Concept Map and Narrative – Evidence-Based Nursing Interventions for a Diabetic Patient
Concept Map
Concept Map
Narrative
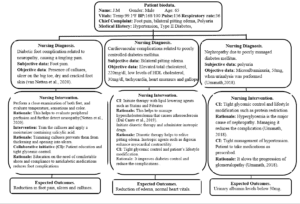
This paper describes a concept map with evidence-based nursing interventions for a diabetic patient with various complications. The complications presented are diabetic nephropathy, cardiovascular complications, and diabetic foot problems. The concept map provides various nursing interventions and their rationale. It also provides different collaborative interventions between the nurse and the patient. Furthermore, the concept map contains the expected patient outcomes after the interventions are implemented. This paper justifies the evidence in the concept map, gives additional evidence, and explains how interprofessional collaboration can help achieve quality outcomes.
The diagnosis of Mr. J.M. was made based on presenting complaints, physical examination, and laboratory data. The patient complains of pain in the foot. Examination reveals calluses, an ulcer on the big toe, and dry, cracked skin. Diabetic foot complications usually result from nerve damage. It presents with burning pain in the foot, decreased sensitivity to stimuli, calluses, and skin dryness (van Netten et al., 2020). Diabetic nephropathy presents with microalbuminuria or macroalbuminuria (Umanath & Lewis, 2018). Microalbuminuria occurs when albumin levels in the urine range between 30 to 300 milligrams (mg) per day (Thamrin et al., 2019). Macroalbuminuria refers to albumin levels greater than 300 milligrams per day. J. M’s albumin levels are 50 mg, a manifestation of microalbuminuria.
Diabetic cardiovascular disease presents with atherosclerosis, heart failure, and arrhythmias. The presence of hypercholesterolemia indicates the presence of atherosclerosis. J.M. has pitting edema, an indication of the possibility of heart failure that resulted from poorly managed diabetes. However, pitting edema can also be observed in conditions such as deep venous thrombosis, chronic lung disease, and liver disease (Dal Canto et al., 2019). Medications that are indicated in heart failure successfully reduce pitting edema caused by diabetic cardiovascular complications.
The concept map provides the nursing interventions in the management of the complications of diabetes. The interventions can either be individualized or collaborative. The nurse can perform individualized interventions without the involvement of the other healthcare practitioners. An individualized intervention included in the concept map is the evaluation of Mr. J. M’s feet’ temperature, color, and response to stimuli. Diabetic nerve damage can reduce the ability to sense stimuli such as heat or cold (van Netten et al., 2020). This can lead to un-noticed foot injuries. Diabetes also causes a decrease in peripheral perfusion. This can present as a decrease in the temperature of feet. Diabetes presents with drying, peeling, or cracking of the foot’s skin. Therefore, the individualized interventions included in the concept map are relevant.
Interprofessional collaboration between various healthcare workers, dieticians, and patients is important in managing diabetes. The healthcare providers that form part of this collaborative approach are nurses, pharmacists, physicians, and orthopedic surgeons (Szafran et al., 2019). The concept map indicates collaborative interventions. The collaborative interventions included in the concept map entail patient education and medication administration. Dieticians educate the patients on the importance of a healthy diet, such as fresh vegetables and fruits. Nurses take part in tight glycemic control by administering medications in the right doses and intervals. They also educate patients on the importance of lifestyle modification. Such modifications include regular exercise and reducing alcohol and cigarette smoking.
Pharmacists can take part in the collaborative approach by providing the patient with appropriate medication information. They should educate the patient on how compliance is essential in tight glycemic control. They provide education on how to use medications such as subcutaneous administration of insulin (Ray et al., 2020). Orthopedic surgeons explain the rationale of amputation to patients with long-term uncontrolled diabetic foot problems. Physicians ensure that individual patients get the most appropriate treatment regimen (Szafran et al., 2019). In addition to these professional collaborative efforts, patients, mostly outpatients, must comply with the instructions given. This strategy, which can involve follow-ups at patient’s residences, has not been included in the concept map.
Poorly managed diabetes presents with microvascular and macrovascular complications. Microvascular complications include diabetic retinopathy, neuropathy, and nephropathy. Macrovascular complications include peripheral vascular, cerebrovascular, and cardiovascular diseases. Interprofessional strategies such as patient education and medication administration provide the patient with comprehensive care. A concept map helps organize ideas logically and organize health care plan decisions.
