Balancing Pain Relief and Safety
Although ML’s VS is 135/75, 80, 97.5, 20, indicating a prehypertension blood pressure condition, and her PE is unremarkable, the prescribed drugs may interact to amplify other unidentified health conditions. Her current regimen includes Losartan 50 mg and Gabapentin 300, in which interactions cause motor impairment (Quintero, 2017). Diazepam 5 is also prescribed on a TID PRN basis, which, if not observed, may lead to overuse with eventual harmful side effects related to prolonged Diazepam use. Diazepam is also used alternatively as a depressant. The prolonged risk of CNS depression is related to chronic pain (Peck et al., 2020).
Further, the potential side effects and misuse of combined doses of Gabapentin 300 and Diazepam 5 are a reason for use contraindications. Alternatively, I would offer pregabalin as an alternative to gabapentin and Niacin (Vitamin B3) for Diazepam 5 mg. Before furnishing the drugs, I will need to screen ML for drugs using a urine drug test and assess her emotional, physical, and social alertness about the effects of the currently prescribed medications. In this case, nurse-patient privacy and consideration of her emotional well-being are required after the screening.
For safe prescription of schedule II and III medications, I will require a prescription history and confirmation from a previous care provider, decide the needed amount based on tests and history of use, and confirm the patient’s identity. Before making the prescription, I search the Medical Board of California (MBC) registry for confirmation and adherence to the state’s prescription guidelines (E-Prescriptions | MBC (ca.gov)). The prescription of Schedule II and III medications in the form of NJ is defined by the New Jersey Administrative Code Title 24 on Food and Drugs, Title 8 Department of Health and Senior Services-Chapter 65: Controlled Dangerous Substances, and Title 13-Law and Public Safety, Chapter 39 State Board of Pharmacy-Subchapter 7 Drug: Dispensing and Prescription Records.
All medications in the current ML list require a written script or electronic order. The hand must include the date issued, the patient’s name and address, DOB, the Clinician’s name, address, DEA number, Drug name, strength, form, prescription amount, usage, prior refills, and the prescriber’s signature. After the prescription, a registrant must immediately update the facility’s inventory records and provide all details of the scheduled drug in the state registry.
The minimum required protocols for furnishing schedule II and III controlled substances with a patient-specific approach include:
- Furnish schedule III controlled substances only if the patient has acute illness, injury, recurrent pain, and continuous chronic pain
- Furnish schedule II and III controlled substances only if the patient has pain related to cancer, trauma, or from cancer, an operation, Attention Deficit Hyperactivity Disorder (ADHD), or neuropsychiatric conditions.
- Appropriately adhere to set pain management protocols and department guidelines.
References
https://www.mbc.ca.gov/Resources/Medical-Resources/e-prescriptions.aspx
https://nida.nih.gov/sites/default/files/SamplePatientAgreementForms.pdf
Peck, J., Urits, I., Crane, J., McNally, A., Noor, N., Patel, M., Berger, A. A., Cornett, E. M., Kassem, H., Kaye, A. D., & Viswanath, O. (2020). Oral Muscle Relaxants for the Treatment of Chronic Pain Associated with Cerebral Palsy. Psychopharmacology Bulletin, 50(4), 142–162. https://www.ncbi.nlm.nih.gov/pmc/articles/pmc7901132/
Quintero, G. C. (2017). Review about gabapentin misuse, interactions, contraindications and side effects. Journal of Experimental Pharmacology, 9, 13–21. https://doi.org/10.2147/JEP.S124391
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
You are a new FNP in a restricted state, and you have your DEA license and state furnishing for schedule II-V controlled substances. You are working at a busy family practice group, and you have a patient, ML, who is establishing care for the first time with your practice and comes to you with the following scenario:
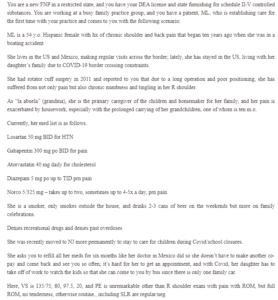
Balancing Pain Relief and Safety
ML is a 54 y.o. Hispanic female with hx of chronic shoulder and back pain that began ten years ago when she was in a boating accident
She lives in the US and Mexico, making regular visits across the border; lately, she has stayed in the US, living with her daughter’s family due to COVID-19 border crossing constraints.
She had rotator cuff surgery in 2011 and reported to you that due to a long operation and poor positioning, she has suffered from not only pain but also chronic numbness and tingling in her R shoulder.
As “la abuela” (grandma), she is the primary caregiver of the children and homemaker for her family, and her pain is exacerbated by housework, especially with the prolonged carrying of her grandchildren, one of whom is ten m.o.
Currently, her med list is as follows.
Losartan 50 mg BID for HTN
Gabapentin 300 mg po BID for pain
Atorvastatin 40 mg daily for cholesterol
Diazepam 5 mg po up to TID prn pain
Norco 5/325 mg – takes up to two, sometimes up to 4-5x a day, prn pain.
She is a smoker, only smokes outside the house, and drinks 2-3 cans of beer on the weekends but more on family celebrations.
Denies recreational drugs and denies past overdoses
She was recently moved to NJ more permanently to stay to care for children during Covid/school closures.
She asks you to refill all her meds for six months like her doctor in Mexico did so she doesn’t have to make another co-pay and come back and see you so often; it’s hard for her to get an appointment, and with Covid, her daughter has to take off of work to watch the kids so that she can come to you by bus since there is only one family car.
Here, VS is 135/75, 80, 97.5, 20, and PE is unremarkable other than R shoulder exam with pain with ROM, but full ROM, no tenderness, otherwise routine., including SLR are regular/neg.
In 600 or fewer words, but a minimum of 250, please describe your approach with this patient. In your paragraphs, include the following:
What are your concerns about her current regimen, and what alternatives will you discuss and offer? What other screenings might you apply? What are your ethical standards in this case that you might consider in addition to legal means?
Provide a sample of an appropriate pain contract that would suit this patient and address her specific safety concerns (cite it and attach the actual arrangement you found – you do not have to make your own – there are plenty online)
Include your steps to ensure safe prescribing. Include the registry you will search before prescribing; name the CA registry, and if you are in a different state, you should also call that registry.
If you were to keep her current list, what are the laws surrounding refills and the amounts you are allowed to dispense with the schedule II and III medications in NJ?
Which medications on her list may you call into the pharmacy, and would you need a written script or electronic order? What elements must be included on the prescription form (paper or electronic signature) for the scheduled medications?
After you prescribe, how, when, and where would you (or your staff) go about making a report of your scheduled prescription in the state registry so that other prescribers and pharmacies could be aware?
In restricted states, APRN prescribers must follow a standardized procedure or protocol for furnishing schedule II and III controlled substances with a patient-specific approach. Please outline the minimum required components of a protocol. You may trace this in bullet form. Alternatively, you may find an appropriate protocol, clinical guideline, or standardized procedure from a literature search and attach it instead of outlining your protocol.


