Childhood Trauma – Jacob Case Study
Severe adversities early in a child’s life have been implicated as a risk factor for various mental health illnesses. Childhood trauma defines any life-threatening, scary, or violent events experienced by children aged between 0 and 18 years. While a direct causal relationship is impossible to establish, there is a positive correlation between early exposure to trauma and mental health illnesses in later life. This casts the burden of trauma assessment and management as best practices to lessen the effect of these traumas. This paper reviews a case study on childhood trauma, emphasizing assessment and management.
Case Study Analysis
The case presented is of a 12-year-old male school-going child, Jacob, currently in grade six, living with his grandmother. The child is reported to be having behavioral issues that started when his sister came to live with them. He becomes angry quickly, has severe mood swings, regular anger outbursts, difficulty sleeping, is easily irritable, has edginess, and impaired concentration. His grandmother also notes that the child is below grade levels in several of his classes and reading. The child, however, seems to be talkative, social and has friends. The child has a recent diagnosis of ADHD and ODD.
Get in touch with us at eminencepapers.com. Our homework help will save you tons of time and energy required for your assignment papers.
The child’s history is significant for past childhood adversities. At 18 months, he was removed from his parents’ care by Child Protection Services and placed under his grandmother’s custody. His grandmother reported that this was because of neglect and abuse. His parents struggled with substance abuse. They were also in a violent relationship in which the child’s mother was physically abused by her husband. At that time, the child’s mother also complained that he was developing slowly and did not meet normal developmental milestones. His mother also complained that he was “difficult” and clingy. At the age of five, the child was reunited with his parents. This was, however, short-lived as Jacob’s kindergarten teacher noted signs of physical injuries such as healing bruises, fractured ribs, and cigarette burns on the torso. This prompted Child Protective Services to relieve them of their caretaker duties, return the child to his grandmother, and press injury charges against them.
The child has not had contact with his father since the injury charges were substantiated and have only had a couple of contacts with his mother. He had only had contact with his younger sister a couple of times until she was brought into his grandmother’s custody. This was after complaints of abuse arose. The child’s grandmother reports that the child’s sister is receiving therapy and adjusting to the new situation. She, however, complains that she has suffered depression for years and is afraid that this may affect how she is parenting the child. She also feels overwhelmed with the family situation and is becoming reluctant to reach out to the school for services.
Trauma-Informed Assessment
The trauma system therapy (TST) assessment guide provides a framework for trauma-informed assessment of children with trauma. The first assessment point, as outlined in the TST format, is identifying the problem that will be the focus when treating the child. The information required in this regard includes the number of episodes of the problematic emotions or behaviors exhibited by the child, exposure to traumatic events, and other problems that may be addressed during therapy and will impact the child, such as comorbidities and the social environment.
In Jacob’s case, a moment-by-moment assessment revealed that he had frequent episodes of irritability, anger outbursts, edginess, and mood swings. The child also had a significant history of exposure to traumatic events. At the ages of 18 months and five years, he was removed from his parents, who physically abused and neglected him. McKay et al. (2021) note that physical abuse and neglect at a very young age increase the propensity for a child to develop symptoms of mental health illnesses such as PTSD considerably. The child’s manifestation may thus be a consequence of these traumatic events that he experienced at a younger age.
The child also seems to be disturbed by his social surroundings. He lives with his grandmother, who has a history of depression. His grandmother noted that his behavioral decline started when his sister came to stay with them. He complains that his sister is given more attention than him. Having contact with the abusive mother may also be a contributing factor to the child’s presentation. As per the case, the child had contact with his mother a couple of times. Notably, McLaughlin et al. (2020) suggest that maintaining contact with a perpetrator of violence may contribute to emotional dysregulation. This is particularly pronounced if the perpetrator is a close relative, which may be the case in this child.
The second assessment step is to determine the significance of these problems. These include identifying the functional impact the identified problems may have on the child and the level of concern these problems present to the child and the family. This step also entails prioritizing concerns based on their level of significance. In Jacob’s case, his behavioral issues, as reported by the grandmother, seem to be affecting his schooling. These behaviors have also become a concern to her, as she noted that she is overwhelmed by the family’s situation. This underpins the need for addressing the child’s behavior. The grandmother also has a history of depression, which she fears may affect her parenting. In this case, the priority concern is addressing Jacob’s behavior. Addressing the grandmother’s depression is also necessary as it will also influence the outcome of the child.
The third assessment point is identifying the interventions necessary for addressing the child’s problem. Information required to determine these interventions includes the environmental capacity to help and protect the child and their vulnerability or likelihood of shifting to a survival state. In Jacob’s case, his environment seems to be protective and helpful. His grandmother is currently his primary caretaker. She seems responsible for the child as she is ready to pursue care services for him. A point of concern, however, arises when she claims that she is becoming reluctant to reach out to the school. The child is also vulnerable to shifting to survival states as he sometimes displays episodes of self-awareness, affect, and action. As noted in the case study, he is talkative, has friends, and is social.