References
Dal Canto, E., Ceriello, A., Rydén, L., Ferrini, M., Hansen, T. B., Schnell, O., Standl, E., & Beulens, J. W. J. (2019). Diabetes as a cardiovascular risk factor: An overview of global trends of macro and microvascular complications. European Journal of Preventive Cardiology, 26(2_suppl), 25–32. https://doi.org/10.1177/2047487319878371
Ray, S., Lokken, J., Whyte, C., Baumann, A., & Oldani, M. (2020). The impact of a pharmacist-driven, collaborative practice on diabetes management in an Urban underserved population: a mixed-method assessment. Journal of Interprofessional Care, 34(1), 27–35. https://doi.org/10.1080/13561820.2019.1633289
Szafran, O., Kennett, S. L., Bell, N. R., & Torti, J. M. I. (2019). Interprofessional collaboration in diabetes care: Perceptions of family physicians practicing in or not in a primary health care team. BMC Family Practice, 20(1), 1–10. https://doi.org/10.1186/s12875-019-0932-9
Thamrin, H., Sutjahjo, A., Pranoto, A., & Soelistijo, S. A. (2019). Association of Metabolic Syndrome with Albuminuria in Diabetes Mellitus Type 2. Biomolecular and Health Science Journal, 2(2), 82. https://doi.org/10.20473/bhsj.v2i2.14964
Umanath, K., & Lewis, J. B. (2018). Update on Diabetic Nephropathy: Core Curriculum 2018. American Journal of Kidney Diseases, 71(6), 884–895. https://doi.org/10.1053/j.ajkd.2017.10.026
van Netten, J. J., Bus, S. A., Apelqvist, J., Lipsky, B. A., Hinchliffe, R. J., Game, F., Rayman, G., Lazzarini, P. A., Forsythe, R. O., Peters, E. J. G., Senneville, É., Vas, P., Monteiro-Soares, M., & Schaper, N. C. (2020). Definitions and criteria for diabetic foot disease. Diabetes/Metabolism Research and Reviews, 36(S1), 1–6. https://doi.org/10.1002/dmrr.3268
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Concept Map and Narrative – Evidence-Based Nursing Interventions for a Diabetic Patient
PART 1 of 3 Part Assignment
******************************
OVERVIEW:
Create a concept map of a chosen condition, disease, or disorder with glucose regulation or metabolic balance considerations. Write a brief narrative (2–3 pages) that explains why the evidence cited in the concept map and narrative are valuable and relevant, as well as how specific inter-professional strategies will help to improve the outcomes presented in the concept map.
Concept Map and Narrative
______________________________
CONTEXT:
The purpose of a concept map is to visualize connections between ideas, connect new ideas to previous ideas, and to organize ideas logically. Concept maps can be an extremely useful tool to help organize and plan care decisions. This is especially true in the biopsychosocial model of health, which takes into account factors beyond just the biochemical aspects of health. By utilizing a concept map, a nurse can simplify the connection between disease pathways, drug interactions, and symptoms, as well as between emotional, personality, cultural, and socioeconomic considerations that impact health.
___________________
QUESTIONS TO CONSIDER:
The assessment will be based on the case of a specific patient with a specific condition, disease, or disorder. Think about an experience you have had treating a patient with a condition, disease, or disorder that interests you.
1. What is the primary condition, disease, or disorder affecting the patient?
- a. What types of experience have you had working with patients with this condition, disease, or disorder?
- b. How does this condition, disease, or disorder typically present?
- c. What are the recommended treatment options?
ii. What, if any, characteristics of an individual patient should be kept in mind when determining a course of treatment.
2. How have you used concept maps to help plan and organize care?
- a. What are the advantages of concept maps, from your point of view?
- b. How could concept maps be more useful?
3. How can inter-professional communication and collaboration strategies assist in driving patient safety, efficiency, and quality outcomes with regard to specific clinical and biopsychosocial considerations?
- a. What inter-professional strategies do you recommend health care providers take in order to meet patient-centered safety and outcome goals?
__________
SCENARIO:
You have already learned about evidence-based practice and quality improvement initiatives in previous courses. You will use this information to guide your assessments while also implementing new concepts introduced in this course. For this assessment, you will develop a concept map and provide supporting evidence and explanations. You may use the case studies presented in the Vila Health: Concept Maps as Diagnostic Tools media, a case study from the literature or your practice that is relevant to the list of conditions below, or another relevant case study you have developed. This case study will provide you with the context for creating your concept map. You may also use the practice context from the case study or extrapolate the case study information and data into your own practice setting. Think carefully when you are selecting the case study for this assessment, as you may choose to build upon it for the second assessment as well.
Some example conditions, diseases, and disorders that are relevant to metabolic balance and glucose regulation considerations are:
- Cancer.
- Diabetes (type 2).
- HIV/AIDS.
- Hyperthyroidism.
- Hypothyroidism.
- Metabolic syndrome.
- Obesity.
- Polycystic ovary syndrome.
- Prediabetes.
- Pregnancy.
______________________________
Instructions
Develop a concept map and a short narrative that supports and further explains how the concept map is constructed. You may choose to use the Concept Map Template (in the Resources) as a starting point for your concept map, but are not required to do so. The bullet points below correspond to the grading criteria in the scoring guide. Be sure that your evidence-based plan addresses all of them. You may also want to read the Concept Map scoring guide and the Guiding Questions: Concept Map document to better understand how each grading criterion will be assessed.
Concept Map and Narrative
Part 1: Concept Map
- Develop an evidence-based concept map that illustrates a plan for achieving high-quality outcomes for a condition that has impaired glucose or metabolic imbalance as related aspects.
Part 2: Additional Evidence (Narrative)
- Justify the value and relevance of the evidence you used as the basis for your concept map.
- Analyze how inter-professional strategies applied to the concept map can lead to the achievement of desired outcomes.
- Construct a concept map and linkage to additional evidence in a way that facilitates understanding of key information and links.
- Integrate relevant sources to support assertions, correctly formatting citations and references using current APA style.
Additional Requirements
- Length of submission: Your concept map should be on a single page, if at all possible. You can submit the concept map as a separate file if you need to. Your additional evidence narrative should be 2–3 double-spaced, typed pages. Your narrative should be succinct yet substantive.
- Number of references: Cite a minimum of 3–5 sources of scholarly or professional evidence that support your concept map, decisions made regarding care, and inter-professional strategies. Resources should be no more than five years old.
- APA formatting:
- – For the concept map portion of this assessment, Resources and citations are formatted according to the current APA style. Please include references both in-text and on the reference page that follows your narrative.
- – For the narrative portion of this assessment, use the APA Paper Template linked in the Resources. An APA Template Tutorial is also provided to help you in writing and formatting your analysis. You do not need to include an abstract for this assessment.

