An Assessment of the Head, Ears, and Eyes
SUBJECTIVE DATA:
Mr. Harold; 68-year-old male; African American
CC (chief complaint): Visual changes in both eyes.
HPI: The patient is a 68-year-old male who reports to the healthcare facility for his routine annual physical examination. The patient says his vision has worsened in both eyes over the last two months. On inquiry, the patient reveals that he has been a glaucoma patient for the past five years. For his glaucoma, he takes Timolol eye drops. Mr. Harold is also a hypertensive patient and controls his blood pressure with oral antihypertensives. He also has hyperlipidemia, for which he takes lipid-lowering agents.
Medical History
- Current Medications: The patient is currently on a cholesterol-lowering agent (atorvastatin), antihypertensives (enalapril), and eye drops (timolol)
- Allergies: the patient reports an allergy to shellfish.
Social History: The patient is a school bus driver.
ROS:
HEENT:
Head: No headaches
Eyes: Reports worsening vision over the last two months.
Ears: No earaches
Nose: No sneezing, rhinorrhea, or congestion
Throat: No dysphagia, odynophagia, or sore throat.
CARDIOVASCULAR: No chest pain, orthopnea, dyspnea, or edema.
RESPIRATORY: No chest pain, no difficulty in breathing, no cough, no shortness of breath.
GASTROINTESTINAL: No nausea, vomiting, abdominal pain, constipation, or diarrhea
GENITOURINARY: No hematuria, dysuria, or incontinence
NEUROLOGICAL: No loss of consciousness, seizures, memory changes, local numbness or tingling, or paralysis
MUSCULOSKELETAL: No joint stiffness or pains; no backache; no joint tenderness or swelling
HEMATOLOGIC: No anemia; no bruising or bleeding
SKIN: no itchiness or changes in the hair.
LYMPHATICS: No lymphadenopathy
ENDOCRINOLOGIC: No thyroid problem; no excessive sweating; no heat or cold intolerance; no polydipsia or polyphagia.
OBJECTIVE DATA:
Physical exam:
Vital signs: blood pressure is 118/68 mmHg, Heart rate is 86 bpm, the temperature is 37, and resp rate is 16
GENERAL: The patient is in generally fair condition with no signs of obvious distress. The patient is alert and oriented to person, place, and time.
HEENT:
Head: Atraumatic, normocephalic
Eyes: Pupils are normal, round, and reactive to light. No scleritis, no diplopia. Vision testing-right look is 20/30, and left eye is 20/50.
Ears: No earaches. Hearing is normal.
Nose: No sneezing, rhinorrhea, or congestion
Throat: No dysphagia, odynophagia, sore throat, or thyromegaly
CARDIOVASCULAR: no murmurs, no gallops, S1 and S2 heard.
RESPIRATORY: Vesicular breath sound heard bilaterally. No respiratory distress
SKIN: No lesions or rashes.
GIT: Bowel sounds heard.
NEUROLOGICAL: The patient is alert and oriented
HEMATOLOGIC: No anemia; no bruising or bleeding
LYMPHATICS: No lymphadenopathy
Risk Factors
Race. The patient is an African American, and this increases his risk of developing open-angle glaucoma 3-4 times. It has been documented that glaucoma is the most common cause of blindness in people of African descent. African Americans are also more likely to develop glaucoma at an earlier age compared to Caucasians. Black patients are generally predisposed to glaucoma because they have a thinner average central corneal thickness. This leads to the underdiagnosis of elevated intraocular pressure. Also, the mean intraocular pressure is higher in blacks than in Caucasians (Biggerstaff & Lin, 2020).
Old Age. Age is a risk factor for glaucoma, especially for patients over 40 years. Intraocular pressure increases with age, which leads to an increased risk of developing glaucoma. Glaucoma is more prevalent in the aging population, even though it is not limited to this population alone (Biggerstaff & Lin, 2020).
High blood pressure is a factor that has been associated with glaucoma. It is, however, not a confirmed risk factor for open-angle glaucoma. The patient is hypertensive, and therefore, it is possible that this could be a potential risk factor (Dietze, 2021).
References
Biggerstaff, K. S. & Lin, A.P. (2020). Primary open-angle glaucoma (POAG). Practice Essentials, Background, Pathophysiology. Retrieved from: https://emedicine.medscape.com/article/1206147-overview#a5.
Dietze, J. (2021, July 3). Glaucoma. StatPearls [Internet]. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK538217/.
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
You will perform a history of a head, ear, or eye problem that your instructor has provided you or one that you have experienced and assess the head, ears, and eyes. You will document your findings and identify actual or potential risks.
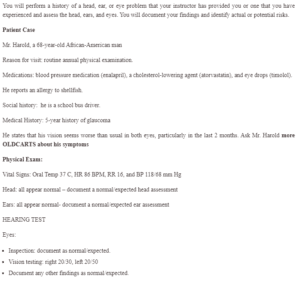
An Assessment of the Head, Ears, and Eyes
Patient Case
Mr. Harold, a 68-year-old African-American man
Reason for visit: routine annual physical examination.
Medications: blood pressure medication (enalapril), a cholesterol-lowering agent (atorvastatin), and eye drops (timolol).
He reports an allergy to shellfish.
Social history: he is a school bus driver.
Medical History: 5-year history of glaucoma
He states that his vision seems worse than usual in both eyes, particularly in the last two months. Ask Mr. Harold more OLDCARTS about his symptoms
Physical Exam:
Vital Signs: Oral Temp 37 C, HR 86 BPM, RR 16, and BP 118/68 mm Hg
Head: all appear normal – document a normal/expected head assessment
Ears: all appear normal- note a normal/expected ear assessment
HEARING TEST
Eyes:
- Inspection: document as normal/expected.
- Vision testing: right 20/30, left 20/50
- Document any other findings as normal/expected.

