Falls Prevention in the Acute Care Healthcare Improvement Project
D156: Business Case Analysis for Healthcare Improvement
Healthcare Improvement Project: Introduction and Project Initiation
Patient safety is an inherent concern in acute care processes and during handoffs like nurse shift changes. Clear communication among handoffs has been noted as one of the factors that lead to adverse events, including patient falls. This Healthcare Improvement Project (HIP) aims to introduce a standardized bedside reporting protocol to enhance the flow of communication and decrease the incidences of falls in an acute care unit. The project displays a systematic pattern, which involves SMART goals, stakeholder contributions, and strategies that are based on evidence: Falls Prevention in the Acute Care Healthcare Improvement Project.
This initiative aims to improve staff accountability, patient safety, and care continuity by incorporating the principles and best practices of project management. The critical points are the development of training, performance measurement based on KPIs, and the application of such tools as SWOT and impact analysis. This paper describes all the stages of the project lifecycle, which presents a complete implementation and evaluation plan.
Organizational Problem
The problem I would like to solve with the help of my healthcare improvement project (HIP) is a high patient fall rate during shift changes in an acute care setting. The most common times when the accidents occur are the time when handovers between shifts are taking place and when monitoring the members of staff carries insufficient attention, communication is poor, and the safety guidelines regarding falling prevention are not followed. There are specific threats to my organization, especially in the area of changing shifts, since additional labor, employee turnover, and the lack of smooth handoffs often take place during this period.
This has led to patients, particularly those at high risk of falling, not being closely monitored, which has resulted in an increased rate of falls. The background of this problem is that the hospital does not currently have a regulated workflow, and the shift handoff is not standardized, which means that the personnel are busy with administrative duties and not entirely devoted to patient care. This created a system fault, resulting in falls that were avoidable and caused patients injury as well as extended length of stay and national health spending. Therefore, bedside reporting in the form of exercises during a shift change improves communication and patient safety.
Stakeholders
The Inpatient Directors are rather influential and powerful in the use of the bedside reporting program. They are tasked with the alignment of the hospital-wide objectives towards patient safety enhancements. They are interested in minimizing injuries as a result of falls and ensuring that the hospital complies with health care requirements.
The authority of the inpatient directors lies in the fact that they can distribute the resources, certify rules and policies, and make sure that the project they propose correlates with the general goals of the hospital. They are the key to the success of the project in the sense that they determine the consent and allocation of resources to carry out the initiative in various departments.
Another stakeholder is the Nurse Manager of Acute Care, who has a significant power of control over the success of the project. Their role is to supervise the staff in the nursing field and guide the new bedside reporting procedure to be followed and implemented accordingly. They are interested in promoting patient safety, positive communication between personnel, and efficient coverage.
The authority of the nurse manager allows the policies to be imposed on the target audience and measures their adherence and guidance of the nursing staff through the course of implementation. Their motivation and leadership of the team are also important in the integration of the initiative in practice.
Nurse educators play a significant role in training the nursing staff, facilitating effective communication, and promoting an understanding of the bedside reporting process and subsequent adherence to it. One of their influences is how they design educational content and conduct content. They ensure that nurses are well-prepared to give the best quality of patient care.
Furthermore, the nurse educator can directly influence the staff’s level of knowledge and preparedness, which is essential to the project’s success. With adequate training, the project will become more successful in minimizing falls during shifts.
Project Team
Two important roles that I will play as the project manager of the Fall Prevention in Acute Care initiative will be coordinating project activities and stakeholder engagement management. As the person handling the coordination of the project, I will make sure that every stage of the project, including the planning and implementation, is met on time and within the budget available. In this position, I will be required to monitor the progress of this project, ensure that various members of the team beat deadlines, and solve any arising problems.
Since my position is managing stakeholder engagement, I will work with all the stakeholders, including those in charge of the hospital, nursing staff, and quality improvement teams, to ensure that they are aware of the objectives of the project and working towards its completion. Consistent communication will be important in carrying momentum and gaining continuous interest in the project.
Besides these, I am also expected to oversee the project performance as well as change management. Performance monitoring would involve monitoring of indicator measures such as the rate of falls at the shift change, which determines whether the project would give the needed outcomes. I shall also be able to identify the differences and make the required corrections.
Leading change management will include engaging the team of nurses towards making a shift to bedside reporting, overcoming any kind of resistance, and seeing through the implementation of the new procedures. I will assign adequate resources, training, and support so that the team feels good about implementing a new workflow.
I possess two major leadership skills: communication and problem-solving, as the project manager. Effective communication will enable me to clearly state the expectations, objectives, and progress to all stakeholders, thereby ensuring everyone is on the same page. The ability to solve problems will play a significant role in addressing complications that may arise during implementation, such as staff resistance or slow adoption of bedside reporting.
