Case Study – 64-Year-Old Male with Hypertensive Emergency Presenting with Headache and Blurred Vision
The patient is a 64-year-old Black male patient presenting with headache and blurred vision for the past two days and with an elevated blood pressure of 195/115 mmHg, which makes some differential diagnoses possible: hypertensive emergency or hypertensive retinopathy. These complaints that he is currently experiencing are the acute symptoms of the complications that are associated with hypertension, especially with the neglect of follow-up visits.
Differential Diagnoses
Hypertensive Emergency
This condition is defined by abnormally high blood pressure that can produce an acute end-organ dysfunction. Mild forms of the disease present with symptoms such as headache and blurry vision, and urgent management is required to avoid severe complications, including stroke and myocardial infarction (Arikan, 2021). This is the most likely diagnosis for this patient because of the severely elevated blood pressure that is accompanied by symptoms such as blurry vision and headaches, which could be a sign of targeted end-organ damage such as hypertensive retinopathy. This condition needs prompt medical attention to avoid further complications.
Hypertensive Retinopathy
This condition arises due to long-term hypertension, which damages blood vessels in the retina. Its manifestations include visual dysfunction and headache, which are consistent with symptoms (Priya & Murugan, 2019).
Migraine
Although it is less common, given the patient’s history and the severe nature of symptoms, migraines can result in headaches and alterations in vision. Still, this diagnosis is less likely given the dramatically elevated blood pressure.
Plan of Care
Immediate Management
Given the blood pressure value and the symptoms, the patient should be assessed for a hypertensive emergency. He may require admission for intravenous antihypertensive therapy to safely lower his blood pressure. He could be started on nitroglycerin or labetalol for his BP and observed for signs of end-organ dysfunction (Rabi et al., 2020).
Long-Term Management
Once stabilization is achieved, the patient should then be transferred to an oral antihypertensive program. Thus, further individualizing his treatment might require an up-titration of metoprolol to the maximum dose or the introduction of an ACE inhibitor or ARB that would not only address hypertension better but also afford renal protection (Rabi et al., 2020).
Lifestyle Modifications
Education on lifestyle modifications is important. The patient should be advised on changes in diet that can be made, such as the DASH diet, increased intake of fruits and vegetables, low salt intake, exercise, and weight control (CDC, 2023).
Medications
Antihypertensives therapy
The initiation of intravenous antihypertensive medications such as calcium channel blockers (Amlodipine) helps to lower blood pressure in a controlled manner. Also, the use of oral antihypertensives like beta-blockers (metoprolol) can help reduce blood pressure in addition to ACE inhibitors such as lisinopril.
Lipid Management Therapy
The patient’s LDL cholesterol level is very high and thus exposes the patient to a high risk of cardiovascular events; initiation of high-intensity statin therapy like Atorvastatin 40-80 mg daily is advisable (Jacobs et al., 2019).
ASCVD Risk
The patient’s ASCVD (Atherosclerotic Cardiovascular Disease) risk is significantly elevated due to his age (Dehghanbanadaki et al., 2023), hypertension, and dyslipidemia (total cholesterol of 263 mg/dl and LDL of 192 mg/dl). When calculating the ASCVD risk, the Pooled Cohort Equation (PCE) is recommended by the American Heart Association (AHA).
However, for this calculation, the smoking status and blood glucose levels are unknown. Assuming the patient does not smoke and has normal blood glucose, then one can predict the 10-year-ASCVD risk based on known information. Based on these factors, the patient will most probably have an ASCVD risk of over 20%, reflecting a great risk for cardiovascular events (Albarqouni et al., 2019). That would be possible if all the data were available.
Specific Goals
The primary goals should be to keep his blood pressure below 130/80 mmHg and address the LDL cholesterol below 100 mg/dl and even below it in case he has CVDS (Rabi et al., 2020). Therefore, this patient is a challenging case of poorly controlled hypertension with new acute manifestations needing emergent treatment, a search for possible complications, and further long-term management plan with respect to hypertension with specific reference to overall control of blood pressure, lifestyle changes, possible referral for other management and follow up.
Referrals
Ophthalmology
The decision is to refer this patient to an ophthalmologist for further assessment and evaluation of possible retinopathy and management of any visual complications. This will also help check for any other underlying sight-threatening condition that could be contributing to the episodes of blurry vision (Sajid et al., 2023).
