Best Practices in Mental Health Care for the Homeless
Homelessness is a social problem that has significant implications on the physical and psychological health and well-being of the individual. The adverse living conditions associated with the problem particularly increase the risk of mental health problems making this population group especially vulnerable to mental health disparities. Concurrent homelessness and mental illness represent a vicious cycle that derails one’s ability to exit homelessness. Additionally, mentally ill homeless individuals are a hard-to-reach population group due to their low rate of utilization of primary care services. Consequently, these individuals are susceptible to severe impairment due to mental illness. Accordingly, interventions targeting homeless individuals need to apply culturally competent best practices to increase treatment engagement and effectiveness. Two such best practices are service integration and mobile technology-based intervention.
Service Integration
Service integration involves bridging all the health care services targeting homeless individuals, allowing clients to access a variety of basic health and social services in a common setting. Fragmentation of medico-social services impedes the ability of mentally ill homeless individuals to seek outpatient mental health services. Mentally ill homeless individuals have multiple social and health needs, including difficult housing conditions, physical health conditions, mental health disorders such as depression, and competing basic needs such as food insecurity (Youn et al., 2019). However, the location of providers that target these problems in different settings derails the ability of these clients to access or adhere to treatments and keep appointments in the various programs, particularly treatments for mental health needs. These challenges are a further complicated aversion to health services by homeless individuals due to previous adverse experiences or fear of discrimination (Jego et al., 2018). These multiple challenges increase the likelihood of poor attendance of treatment sessions and impede consistent participation in behavioral health groups (Youn et al., 2019). Accordingly, integration of service provides a strategy for improving access to mental health by limiting the effect of barriers to mental health treatment seeking and adherence.
One approach to service integration is the co-location of services. This involves sitting primary health care, mental and behavioral health, social work, and housing support services in a common setting. Randomized controlled trial studies have shown that service delivery models for homeless individuals, integrating primary care with services targeting social determinants of health, reduce hospitalization and the number of emergency department visits (O’Toole et al., 2016). An integrated service model consists of a facility-based multidisciplinary team that is aligned with the homeless population. Alongside mental and behavioral health practitioners, the homeless patient-aligned team should consist of a general practitioner, a social worker, a volunteer, an occupational therapist, a housing worker, and a peer advocate. Service integration enhances coordination and continuity of care for individual mentally ill homeless patients through intra-facility referrals and in-reach. An intervention utilizing such a multidisciplinary team model resulted in greater levels of client satisfaction, improved housing status, and increased utilization of services by homeless clients (Dorney-Smith et al., 2016). A pilot study also demonstrated that interventions provided by a homeless care team yield similar outcomes (Stergiopoulos et al., 2018). Adapting the integrated service model into an outpatient setting increases the number of entry points into mental health treatment services and client engagement.
Mobile Technology-Based Intervention
Mobile phone-based intervention is a technology-based service delivery model that increases access to mental health services, particularly among homeless clients in the young adult age group. This strategy is particularly effective in addressing the access barriers regarding the affordability of mental health services and the availability of services in light of the nomadic lifestyle of this population group. Furthermore, homeless individuals have reported a lack of trust and negative relationships with providers (Adkins et al., 2017). This model is feasible because homeless young adults have access to and use of mobile technology comparable to that of their housed peers (Rhoades et al., 2017). Additionally, more than 25% of homeless young adults use mobile technology-based internet services for at least one hour per day (Adkins et al., 2017). Mobile phone-based technology improves engagement by enabling homeless patients to access mental and behavioral health services between physical outpatient visits.
This practice has shown remarkable potential in studies. Pilot feasibility trials have shown that brief mobile-phone-based mental health engagement programs for homeless young adults resulted in a high participant satisfaction rate and intention to recommend the service (Schueller et al., 2019). Implementation of this intervention on a larger scale and longer duration may enable the impact of the strategy on mental health outcomes to be assessed. A similar study in which mental health and wellness information and self-help tips were conveyed via mobile applications yielded positive outcomes in terms of self-reported satisfaction and treatment benefits in more than 63% of the participants (Glover et al., 2019). Similarly, studies have also shown that homeless young adults recognize mobile phone-based motivational messages, reminders, and tips as important sources of psychosocial support (Adkins et al., 2017). Implementing this strategy in a mental health outpatient setting may increase treatment continuity and engagement among mentally ill homeless clients and mental health service utilization through recommendations.