The nurse educator is also another key project team member. They will develop training material on bedside reporting and provide education sessions to nursing personnel. They will also be expected to gauge the success of the training and make necessary adjustments to the curriculum by considering feedback from staff and the assessment success rate. This role will ensure that nurses are prepared to adopt the new reporting system, which is crucial to the initiative’s success.
Needs Assessment
In the case of the Needs Assessment, I employed the Cause-and-Effect Diagram (Fishbone) tool to identify the underlying causes behind the patient’s needs during the shift in the acute care facility. Breaking down complex issues with the Fishbone tool into groups like People, Processes, Environment, and Interventions proved to be the best option, as it enabled a project team to identify particular forces requiring project attention. This helped to create a clear picture of the root problems and develop specific interventions, such as bedside reporting.
When developing the needs assessment, stakeholders and project team members openly discussed the issue of patient falls, especially those that occurred during shift change. We identified some themes related to the root causes of the problem. Within the team, issues were discussed regarding how the absence of a handoff procedure and inconsistent communication during shift changeovers contributed to falls. The staff was concerned about the inability to see high-risk patients, especially when making reports outside the bedside.
Environmental elements, such as walking through crowded hallways and using insufficient lighting during shift changes, were also identified as risk factors for falling (Lee, 2021). Based on these discussions, the team realized that one way to address some of these issues is to implement a more effective handoff process that includes bedside reporting, which would improve communication and facilitate real-time patient assessment.
The two essential needs assessment results were that the irregularity of handoff procedures and environmental risks were considered the significant causes of patient falls. The team acknowledged that significant details are often omitted when reports are not carried out at the bedside, including details concerning the patient’s mobility and the risk posed by the patient to fall. Additionally, environmental risk factors such as clutter and dim illumination contributed to the occurrence of falls, which increased during shift changes when the staff’s attention was divided. These results demonstrated the necessity of having an organized process of bedside reporting so that everyone could feel much more secure during the transition period and have better communication.
SWOT Analysis
Among the weaknesses highlighted in the SWOT analysis are that staff is resistant to change, and there is variable training on shifts. When implementing new processes, staff resistance is frequent because nurses may reason that the newly added activities during shift changes will only burden them. Accordingly, I will involve nursing leadership earlier to minimize this and win their support. I will also explain the advantages of bedside reporting, particularly in terms of decreasing workload and improving patient safety and communication (Jimmerson et al., 2020).
Regarding irregular training, employees on different shifts might have various degrees of knowledge of the new procedure. To counter this, I will liaise with the nurse educator to develop standard and inclusive training material and conduct training on all shifts to provide uniformity in knowledge and practice.
The two main threats identified are the issue of time limits when changing shifts and the issue of staff not being compliant. Limited time is one of the threats, as nurses already have multiple duties to attend to during a shift change and are thus unlikely to accept an extra task on bedside reporting. To help control this, I will streamline the reporting process and discuss with leadership the need for adequate staffing during shift changes, particularly when there are more people on a shift, thereby easing the pressure (Harrison et al., 2021).
There should also be noncompliance if the nurses do not regularly adhere to the new protocol. I will establish a system of regular checkups and feedback to monitor compliance and curb setbacks by providing extra support and training.
Leadership support and fall prevention protocols are key strengths of the project. Strong leadership support is critical for securing the necessary resources and support needed for successful implementation. To maximize this strength, I will ensure constant communication between myself and the leadership so that there is continuous support and that they are notified about concerns that may arise.
Fall prevention programs that have already been implemented serve as a good background for incorporating bedside reporting (Turner et al., 2022). In addition, I will ensure that bedside reporting is smoothly integrated into the existing processes without negatively impacting the current practice and enhance the current approach to patient safety.
Interdisciplinary collaboration and hospital-wide implementation are the two main opportunities the project can leverage. Nursing, quality improvement, and physical therapy teams are examples of multidisciplinary collaboration focusing on patient safety. To ensure this, I will promote frequent contact among the departments, creating a team atmosphere.
There is an opportunity to implement hospital-wide changes and make bedside reporting available across all units (Turner et al., 2022). To take advantage of this, I will report the project’s success and results and advocate for differences supported by data in favor of broader adoption in the hospital.
Impact Analysis
According to the Impact Analysis Template, the Total Benefits Score was 12, and the Total Risks Score was 10, with an Impact Ratio of 1.2. The impact ratio is a simple formula where the benefits are divided by the risks, and in this instance, the impact ratio would be 1.2. This means that the advantages of implementing the bedside reporting system during shift changes outweigh the risks associated with it, and such an initiative can be an effective and advantageous one for the hospital.
The advantages to the organization under the impact ratio will be increased patient safety and minimized injuries associated with falls. Bedside reporting guarantees real-time patient evaluation, improving communication between outgoing and incoming staff so that high-risk patients can be monitored better (Chien et al., 2022).
