Case study – General Anxiety Disorder
Mrs. Baker. C, a 32-year-old female, presents to the clinic after she noted that she is always worried, has a certain fear of everything, has prolonged nervousness, is always feeling tense, and has been having trouble with her sleep within the last three months.
Subjective Data:
- Chief Complaint: Persistent worry, fear, and nervousness, feeling tense, and difficulty sleeping for the past three months.
- History of Present Illness: The client reports feeling edgy, apprehensive, and restless for over the last four months. She is always worried, fatigued, easily irritated, and afraid to go out to social events.
- Demographics: The patient is a White female, a mother of 2, divorced, and a nurse.
- Risk Factors: Work stress, family issues, and recent divorce
- Previous Medical, Surgical, and Psychiatric History: One CS for her second child, no clear mental and medical history
Objective data:
- Physical Exam Findings: The patient has a mildly elevated blood pressure at 128/72 mm Hg, notably tensed muscles, especially around her neck and shoulders. Joint movements within a normal range of motion.
- Mental Status Exam: The client appears tensed, restless, and visibly anxious. She is in a worried mood. All other cognitive functions are intact.
Recommended diagnostic tests:
- Beck Anxiety Inventory (BAI): To assess the severity of anxiety symptoms. The BAI has proven validity in the differentiation diagnosis of depression and anxiety in diverse workplaces and populations (Chapa, 2022).
- General Health Questionnaire (GHQ-12): To test for other mental disorders including depression. GHQ-12 has a higher validity in testing psychological disturbances and disorders and can be self-administered (Hystad & Johnsen, 2020).
Top three differential diagnoses:
- Generalized Anxiety Disorder (GAD)
- Adjustment Disorder with Anxiety
- Depression
Final Diagnosis:
- Generalized Anxiety Disorder (GAD)
Management Plan
As per the Anxiety & Depression Association of America (ADAA) guidelines, GAD can be managed through a combination of psychotherapy with cognitive-behavioural therapy (CBT) as first-line therapy and pharmacotherapy using selective serotonin reuptake inhibitors (SSRIs) (DeGeorge et al., 2022). The patient will be started on CBT 45-minute sessions every Tuesday and Friday for a total of 15 sessions. The patient will also be started on Duloxetine 60mg taken orally once a day.
References
Chapa, O. (2022). An examination of the Beck Anxiety Inventory structure and psychometric properties: A study of American employees. The International Journal of Human Resource Management, 33(12), 2420–2441. https://doi.org/10.1080/09585192.2020.1863246
DeGeorge, K. C., Grover, M., & Streeter, G. S. (2022). Generalized Anxiety Disorder and Panic Disorder in Adults. American Family Physician, 106(2), 157–164. https://www.aafp.org/pubs/afp/issues/2022/0800/generalized-anxiety-disorder-panic-disorder.html
Hystad, S. W., & Johnsen, B. H. (2020). The Dimensionality of the 12-Item General Health Questionnaire (GHQ-12): Comparisons of Factor Structures and Invariance Across Samples and Time. Frontiers in Psychology, 11, 540269. https://doi.org/10.3389/FPSYG.2020.01300/BIBTEX
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
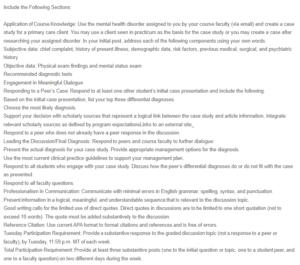
Include the Following Sections:
Application of Course Knowledge: Use the mental health disorder assigned to you by your course faculty (via email) and create a case study for a primary care client. You may use a client seen in practicum as the basis for the case study or you may create a case after researching your assigned disorder. In your initial post, address each of the following components using your own words:
Subjective data: chief complaint, history of present illness, demographic data, risk factors, previous medical, surgical, and psychiatric history
Case study – General Anxiety Disorder
Objective data: Physical exam findings and mental status exam
Recommended diagnostic tests
Engagement in Meaningful Dialogue
Responding to a Peer’s Case: Respond to at least one other student’s initial case presentation and include the following:
Based on the initial case presentation, list your top three differential diagnoses.
Choose the most likely diagnosis.
Support your decision with scholarly sources that represent a logical link between the case study and article information. Integrate relevant scholarly sources as defined by program expectationsLinks to an external site..
Respond to a peer who does not already have a peer response in the discussion.
Leading the Discussion/Final Diagnosis: Respond to peers and course faculty to further dialogue:
Present the actual diagnosis for your case study. Provide appropriate management options for the diagnosis.
Use the most current clinical practice guidelines to support your management plan.
Respond to all students who engage with your case study. Discuss how the peer’s differential diagnoses do or do not fit with the case as presented.
Respond to all faculty questions.
Professionalism in Communication: Communicate with minimal errors in English grammar, spelling, syntax, and punctuation.
Present information in a logical, meaningful, and understandable sequence that is relevant to the discussion topic.
Good writing calls for the limited use of direct quotes. Direct quotes in discussions are to be limited to one short quotation (not to exceed 10 words). The quote must be added substantively to the discussion.
Reference Citation: Use current APA format to format citations and references and is free of errors.
Tuesday Participation Requirement: Provide a substantive response to the graded discussion topic (not a response to a peer or faculty), by Tuesday, 11:59 p.m. MT of each week.
Total Participation Requirement: Provide at least three substantive posts (one to the initial question or topic, one to a student peer, and one to a faculty question) on two different days during the week.