The mentally ill homeless population is a significantly underserved population group. Accordingly, the realization of positive mental health outcomes requires a culturally sensitive approach that integrates the social determinants of health in this population. Service integration and a mobile phone-based model represent promising best practices for circumventing this population’s mental health care access problem. Adopting these strategies in the outpatient setting may potentially increase the effectiveness of treatments provided in the facility.
References
Adkins, E. C., Zalta, A. K., Boley, R. A., Glover, A., Karnik, N. S., & Schueller, S. M. (2017). Exploring the potential of technology-based mental health services for homeless youth: A qualitative study. Psychological services, 14(2), 238.
Dorney-Smith, S., Hewett, N., Khan, Z., & Smith, R. (2016). Integrating health care for homeless people: Experiences of the KHP Pathway Homeless Team. British Journal of Healthcare Management, 22(4), 215-224.
Glover, A. C., Schueller, S. M., Winiarski, D. A., Smith, D. L., Karnik, N. S., & Zalta, A. K. (2019). Automated Mobile Phone–Based Mental Health Resource for Homeless Youth: Pilot Study Assessing Feasibility and Acceptability. JMIR mental health, 6(10), e15144.
Jego, M., Abcaya, J., Ștefan, D. E., Calvet-Montredon, C., & Gentile, S. (2018). Improving health care management in primary care for homeless people: a literature review. International journal of environmental research and public health, 15(2), 309.
O’Toole, T. P., Johnson, E. E., Aiello, R., Kane, V., & Pape, L. (2016). Peer reviewed: Tailoring care to vulnerable populations by incorporating social determinants of health: the veterans health administration’s “Homeless Patient Aligned Care Team” Program. Preventing chronic disease, 13.
Rhoades, H., Wenzel, S. L., Rice, E., Winetrobe, H., & Henwood, B. (2017). No digital divide? Technology use among homeless adults. Journal of Social Distress and the Homeless, 26(1), 73-77.
Schueller, S. M., Glover, A. C., Rufa, A. K., Dowdle, C. L., Gross, G. D., Karnik, N. S., & Zalta, A. K. (2019). A mobile phone–based intervention to improve mental health among homeless young adults: Pilot feasibility trial. JMIR mHealth and uHealth, 7(7), e12347.
Stergiopoulos, V., Gozdzik, A., Nisenbaum, R., Durbin, J., Hwang, S. W., O’Campo, P., … & Wasylenki, D. (2018). Bridging hospital and community care for homeless adults with mental health needs: outcomes of a brief interdisciplinary intervention. The Canadian Journal of Psychiatry, 63(11), 774-784.
Youn, S. J., Sauer-Zavala, S., Patrick, K. A., Ahles, E. M., Silvan, Y. A., Greig, A., … & Shtasel, D. L. (2019). Barriers and Facilitators to Implementing a Short-Term Transdiagnostic Mental Health Treatment for Homeless Persons. The Journal of Nervous and Mental Disease, 207(7), 585-594.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
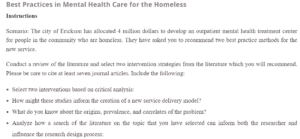
Best Practices in Mental Health Care for the Homeless
Instructions
Scenario: The city of Erickson has allocated 4 million dollars to develop an outpatient mental health treatment center for homeless people in the community. They have asked you to recommend two best practice methods for the new service.
Conduct a review of the literature and select two intervention strategies from the literature that you will recommend. Please be sure to cite at least seven journal articles. Include the following:
- Select two interventions based on critical analysis:
Best Practices in Mental Health Care for the Homeless
- How might these studies inform the creation of a new service delivery model?
- What do you know about the origins, prevalence, and correlates of the problem?
- Analyze how a search of the literature on the topic that you have selected can inform both the researcher and influence the research design process:
- What functions does the literature review serve with respect to the scenario provided?
- How you might go about conducting a literature review for the intervention strategy? Describe the steps you might take.
- Evaluate sources of information that might be related to your topic:
- Evaluate each article.
- Reflect on the applicability of the article to your proposed question.