This contributes to fewer falls and complications following falls, and finally, healthcare costs due to prolonged stays and treatments are decreased. Additionally, customer satisfaction will increase since the treatment procedure will be more detailed and mindful, which will contribute to the enhanced performance rate of the hospitals.
The risks, however, are associated with the possibility of staff resistance to change and the factors related to the time spent on reporting extra work and additional demand, especially when shifts change. Such resentment may result in noncompliance, which can affect the success of such an effort. Nevertheless, the risks are preventable with proper training, constant support, and leadership involvement to implement it smoothly and ensure staff commitment (Ystaasa et al., 2023).
The impact ratio of 1.2 indicates that there are risks. However, the overall benefits, including improved patient safety, economic growth through reduced rates of falls, and enhanced staff communication, make the initiative worthwhile for the hospital.
Justification and Project Purpose
This Healthcare Improvement Project (HIP) aims to decrease patient falls on shift change in the acute care facility by introducing bedside reporting. The application of bedside reporting shift changes allows nurses to directly evaluate patients, thereby enhancing communication between personnel transitioning from duty to off-duty and those assuming duty.
In turn, this ensures that key information concerning patient conditions is properly transferred and fall vulnerabilities are promptly recognized and addressed (Cruchinho et al., 2023). Bedside reporting is another way to identify the causes of patient falls in the unit, as it enhances communication, especially during handoff periods, and to some extent, it ensures patients are not left to their own devices.
Indeed, this project will determine the solution to the issue of the rise in falls during shift changes because of ineffective communication, inadequate monitoring of fall prevention, and inconsistent response performance (Garcia et al., 2021). Communication breakdown, employee distraction, and the surrounding environment, including cluttering hallways and insufficient lighting, are causes of these falls during the needs assessment. Using bedside reporting, the hospital can mitigate such problems and decrease the chances of falls during shifts.
Based on the needs assessment, we found important themes, such as communication lapses and environmental risks, to be factors that can exacerbate the problem. According to the SWOT analysis, there are some challenges in the analysis, including resistance to change and staff, but the availability of the fall prevention protocols and the support of the leaders is a significant strength in the analysis to support the project.
Impact analysis affirmed that the advantages that improved patient safety, decreased falls, and enhanced communication among staff offset the risks, which are time limitation and staff resistance. The finding of the impact ratio of 1.2 proved that bedside reporting is a worthwhile intervention to improve patient safety at shift handovers.
Review of Relevant Scholarly Sources
A research article by Albasha et al. (2024) titled Staff Perspectives on Fall Prevention Activities in Long-Term: Care Facilities among Older Residents is very significant for gaining insights into the appropriate strategies for preventing falls. In the study, the role of education and training of the staff in the prevention of falls among older residents is highlighted. It indicates that frequent education interventions that are short in duration are likely to be more effective than long, infrequent training interventions.
This approach is somewhat practical in guaranteeing that the staff is not going to be out of the loop and that fall prevention strategies will be used in their daily activities. The paper also emphasizes that the addition of a staff-to-resident ratio and appropriate skill mix are important in improving the role of fall prevention (Albasha et al., 2024). Notably, sufficient staff would enable them to monitor and support timely remedial actions to ensure that the risks of falls are circumvented. This good practice can be translated to better patient safety and fall-related injury areas of a long-term care facility.
The article of Appeadu and Bordoni (2023), which discusses the topic of Falls and Fall Prevention in Older Adults, gives a detailed and comprehensive coverage of falls among older adults, their risk factors, and fall prevention. The most prevalently reported type of accident in individuals 65 years and above were referred to as falls, and they result in excess morbidity and mortality. The article concludes that the occurrence of the chance of falls is associated with the prevalence of risk factors, which include medical use of drugs such as antihypertensives, neuroleptics, sedatives, subpar cognitive state, sarcopenia, and postprandial hypotension.
Other predisposing factors have been discovered as well, such as obesity, which is caused by muscle quantity and neuromuscular mechanisms. According to Appeadu and Bordoni (2023), a complex prevention strategy is vital regarding the use of medication, individual physical activity, intervention related to the environment, and management of intrinsic risk factors within the specification of patients receiving treatment. This in-depth knowledge aims to initiate the implementation of bedside reporting as one of the communication alternatives that may enhance the communication process during transition periods and, therefore, assure proper identification of possible fall risks and patient safety.
The article by Jimmerson et al. (2020) on bedside shift reporting (BSR) identifies a number of best practices that can be regarded to enhance the process implementation. Among the practices, the adjustment of the BSR approach was implemented so that there was a partial handoff in the room and a partial handoff outside the room. This method allows the confidential creation of sensitive information, but it does not exclude the patient from partial involvement in his or her care, which helps in better communication and involvement.