The fourth assessment point is identifying strengths. The information required, in this respect, includes the strengths of the child, the strength of their families, and their social environment. In this case, the child’s strengths are his talkative nature, socialization skills, and friends. These could be exploited in therapy. Jacob’s grandmother also shows concern for the child’s well-being and is likely to engage in the therapy processes.
The fifth assessment point is to identify barriers to addressing the problem. Information required includes understanding the trauma, necessary interventions, and the practical barriers to treatment engagement. An apparent barrier to addressing the child’s problem identified in the case is the grandmother’s history of depression. Depression causes significant functional deficits that may be mirrored in parenting and caretaking roles (Brophy et al., 2021). For that reason, this highlights the need for addressing depression.
Cultural and developmental considerations are considered during assessment in trans-cultural and age-specific communication processes. In this respect, the communication process should demonstrate awareness, openness, clarity, respect, and transparency. In case of language barriers, a translator may be sought. Age-specific communication tailors the communication process to age. In this case involving a child and his grandmother, the communication should be clear and transparent, utilizing simple language, appropriate gestures, and other non-verbal cues.
Core Concepts as a Guide to Identify the Most Immediate Treatment Issues for the Client
The core concepts for understanding traumatic stress responses in children and families provide a framework for identifying treatment issues for clients with childhood traumas. The core concept stating that traumatic events generate secondary adversities provides a groundwork for understanding the child’s current presentation. It allows the interrogation of earlier childhood experiences that may contribute to his current manifestation (NCTSN, 2020). Next, the core concept stating that traumatic experiences affect the family and broader caregiving systems informs the need to involve the caregivers’ system in therapy. In this case, the child’s grandmother was involved in therapy. In addition, the core concept stating that trauma can affect a child’s development reinforces the need to address the child’s presentation as a measure for promoting their development. It also gives insight into possible reasons the child in the case may have been struggling in school (NCTSN, 2020). Providing these core concepts points to addressing the child’s behavior. These provisions indicate the likelihood of the child’s presentation affecting the whole family and even his school performance. Addressing these behaviors is thus the priority point of management.
Persons Included in the Treatment Plan
The treatment plan to address this child’s case will draw multiple providers. As such, the client’s treatment plans will include physicians, pharmacists, psychiatrists, and counselors. Psychiatrists, physicians, and pharmacists will diligently diagnose the client and design a therapeutic plan for him. Essentially, physicians will help in diagnosing any underlying pathologies that may be contributing to the child’s presentation, while a psychiatrist will be responsible for diagnosing the exact psychiatric conditions that the child may present. Further, in this case, the pharmacist will aid in designing pharmacotherapeutic plans for the client, while nurses will aid in medication administration where necessary. Lastly, counselors will work with the client, the family, and the school to help the child overcome social and emotional issues. In addition, the systems involved in this case are the family and the healthcare system. The family works with the healthcare providers in addressing the child’s presenting issues.
Description of a Treatment Plan for the Client
The priority intervention outlined upon assessing the client was to manage the child’s behavior. The goals of therapy are to lessen the severity of symptoms, lower the frequency of these symptoms, and improve their performance in school. Regulation-focused treatment is a treatment option that may be beneficial for the child. This psychotherapeutic option is particularly beneficial for children who develop externalizing behaviors. This intervention aims to enhance the child’s emotional regulation capacity and the caregiver’s capacity to protect and help the child. This therapeutic strategy will follow a systematic approach that begins with building the child’s awareness of the behavior, including why and how they respond to their environment the way they do. Subsequently, this is followed by applying this awareness to respond to their environment. The goal is to help the child learn how to use their awareness to gain better self-regulation.
Regulation-focused therapy involves the child, their caretaker, and the therapist. In Jacob’s case, the therapist will work with Jacob and his grandmother to help him obtain skills that will help him have better self-emotional regulation. This may help with his emotional manifestations. Pharmacotherapy may be warranted in Jacob’s case if his bouts of impaired concentration, irritability, edginess, and difficulty sleeping persist. This may improve his concentration in school and subsequently enhance his performance. Besides, Kast et al. (2021) note that pharmacotherapeutic approaches to managing restlessness symptoms and impaired concentration significantly enhance clients’ school performance. This highlights the addition of pharmacotherapeutic approaches to this client’s treatment plan.
Jacob can also be admitted to an individualized educational program to help meet his individual needs. Assessment findings reveal that the child is lagging in school. Jacob also reports that reading was his least favorite learning session. By admitting him into an individual educational program (IEP), Jacob will work closely with instructors to identify the child’s learning and developmental needs. Remarkably, Francisco et al. (2020) note that IEP maintains significance in children with developmental delays and those who manifest externalizing behaviors. It allows children, caregivers, and school administrators to work collaboratively to improve the child’s performance.
The trauma-informed approach encompasses trauma-specific interventions in providing care to clients. When working with this client and his family, the first step is to work with the family to identify the client’s presenting issues. This can be attained through a thorough assessment of the client using the TST framework. This will be followed by using an effective therapeutic approach to address the issue. The regulation-focused technique is valuable in this regard as it aims to equip the child with skills to have better self-regulation. Working closely with the family and maintaining contact will also enable me to follow up on the child’s progress and inform any necessary adjustments to the therapy process. When working with the client, any presenting issues will be addressed promptly based on the provision of ethical practice outlined by the ACA.