Cardiology
Another possible referral would be to a cardiologist for further cardiovascular risk factor evaluation and preventive strategies, as the patient’s ASCVD risk is high, and hypertension is not adequately controlled.
Follow-Ups
Short-Term Follow-Up
An appointment for review within one to two weeks would be advised to check blood pressure and any new manifestations or side effects of medications. Since antihypertensive medications directly act on blood pressure regulation, such constant monitoring is necessary once new antihypertensive therapy is initiated or the patient’s antihypertensive regimen is adjusted.
Long-Term Follow-Up
Schedule follow-up visits for the patients every 3-6 months to assess blood pressure, lipid profile, and cardiovascular markers to assess response and compliance. This monitoring assists in further treatment modifications and risk-reduction strategies.
References
Albarqouni, L., Doust, J. A., Magliano, D., Barr, E. L., Shaw, J. E., & Glasziou, P. P. (2019). External validation and comparison of four cardiovascular risk prediction models with data from the Australian Diabetes, Obesity and Lifestyle study. Medical Journal of Australia, 210(4), 161–167. https://doi.org/10.5694/mja2.12061
Arikan, E. (2021). Hypertensive emergency and hypertensive urgency management in the emergency department. Cumhuriyet Medical Journal. https://doi.org/10.7197/cmj.963044
CDC. (2023). High blood pressure facts. https://www.cdc.gov/high-blood-pressure/data-research/facts-stats/index.html
Dehghanbanadaki, H., Dodangeh, S., Roudsari, P. P., Hosseinkhani, S., Khashayar, P., Noorchenarboo, M., Rezaei, N., Dilmaghani-Marand, A., Yoosefi, M., Arjmand, B., Khalagi, K., Najjar, N., Kakaei, A., Bandarian, F., Meybodi, H. A., Larijani, B., & Razi, F. (2023). Metabolomics profile and 10-year atherosclerotic cardiovascular disease (ASCVD) risk score. Frontiers in Cardiovascular Medicine, 10. https://doi.org/10.3389/fcvm.2023.1161761
Jacobs, D., Wassell, K., Guidry, T. J., & Sullivan, J. (2019). Safety Outcomes of Atorvastatin 80 mg Versus Atorvastatin 40 mg in a Veteran Population. Annals of Pharmacotherapy, 54(2), 151–156. https://doi.org/10.1177/1060028019877540
Priya, T. V., & Murugan, undaram A. (2019). Prevalence of hypertensive retinopathy in newly diagnosed hypertensive patients. Journal of Evidence Based Medicine and Healthcare, 6(14), 1141–1144. https://doi.org/10.18410/jebmh/2019/238
Rabi, D. M., et al. (2020). Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Canadian Journal of Cardiology, 36(5), 596–624.
Sajid, M. Z., Qureshi, I., Abbas, Q., Albathan, M., Shaheed, K., Youssef, A., Ferdous, S., & Hussain, A. (2023). Mobile-HR: An ophthalmologic-based classification system for diagnosis of hypertensive retinopathy using optimized MobileNet architecture. Diagnostics, 13(8), 1439. https://doi.org/10.3390/diagnostics13081439
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
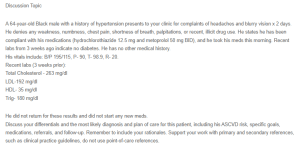
Discussion Topic
A 64-year-old Black male with a history of hypertension presents to your clinic for complaints of headaches and blurry vision x 2 days. He denies any weakness, numbness, chest pain, shortness of breath, palpitations, or recent, illicit drug use. He states he has been compliant with his medications (hydrochlorothiazide 12.5 mg and metoprolol 50 mg BID), and he took his meds this morning. Recent labs from 3 weeks ago indicate no diabetes. He has no other medical history.
64-Year-Old Male with Hypertensive Emergency
His vitals include: B/P 195/115, P- 90, T- 98.9, R- 20.
Recent labs (3 weeks prior):
Total Cholesterol – 263 mg/dl
LDL-192 mg/dl
HDL- 35 mg/dl
Trig- 180 mg/dl
He did not return for these results and did not start any new meds.
Discuss your differentials and the most likely diagnosis and plan of care for this patient, including his ASCVD risk, specific goals, medications, referrals, and follow-up. Remember to include your rationales. Support your work with primary and secondary references, such as clinical practice guidelines, do not use point-of-care references.