The other best practice is the process of personalizing the report content to cover the condition the patient is in and what the nurse knows about the patient. Such an individualized plan will aid in maintaining the information exchanged clearly and correctly by preventing over-information, which enhances the quality of the handoff communication process (Jimmerson et al., 2020). Such practices can lead to better patient safety, fewer occurrences of miscommunication, and higher nurse satisfaction, which falls in line with the goals of the Healthcare Improvement Project, as it aims to eliminate the number of patient falls during shift changes.
The research by Ojo and Thiamwong (2022) is a systematic review that focuses on the positive impacts of nurse-led fall prevention initiatives in older people. It was composed of 6 randomized control trials, two non-randomized control studies, and three quasi-experimental designs. The findings indicate that nurse-intervened interventions, which entail the evaluation of patients, their education, exercises, and post-discharge, can massively reduce the rate and incidence of falls.
Also, these programs positively influence patients and make them become more active participants in fall prevention processes. Ojo and Thiamwong (2022) came to the conclusion that education-based fall prevention programs that are applied to older adults and to nurses as a group are a promising choice that yields good outcomes, and the role of a nurse in maximizing patient safety and reducing the detriments of falls-related injuries earns an important point.
The article by Randell et al. (2024) on the assessment and prevention of falls within acute hospitals highlights the importance of engaging patients in the care process to minimize the risk of falls. The study established that patients’ active involvement in assessing and planning their care would increase the likelihood of their understanding interventions aimed at fall prevention and engaging in such interventions, as well as communication between staff implementing their strategies.
Besides building confidence among patients, such participation also helps prevent future falls by enabling patients to understand better their individual fall risk and the steps that can be taken to mitigate it. Ojo and Thiamwong (2022) have indicated that patient-centered care, in which patient needs and preferences are considered, has become key in minimizing fall events. The introduction of bedside reporting aligns with this best practice because it promotes direct nurse-patient communication, allowing patients to be aware of and participate in their care plan, which leads to enhanced safety and a minimized fall risk.
The two best practices found in the review of the articles propose the appropriate practice of BSR in order to reduce the number of patient falls that do occur at shift changes, and these are the following. To start with, it has been proven that the involvement of patients in their care during shift changes promotes greater communication and safety.
Patient participation in handoff has been considered to lead to improved conversation with the patients, thus increasing patient safety and satisfaction with the nurses due to the reduction of the fall rate. Such a practice contributes to fewer incidences of falls during shift changes due to the accurate delivery of important information and the involvement of patients in various treatment procedures (Jimmerson et al., 2020).
Second, nurse-based fall prevention programs are helpful in preparing nurses to recognize the causes of fall risks and apply interventions to individual patients. Such interventions include educating personnel on the detection of patients at risk of falling, the application of mobility aids, and regular evaluations as a fall prevention measure. Ojo and Thiamwong (2022) indicate that programs of this nature significantly decrease the rate of falls and their adverse effects on patients by transforming nurses into the most active stakeholders in fall prevention action, an objective that the project aims to achieve in acute care.
Project Environment
Among the policies that may affect the project’s implementation is the hospital’s Patient Safety and Fall Prevention Policy. This policy outlines the procedure for evaluating the risk of falls, executing interventions to prevent falls, and reporting falls. The policy directly supports my project, as the design of bedside reporting practice will align with current fall prevention strategies (Natora et al., 2022).
It assists in improving communication during shift transfers, with a priority focus on fall risks during handoffs so that care for high-risk patients is provided according to safety precautions. The policy that emphasizes consistent monitoring and intervention to prevent falls creates a solid foundation for starting the project, as this approach would integrate the bedside reporting project into the existing system. In the long run, it could enhance patient safety and prevent falls.
SMART Goal
By December 15, 2025, 90% of nursing personnel in the acute care unit will consistently conduct bedside reporting during each shift, resulting in a 15% decrease in patient falls during shift changes. This will be achieved by enhancing handoff communications and ensuring that fall risks and other pertinent patient information are effectively communicated among nursing staff members.
Audits of the bedside reporting implementation, along with feedback provided by the staff, will be utilized. Compliance with the bedside reporting protocol, at 90%, will be used as the indicator of project success, and a decrease in the number of fall incidents will be deemed evidence of increased patient safety and communication.
KPI #1
Before the implementation of the project, 100% of the bedside reporting training program will be developed. KPIs are crucial in ensuring that the project stays on track and that the desired objective is met. The first KPI will be based on developing the bedside reporting training program, with all materials to be ready by July 20, 2025. The training will involve significant aspects of bedside reporting, such as the purpose, steps involved, and advantages to patient safety.
The nurse educator will create training materials that will be implemented by the project manager, who will oversee the process to ensure it aligns with the project’s goals and objectives. The training program will be completed before the staff training session starts, ensuring the nursing staff is well-prepared to apply the protocol successfully.