When working with this client, referral to psychiatric services and medical services may be necessary. Psychiatrists play a role in diagnosing and managing mental health illnesses. The client may also require medical services and contact with physicians, nurses, and pharmacists if an underlying pathology is identified as a contributing factor to his presentations. These services contribute to the overall wellness of the child. Additionally, regulation-focused interventions will be used in the case. These interventions maintain effectiveness in externalizing behaviors and emotional dysregulations. Clinical interventions used in this approach include cognitive reappraisal, attention control, and response modulation (Di Giuseppe et al., 2020). These interventions may enable the child to understand their behavior better and equip them with control skills.
Personal Reactions to the Case
The case represents how childhood trauma may affect a child in their later developmental stages. Jacob’s history of abuse was a shock to me. However, this should not affect my working relationship with the family. Accordingly, if I experience intense reactions when working with clients, I will take some time out, exercise, exploit my hobbies, and, if necessary, seek healthcare. These self-care strategies will lessen the emotional burden that I may experience after trauma.
Conclusion
Childhood trauma remains a concern in children’s growth and development. They have been implicated in various mental health illnesses. TST provides a framework for identifying presenting childhood manifestations that may have been influenced by the traumatic events they experienced in their earlier lives. The core concepts of understanding traumatic stress responses in children and families provide the groundwork for determining childhood issues that require a prompt address. As evident in the case, Jacob’s manifestation may have resulted from his history. Regulation-focused therapy may be beneficial to Jacob. This intervention equips him with self-regulation skills. Also, the case presented is a replica of how childhood trauma may influence a child’s behavior. It reinforces the need for trauma assessment when working with children presenting with behavior issues.
References
Brophy, S., Todd, C., Rahman, M. A., Kennedy, N., & Rice, F. (2021). Timing of parental depression on risk of child depression and poor educational outcomes: A population-based routine data cohort study from born in Wales, UK. PLOS ONE, 16(11). https://doi.org/10.1371/journal.pone.0258966
Di Giuseppe, M., Prout, T. A., Rice, T., & Hoffman, L. (2020). Regulation-focused psychotherapy for children (RFP-C): Advances in the treatment of ADHD and odd in childhood and adolescence. Frontiers in Psychology, 11. https://doi.org/10.3389/fpsyg.2020.572917
Francisco, M. P., Hartman, M., & Wang, Y. (2020). Inclusion and special education. Education Sciences, 10(9), 238. https://doi.org/10.3390/educsci10090238
Kast, K. A., Rao, V., & Wilens, T. E. (2021). Pharmacotherapy for attention-deficit/hyperactivity disorder and retention in outpatient substance use disorder treatment. The Journal of Clinical Psychiatry, 82(2). https://doi.org/10.4088/jcp.20m13598
McKay, M. T., Cannon, M., Chambers, D., Conroy, R. M., Coughlan, H., Dodd, P., Healy, C., O’Donnell, L., & Clarke, M. C. (2021). Childhood trauma and adult mental disorder: A systematic review and meta‐analysis of Longitudinal Cohort Studies. Acta Psychiatrica Scandinavica, 143(3), 189–205. https://doi.org/10.1111/acps.13268
McLaughlin, K. A., Colich, N. L., Rodman, A. M., & Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1). https://doi.org/10.1186/s12916-020-01561-6
NCTSN. (2020, October 19). The 12 core concepts: Concepts for understanding traumatic stress responses in children and families. The National Child Traumatic Stress Network. Retrieved December 2, 2022, from https://www.nctsn.org/resources/12-core-concepts-concepts-understanding-traumatic-stress-responses-children-and-families.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
Childhood Trauma – Jacob Case Study
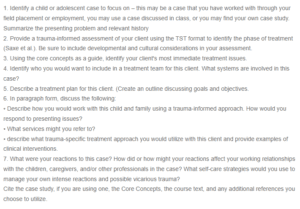
1. Identify a child or adolescent case to focus on – this may be a case that you have worked with through your field placement or employment, you may use a case discussed in class, or you may find your case study. Summarize the presenting problem and relevant history
2. Provide a trauma-informed assessment of your client using the TST format to identify the phase of treatment (Saxe et al.). Be sure to include developmental and cultural considerations in your assessment.
3. Using the core concepts as a guide, identify your client’s most immediate treatment issues.
4. Identify who you would want to include in a treatment team for this client. What systems are involved in this case?
5. Describe a treatment plan for this client. (Create an outline discussing goals and objectives.
6. In paragraph form, discuss the following:
• Describe how you would work with this child and family using a trauma-informed approach. How would you respond to presenting issues?
• What services might you refer to?
• describe what trauma-specific treatment approach you would utilize with this client and provide examples of clinical interventions.
7. What were your reactions to this case? How did or how might your reactions affect your working relationships with the children, caregivers, and/or other professionals in the case? What self-care strategies would you use to manage your intense reactions and possible vicarious trauma?
Cite the case study, if you are using one, the Core Concepts, the course text, and any additional references you choose to utilize.

