciplinary team members should embrace various strategies to minimize medication errors. Firstly, they should embrace technology. In this context, technology such as barcodes, electronic health record (EHR) systems, and smart infusion pumps (SIP) will reduce medication errors (Michalek & Carson, 2020; Naidu & Alicia, 2019). EHR systems improve documentation, and barcodes facilitate the elimination of errors associated with patient identification, whereas SIP eliminates errors related to dosing. Secondly, they should standardize their tasks by formulating policies and standardized procedures. Thirdly, they should improve their workflow by limiting and avoiding distractions and adopting collaborative strategies such as double-checking (Koyama et al., 2020). Lastly, they should embrace open communication and conduct regular performance evaluations.
References
Akdeniz, M., Yardımcı, B., & Kavukcu, E. (2021). Ethical considerations at end-of-life care. SAGE Open Medicine, 9, 205031212110009. https://doi.org/10.1177/20503121211000918
FloridaSenate.gov. (2022). 2018 Florida Statutes. https://www.flsenate.gov/Laws/Statutes/2018/0456.057
Koyama, A. K., Maddox, C. S. S., Li, L., Bucknall, T., & Westbrook, J. I. (2020). Effectiveness of double checking to reduce medication administration errors: A systematic review. BMJ Quality and Safety, 29(7), 595–603. https://doi.org/10.1136/bmjqs-2019-009552
Michalek, C., & Carson, S. L. (2020). Implementing barcode medication administration and smart infusion pumps is just the beginning of the safety journey to prevent administration errors. Farmacia Hospitalaria, 44(3), 114–121. https://doi.org/10.7399/fh.11410
Naidu, M., & Alicia, Y. L. Y. (2019). Impact of Bar-Code Medication Administration and Electronic Medication Administration Record System in Clinical Practice for an Effective Medication Administration Process. Health, 11(05), 511–526. https://doi.org/10.4236/health.2019.115044
Wyles, C. C., Hevesi, M., Ubl, D. S., Habermann, E. B., Gazelka, H. M., Trousdale, R. T., & Mabry, T. M. (2020). Implementation of procedure-specific opioid guidelines: a readily employable strategy to improve consistency and decrease excessive prescribing following orthopaedic surgery. JBJS Open Access, 5(1). https://doi.org/10.2106/JBJS.OA.19.00050
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
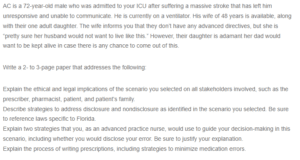
AC is a 72-year-old male who was admitted to your ICU after suffering a massive stroke that has left him unresponsive and unable to communicate. He is currently on a ventilator. His wife of 48 years is available, along with their one adult daughter. The wife informs you that they don’t have any advanced directives, but she is “pretty sure her husband would not want to live like this.” However, their daughter is adamant her dad would want to be kept alive in case there is any chance to come out of this.
Ethical and Legal Implications of Prescribing Drugs
Write a 2- to 3-page paper that addresses the following:
Explain the ethical and legal implications of the scenario you selected on all stakeholders involved, such as the prescriber, pharmacist, patient, and patient’s family.
Describe strategies to address disclosure and nondisclosure as identified in the scenario you selected. Be sure to reference laws specific to Florida.
Explain two strategies that you, as an advanced practice nurse, would use to guide your decision-making in this scenario, including whether you would disclose your error. Be sure to justify your explanation.
Explain the process of writing prescriptions, including strategies to minimize medication errors.