KPI #2
All educational materials needed during bedside reporting will be created by the time the project is implemented. The KPI associated with the training will involve planning and signing off on the training materials by the nurse educator. The materials will be provided as a one-hour training session with the nurse supervisors, and the nursing staff will attend a one-hour training session in a small-group setting.
Participation and understanding will be recorded through attendance and the signing of policy awareness forms. At least 95% of all nursing personnel will complete their training and be ready to implement the new bedside reporting process by 8/10 2025. This KPI will be supervised by the project manager, who will monitor progress and verify that all staff comply with it before the implementation stage.
Key stakeholders, including the nurse manager, inpatient directors, and nurse educators, were engaged in meetings to gather the views of stakeholders and project team members. The nurse manager stressed the importance of clear communication during shift changes, with a particular focus on fall risks. The inpatient directors emphasized the importance of adhering to the hospital’s patient safety objectives and the value of tangible results.
The nurse educator highlighted the significance of training staff to comply with protocol. The discussions identified priority areas, including training, communication, and staff participation, which were incorporated into the SMART goal. The purpose was expected to be narrow, measurable, and time-sensitive, covering the needs of staff education and patient safety so that it aligns with the hospital’s and nursing team’s priorities and objectives.
Project Management Lifecycle
The fact that fall prevention project management has four stages—initiation, planning, implementation, and evaluation—is the backbone of the project’s success. Phase one of the implementation is the initiation process, which requires gathering the key stakeholders and team members to frame the issue of patient falls during shift changes and determine the desired result: the reduction of patient falls through enhanced and improved communication with bedside reporting.
During planning, the team will draw a roadmap that outlines the implementation timeline, activities, required resources, and functions. This step is necessary to inform all parties of their roles and ensure the plan aligns with hospital objectives. The implementation phase follows, during which the nursing staff receives training and bedside reporting is introduced.
The period will also entail tracking the staff’s compliance levels and feedback to modify the procedure. Lastly, the evaluation will determine the project’s success based on the decrease in fall rates and the effectiveness of bedside reporting. When the project is not as successful as expected, the review process will be able to identify where a setback occurred. Thus, there can be possible adjustments and a follow-up to the final meeting to improve the process.
References
Albasha, N., Curtin, C., McCullagh, R., Cornally, N., & Timmons, S. (2024). Staff perspectives on fall prevention activities in long-term care facilities for older residents: “Brief but often” staff education is key. PLOS ONE, 19(9), 1–20. https://doi.org/10.1371/journal.pone.0310139
Appeadu, M., & Bordoni, B. (2023, June 4). Falls and fall prevention in the elderly. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560761/
Chien, L. J., Slade, D., Dahm, M. R., Brady, B., Roberts, E., Goncharov, L., Taylor, J., Eggins, S., & Thornton, A. (2022). Improving patient-centered care through a tailored intervention addressing nursing clinical handover communication in its organizational and cultural context. Journal of Advanced Nursing, 78(5), 1413–1430. https://doi.org/10.1111/jan.15110
Cruchinho, P., Teixeira, G., Lucas, P., & Gaspar, F. (2023). Influencing factors of nurses’ practice during the bedside handover: A qualitative evidence synthesis protocol. Journal of Personalized Medicine, 13(2), 267. https://doi.org/10.3390/jpm13020267
Flaubert, J. L., Menestrel, S. L., Williams, D. R., & Wakefield, M. K. (2021). Supporting the health and professional well-being of nurses. In www.ncbi.nlm.nih.gov. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK573902/
Garcia, A., Bjarnadottir, R. (Raga) I., Keenan, G. M., & Macieira, T. G. R. (2021). Nurses’ perceptions of recommended fall prevention strategies. Journal of Nursing Care Quality, Publish Ahead of Print(3). https://doi.org/10.1097/ncq.0000000000000605
Harrison, R., Fischer, S., Walpola, R. L., Chauhan, A., Babalola, T., Mears, S., & Le-Dao, H. (2021). Where do models for change management, improvement, and implementation meet? A systematic review of the applications of change management models in healthcare. Journal of Healthcare Leadership, 13(2), 85–108. https://doi.org/10.2147/JHL.S289176
Jimmerson, J., Wright, P., Cowan, P. A., King-Jones, T., Beverly, C. J., & Curran, G. (2020). Bedside shift report: Nurses’ opinions based on their experiences. Nursing Open, 8(3), 1393–1405. https://doi.org/10.1002/nop2.755
Lee, S. (2021). Falls are associated with indoor and outdoor environmental hazards among community-dwelling older adults, and they are between men and women. BMC Geriatrics, 21(1). https://doi.org/10.1186/s12877-021-02499-x
