Discussion – Culture of Safety in Healthcare Settings
In my experience working in a healthcare setting, there was a transparent culture of safety rather than a blame culture. During interdisciplinary bedside rounds, emphasis was placed on collaboration and open communication to enhance patient care, as highlighted by Braun et al. (2020). The structured rounds promoted information sharing and joint decision-making, leading to a supportive environment where the focus was on improving care rather than assigning blame. This approach allowed for transparent communication among team members, which not only improved patient outcomes but also fostered trust and mutual respect within the team.
Incident Reporting in Clinical Practice
No fear arose from completing any of the incident reports since the culture was reporting to improve, not in light of penalties. The organization continued to stress that incident reports were useful for improving deficiencies as a method for holding employees accountable, as it stressed safety over retribution. The cultured attitude provided favorable circumstances in which staff could report incidents and near misses during work without fearing that something would be done against them if they were involved in the incidents.
Incentivizing Incident Reporting in Healthcare
To encourage enhanced staff reporting, healthcare organizations should use self-reporting to improve safety rather than punish staff for mistakes. One of the plans is to use incentive programs that pin the value of reporting mistakes and servlets, coupled with ongoing education on the importance of incidence reports for enhancing patient outcomes (Mistri et al., 2023). Moreover, showing the staff how their reports contribute to change in the organization’s safety status can also help encourage more people to report their observations in the future. The culture of incident reporting can change from a negative connotation of blame assignment to that of positive learning and process improvement.
References
Braun, B. I., Chitavi, S. O., Suzuki, H., Soyemi, C. A., & Puig-Asensio, M. (2020). Culture of safety: Impact on improvement in infection prevention process and outcomes. Current Infectious Disease Reports, 22(12). https://doi.org/10.1007/s11908-020-00741-y
Mistri, I. U., Badge, A., Shahu, S., Mistri, I. U., Badge, A., & Shahu, S. (2023). Enhancing patient safety culture in hospitals. Cureus, 15(12), 1–7. https://doi.org/10.7759/cureus.51159
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Discussion
Purpose
The purpose of this discussion is to analyze topics related to the application of quality and safety practices in clinical practice.
Course Outcomes
This assignment enables the student to meet the following course outcomes:
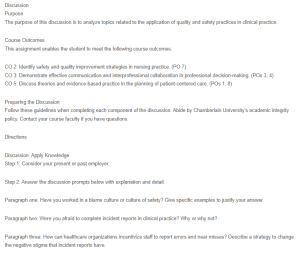
Discussion – Culture of Safety in Healthcare Settings
CO 2: Identify safety and quality improvement strategies in nursing practice. (PO 7)
CO 3: Demonstrate effective communication and interprofessional collaboration in professional decision-making. (POs 3, 4)
CO 5: Discuss theories and evidence-based practice in the planning of patient-centered care. (POs 1, 8)
Preparing the Discussion
Follow these guidelines when completing each component of the discussion. Abide by Chamberlain University’s academic integrity policy. Contact your course faculty if you have questions.
Directions
Discussion: Apply Knowledge
Step 1: Consider your present or past employer.
Step 2: Answer the discussion prompts below with explanation and detail.
Paragraph one: Have you worked in a blame culture or culture of safety? Give specific examples to justify your answer.
Paragraph two: Were you afraid to complete incident reports in clinical practice? Why or why not?
Paragraph three: How can healthcare organizations incentivize staff to report errors and near misses? Describe a strategy to change the negative stigma that incident reports have.
References: Provide complete references for all citations.
Posts should meet the following criteria:
Integrate Evidence: Cite at least two sources of evidence in weekly posts.
Integrate evidence from assigned reading(s) OR lesson.
Integrate evidence from at least one outside scholarly source as directed in the discussion directions.
Integrate evidence that supports the discussion.
Cite all scholarly sources, reading(s), OR lessons in an in-text citation within the post and include a complete reference at the bottom of the post.
Use sources no more than five years old unless they are historical references.
Engage in Meaningful Dialogue: Engage with peers and/or faculty by asking questions and offering new insights, applications, perspectives, information, or implications for practice.
Respond to a peer and/or faculty post.
Provide additional information or clarification in the reply post.
Add depth to the discussion.
Communicate Professionally: Communicate professionally on all posts.
Communicate clearly and concisely.
Communicate respectfully, civilly, and caringly.
Communicate with minimal errors in English grammar, spelling, syntax, and punctuation.
Participate: Participate during the assigned week. You are expected to meet the minimum participation requirement described below. You will receive a 10% point deduction in a graded discussion if you do not post at least two (2) times on at least two (2) different days during the assigned week.
Post in the discussion at least two times.
Post in the discussion on two different days.