Natora, A. H., Oxley, J., Barclay, L., Taylor, K., Bolam, B., & Haines, T. P. (2022). Improving policy for the prevention of falls among community-dwelling older people—A scoping review and quality assessment of international national and state level public policies. International Journal of Public Health, 67. https://doi.org/10.3389/ijph.2022.1604604
Ojo, E. O., & Thiamwong, L. (2022). Effects of nurse-led fall prevention programs for older adults: A systematic review. Pacific Rim International Journal of Nursing Research, 26(3), 417. https://pmc.ncbi.nlm.nih.gov/articles/PMC9432804/
Randell, R., McVey, L., Wright, J., Zaman, H., Cheong, V., Woodcock, D. M., Healey, F., Dowding, D., Gardner, P., Hardiker, N. R., Lynch, A., Todd, C., Davey, C., & Alvarado, N. (2024, March 1). Patient participation. Practices of Falls Risk Assessment and Prevention in Acute Hospital Settings: A Realist Investigation – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK602079/
Turner, K., Staggs, V. S., Potter, C., Cramer, E., Shorr, R. I., & Mion, L. C. (2022). Fall prevention practices and implementation strategies. Journal of Patient Safety, 18(1), 236–242. https://doi.org/10.1097/pts.0000000000000758
Ystaas, L. M. K., Nikitara, M., Ghobrial, S., Latzourakis, E., Polychronis, G., & Constantinou, C. S. (2023). The impact of transformational leadership in the nursing work environment and patients’ outcomes: A systematic review. Nursing Reports, 13(3), 1271–1290. https://doi.org/10.3390/nursrep13030108
Appendix A
SMART Goal Worksheet (D156)
Work with your stakeholders, project team members, or both to create a SMART (specific, measurable, achievable, relevant, time-bound) goal and two process KPIs for your healthcare improvement project (HIP). Answer the following SMART questions about your project. Next, synthesize your answers into a SMART goal for your project and enter it into the SMART Project Goal box.
| SMART
Questions |
SMART
Answers |
|||||
| Specific:
· What is your project? (Be specific) · How will you accomplish this? (interventions) |
The project aims to reduce patient falls during shift changes in the acute care unit by implementing bedside reporting as a new communication protocol for handoffs.
This will be achieved by training nursing staff to perform bedside reporting during shift changes, ensuring real-time patient assessment, and better communication between outgoing and incoming nurses. |
|||||
| Measurable:
· What will you measure to determine your project’s success? (Indicators or metrics) · How will you know that change has occurred? · What percentage of the outcome will you accomplish by date? (Numbers and quantities provide means of measurement and comparison). |
The primary metric will be the number of patients who fall during shift changes before and after implementing bedside reporting. Success will also be measured by nurse compliance with the new bedside reporting protocol.
The goal will be to reduce 15 percent in patient falls in the acute care unit by December 31, 2025. Also the audit of adherence to bedside reporting protocol by the nurses will also be conducted weekly until at least 90% adherence is achieved on October 31, 2025. |
|||||
| Achievable:
· Based on your impact analysis and SWOT analysis, what support, resources, and justification exist for your project? |
According to the Impact Analysis (Impact Ratio of 1.2) and the SWOT Analysis, the project is feasible. There is good leadership backing and in the organization, there are fall prevention policies already in place.
The availability of resources that include staffing or time of training, and policy alignment can be made available. The strengths and opportunities identified, such as the support of top management, interprofessional cooperation, and the already existing fall prevention infrastructure, show that the project is ready to succeed. |
|||||
| Relevant:
· Is your project worthwhile? · Why does your project matter to the target population, the organization, and nursing practice? |
This project is relevant because it directly addresses patient safety by reducing falls, a critical issue in acute care settings. The project aligns with the hospital’s goals of improving patient care quality and reducing fall-related costs.
The project is directly related to the nursing practice as it solves one of the most critical issues regarding patient safety, falls that can cause serious harm, prolong the hospital stays, and increase healthcare expenses as well. Nurses are the most critical players in the monitoring of the patient, handoff communication, and compliance. Enhanced bedside reporting reinforces continuity of care and accountability and fits the nurse’s role in caring about safe transition and preventing preventable harm. |
|||||
| Time-Bound:
· Health Placement Approval date · D156 course start date · Project start date · Project end date · Expected graduation date |
· Health Placement Approval date: 6/3/2025
· D156 course start date: 6/16/2025 · Project start date: 6/24/2025 · Project end date: 12/15/2025 · Expected graduation date:1/15 /2026 |
|||||
| SMART Project Goal: Synthesize your SMART answers from above into a statement that includes specific, measurable, and time-bound elements. | ||||||
| To reduce patient falls during shift changes in the acute care unit by 15% within six months by implementing bedside reporting during shift handoffs. | ||||||
|
||||||
| KPI # 2
|
· At least 95% of nursing staff will complete the bedside reporting training by 8/10 2025.
o Participation will be tracked through attendance sheets and signed policy acknowledgments. o This ensures staff readiness for implementing bedside reporting to reduce falls. |
|||||
Appendix B
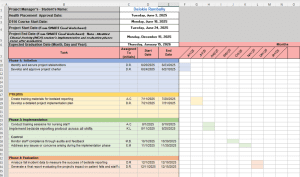
Screenshot of the Gantt Chart (D156)
ORDER A PLAGIARISM-FREE PAPER HERE
We’ll write everything from scratch
Question
IYM3 Task 1: Healthcare Improvement Project
Business Case Analysis for Healthcare Improvement — D156
PRFA — IYM3
PreparationTask OverviewSubmissionsEvaluation Report
Competencies
7073.2.1 : Examine Requirements
The learner examines regulatory and compliance requirements for implementing an improvement project comprising systematic activities and processes that are organized and implemented to improve organizational quality, safety, and performance.
7073.2.2 : Collaborate with Stakeholders
The learner collaborates with internal and external stakeholders to assess the need and organizational readiness for a healthcare improvement project using improvement science methods and practices.
7073.2.3 : Describe the Project Management Life Cycle
The learner describes the four phases of the project management lifecycle that will guide their healthcare improvement project successfully from initiation to closure.
7073.2.4 : Synthesize Data
The learner synthesizes relevant evidence, feasibility results, patient preferences, and interdisciplinary stakeholder perspectives to initiate a healthcare improvement project.
Introduction
Note: You must have completed and passed the performance assessments for D155: Leading with Personal Mastery IOM1 Tasks 1 and 2 prior to beginning this performance assessment.
Note: You must have completed and passed the CPE record and CPE e-portfolio for D156 prior to beginning this performance assessment.
All specialty courses in the Leadership and Management program will have an authentic performance assessment that scaffolds the tasks of the healthcare improvement project (HIP) through the project management lifecycle phases of project initiation, planning, implementation, and evaluation. Each performance assessment will focus on aspects of the proposal you will develop for a healthcare improvement project using a real-world approach to improving healthcare. You will describe each phase of the project management lifecycle in the corresponding sections of the attached “HIP Paper Template.”
This task is focused on initiating the proposed HIP using information from a former or current organization. You will describe the collaborative process used to complete the business case analysis. You will also determine the need, feasibility, and organizational readiness for your HIP using a needs assessment tool, the SWOT analysis, and impact analysis.
As the project manager developing the business case analysis in this initiation phase, your end goal is to justify the project. To help justify your project. you will place your proposed HIP in the context of the literature and provide evidence to support it. In the “Review of Relevant Scholarly Sources” section of your paper, you will discuss key articles that provide the best practices you identified for your project.
You must include scholarly sources published within the last five years that are credible and relevant to your HIP.
This task requires the submission of the provided “D156 HIP Paper Template”, including the following sections of your HIP paper, which you will be developing in this performance assessment:
- Healthcare Improvement Project: Introduction and Project Initiation
o Organizational Problem
o Stakeholders
o Project Team
o Needs Assessment
o SWOT Analysis
o Impact Analysis
o Justification and Project Purpose
o Review of Relevant Scholarly Sources
o Project Environment
o SMART Goal
o Project Management Lifecycle
The following templates should be completed and submitted as appendices to your provided HIP paper template:
- SMART Goal Worksheet (Appendix A)
- Gantt Chart (Appendix B)
During your clinical practice experience (CPE), you identified project stakeholders and project team members (e.g., subject matter experts, colleagues from a former or current organization, faculty, other nursing professionals) who agreed to collaborate with you during this phase of your project. Also during your CPE you consulted with appropriate stakeholders and/or project team members to complete and submit the “Needs Assessment Template,” “SWOT Analysis Template,” and “Impact Analysis Template.” These deliverables were evaluated in your CPE for completion, not quality or content. Your CPE provided you an opportunity to practice and improve these items without including them in your performance assessment.
Falls Prevention in the Acute Care Healthcare Improvement Project
Scenario
There is no scenario required for this task.
Requirements
Your submission must represent your original work and understanding of the course material. Most performance assessment submissions are automatically scanned through the WGU similarity checker. Students are strongly encouraged to wait for the similarity report to generate after uploading their work and then review it to ensure Academic Authenticity guidelines are met before submitting the file for evaluation. See Understanding Similarity Reports for more information.
Grammarly Note:
Professional Communication will be automatically assessed through Grammarly for Education in most performance assessments before a student submits work for evaluation. Students are strongly encouraged to review the Grammarly for Education feedback prior to submitting work for evaluation, as the overall submission will not pass without this aspect passing. See Use Grammarly for Education Effectively for more information.
Microsoft Files Note:
Write your paper in Microsoft Word (.doc or .docx) unless another Microsoft product, or pdf, is specified in the task directions. Tasks may not be submitted as cloud links, such as links to Google Docs, Google Slides, OneDrive, etc. All supporting documentation, such as screenshots and proof of experience, should be collected in a pdf file and submitted separately from the main file. For more information, please see Computer System and Technology Requirements.
You must use the rubric to direct the creation of your submission because it provides detailed criteria that will be used to evaluate your work. Each requirement below may be evaluated by more than one rubric aspect. The rubric aspect titles may contain hyperlinks to relevant portions of the course.
Organizational Problem
- Describe the problem that you plan to address with your healthcare improvement project (HIP).
- Describe the background of your organization that is causing the problem.
Stakeholders
- Describe the influence, interest, and power within your stakeholder group related to implementing your HIP.
Note: Do not include the actual names of people.
Project Team
- Describe twoof your roles and two of your responsibilities as the project manager of your HIP.
- Describe twoskills you possess as the project manager that demonstrate leadership related to your HIP.
- Describe tworoles and tworesponsibilities of one additional project team member who will support a solution to the problem described in part A.
Needs Assessment
- Describe the “Needs Assessment Template” that you completed during your CPE by doing the following:
- Identify which tool you used from the following list:
- five whys
- cause and effect diagram (fishbone)
- failure modes and effect analysis (FMEA)
- affinity analysis
- Describe how the stakeholders and/or project team members discussed and identified themes related to the problem from part A.
- Describe twofindings related to the problem from part A that were identified by the stakeholders and/or project team members during the development of your needs assessment.
SWOT Analysis
- Based on the “SWOT Analysis Template” that you completed during your CPE, complete the following:
- Identify twoweaknesses and twothreats.
- Describe how you plan to mitigate eachof the weaknesses and threats.
- Identify twostrengths and twoopportunities.
- Describe how you plan to maximize eachof the strengths and opportunities.
Impact Analysis
- Provide your total benefit score and total risk score from the “Impact Analysis Template” that you completed during your CPE. Then identify the impact ratio.
- Describe the benefits and risks to the organization based on the impact ratio.
Justification and Project Purpose
- Explain the purpose of your HIP.
- Describe how your HIP addresses the problem you identified in part A.
- Summarize your findings from the needs assessment, SWOT analysis, and impact analysis to justify your HIP.
Review of Relevant Scholarly Sources to Support the Solution to the Identified Problem (Best Practices from the Literature)
- Synthesize fiverelevant scholarly sources in a narrative format, published within the last fiveyears, that can be used to support solutions to the identified problem.
Note: Citations and references are required for each source used.
- Discuss twobest practices identified in your review of the literature that support your planned solution to the problem.
Project Environment
- Describe onepolicy, procedure, or guideline and how it impacts the implementation of your project.
Note: You may use policies, procedures, or guidelines from appropriate organizations such as IHI, AAP, CDC, CMS, The Joint Commission, AHRQ, a local organization, etc.
SMART Goal
- Complete the “SMART Goal Worksheet” section (Appendix A of the attached “HIP Paper Template”) by doing the following:
- Complete eachof the SMART questions on the “SMART Goal Worksheet.”
- Identify oneSMART project goal for the project on the “SMART Goal Worksheet.”
- Identify twoprocess KPIs that you will use to determine progress toward your goal.
- Describe how you gathered stakeholder and/or project team member perspectives and synthesized those into your SMART goal.
Project Management Life Cycle
- Explain the four phases of the project management lifecycle in terms of your HIP by doing the following:
- Describe the fourproject management lifecycle phases that will guide your project.
- Create a Gantt Chart (use the attached “Gantt Chart template”) and submit a clearly visible screenshot of it as Appendix B of the attached “HIP Paper Template”, including each of the following components:
o your CLPS clearance date
o your D156 course start date
o your project start date
o your project end date
o your planned graduation date
o each of the four project lifecycle phases (initiation, planning, implementation, and evaluation)
o at least two tasks or deliverables that have been completed in the initiation phase
o at least one task or deliverable that will be completed in each of the remaining phases (planning, implementation, and evaluation)
o the start and end dates associated with each of the tasks or deliverables
o a bar chart for each of the tasks or deliverables representing the duration of each task
o the stakeholder initials to whom each task or deliverable is assigned
o aligned Gantt chart initiation start date with your SMART goal worksheet project start date
o aligned Gantt chart evaluation or closure end date with your SMART goal end dat
- Acknowledge sources, using in-text citations and references, for content that is quoted, paraphrased, or summarized.
- Demonstrate professional communication in the content and presentation of your submission.
File Restrictions
File name may contain only letters, numbers, spaces, and these symbols: ! – _ . * ‘ ( )
File size limit: 200 MB
File types allowed: doc, docx, rtf, xls, xlsx, ppt, pptx, odt, pdf, csv, txt, qt, mov, mpg, avi, mp3, wav, mp4, wma, flv, asf, mpeg, wmv, m4v, svg, tif, tiff, jpeg, jpg, gif, png, zip, rar, tar, 7z